The Brugada-like Electrocardiogram (ECG) pattern is a transient condition which may be induced by number of conditions. In this case reported, a 53-year-old Iranian male patient, presented with seven-day history of fever, chills, headache and shortness of breath. At the time of presentation to the Emergency Department (ED), the patient was febrile with tachycardia, tachypnea, and oxygen (O2) saturation 75%. The chest radiograph showed a bilateral infiltration and positive result of Real Time Polymerase Chain Reaction (RT-PCR) confirmed the diagnosis of COVID-19 infection. He received kaletra, hydroxychloroquine, azithromycin, antibiotics, and Intravenous Immunoglobulin (IVIG). The patients was intubated and underwent mechanical ventilation because of no improvement on the O2 saturation level. Fever subsided on seventh day and hydroxychloroquine was stopped on fifth day. On the sixth day of hospital stay, ECG showed sinus tachycardia. Troponin-I- high sensitive was within normal range and Transthoracic Echocardiography (TTE) showed normal Ejection Fraction (EF). On 10th day, type I Brugada-ECG pattern presented and regular ECG monitoring was recommended. Finally, after 11-day hospital stay, the patient died due to bradycardia and asystole despite Cardiopulmonary Resuscitation (CPR). Thus, physicians should consider Brugada-ECG pattern in the pre-cordial leads (V1 to V3) of ECG among patients with COVID-19 infection beside regular QT interval monitoring.
Corona virus disease-2019, Electrocardiography, Fever, Hydroxychloroquine, Sinus tachycardia
Case Report
A 53-year-old Iranian man presented to the ED with a seven-day history of fever, chills, headache and shortness of breath. Upon presentation to the ED, the patient was febrile (temperature 38.8°C) with tachycardia (pulse 148 beats per minute) and tachypnea (respiratory rate 27 breaths per minute). The blood pressure was 115/66 mm Hg and the oxygen (O2) saturation was 75% while he was breathing the ambient air. He reported no history of medications, allergies, syncope and no family history of Sudden Cardiac Death (SCD). He denied recent travel or sick contacts.
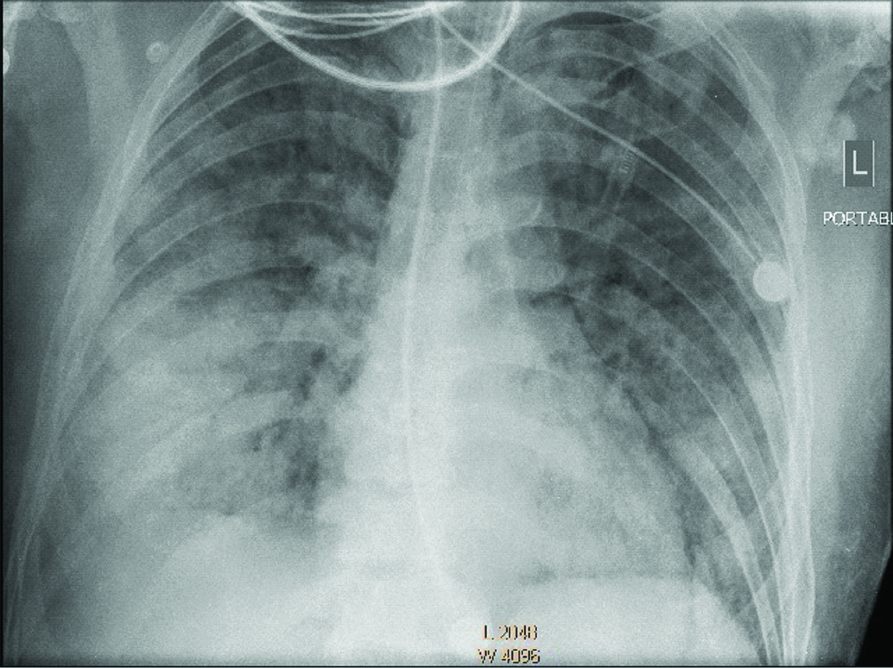
While being admitted to the ED, all droplet and contact precautions were also considered suspecting COVID-19. During the patient’s physical examination, generalised coarse rales sound was heard in the both lungs, while heart sounds were normal. Laboratory data indicated leukocytosis, anaemia, thrombocytopenia, neutropenia, lymphopenia, positive C-reactive protein, hyponatremia, elevated Blood Urea Nitrogen (BUN) and creatinine, elevated Aspartate Aminotransferase (AST), hypoalbuminemia, elevated Lactate Dehydrogenase (LDH) and longer Prothrombin Time (PT) [Table/Fig-1]. The portable chest radiograph showed a bilateral infiltration [Table/Fig-2]. Since the clinical presentations and findings on the laboratory tests and chest radiography were consistent with COVID-19, supportive care such as Intravenous (IV) fluid therapy, oxygen therapy with the nasal cannula, and antipyretic treatment was implemented.
Clinical laboratory results.
| Variable | Report | Normal range |
|---|
| Haematology |
| White cell count (×1000/μL) | 14.9* | 4.5-11 |
| Haemoglobin (g/dL) | 13.0† | 13.5-17.5 |
| Haematocrit (%) | 38.6† | 41.0-53.0 |
| Platelet count (×1000/mm3) | 115† | 150-450 |
| Absolute Neutrophil count (×1000/μL) | 0.85† | 1.8-7.7 |
| Absolute lymphocyte count (×1000/μL) | 0.12† | 1.1-4.8 |
| High sensitivity cardiac troponin (ng/L) | 10.6 | <19 |
| C-reactive protein (mg/liter) | Positive | Negative |
| Sodium (mEq/l) | 129† | 135.0-148.0 |
| Potassium (mEq/l) | 4.0 | 3.5-5.5 |
| Blood urea nitrogen (mg/dL) | 21.0* | 7.9-20 |
| Creatinine (mg/dL) | 1.74* | 0.7-1.4 |
| blood glucose (mg/dL) | 116 | 70-140 |
| Calcium (mg/dL) | 8.6 | 8.4-10.2 |
| Phosphorus (mg/dL) | 2.6 | 2.6-4.5 |
| Aspartate aminotransferase (U/L) | 173* | 5.0-40.0 |
| Alanine aminotransferase (U/L) | 30.0 | <40 |
| Albumin (g/dL) | 2.8† | 3.4-5.4 |
| Alkaline phosphate (IU/L) | 211.0 | 80.0-306.0 |
| Lactate dehydrogenase serum (IU/L) | 1772.0* | Up to 480 |
| Prothrombin time (patient) (second) | 15* | 11.0-13.5 |
| Prothrombin time (control) (second) | 13 | 11.0-13.5 |
| INR | 1.24 | ≤1.1 |
| Partial thromboplastin time (patient) (second) | 58 | 60-70 |
*The value in the patient was above the normal interval
†The value in the patient was below the normal interval
INR: International normalised ratio
Portable chest radiograph showing a bilateral infiltration (anteroposterior view).
Moreover, positive result of Real Time-Polymerase Chain Reaction (RT-PCR) from nasal and throat swab was reported and the diagnosis of COVID-19 infection was confirmed. Thus, the patient received medications such as kaletra (lopinavir/ritonavir) (400/100 mg, per oral (PO), twice a day), hydroxychloroquine (200 mg, PO, twice a day), azithromycin (500 mg on a day one, then 250 mg on day 2-5, PO), meropenem (2 g, IV, twice a day), vancomycin (1 g, IV, once a day) and IVIG (20 g, once a day). On the second day of admission, due to no improvement on the O2 saturation following O2 therapy with nasal cannula (O2 saturation 79%), the patient was intubated, transferred to a dedicated COVID-19 Intensive Care Unit (ICU) and underwent mechanical ventilation.
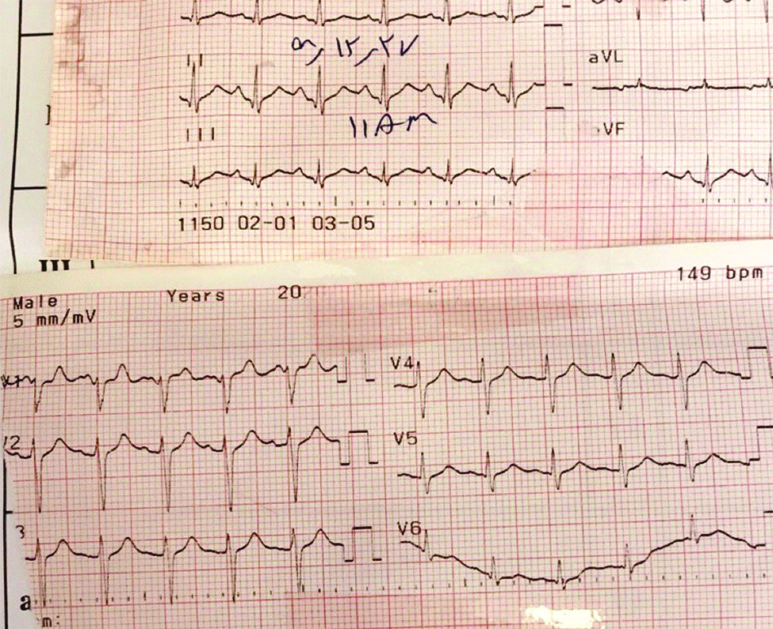
Fever subsided on seventh day and hydrochloroquine was stopped on fitth day. While, O2 saturation dropped from 79% to 63%. On the sixth day of hospital stay, routine ECG monitoring in the Intensive Care Unit (ICU) showed a sinus tachycardia opposite normal sinus rhythm at baseline [Table/Fig-3]. High-sensitivity Cardiac Troponin was in the normal range [Table/Fig-1] and bedside TTE indicated normal EF with no anatomic abnormalities and pericardial effusion.
Electrocardiogram demonstrating sinus tachycardia.
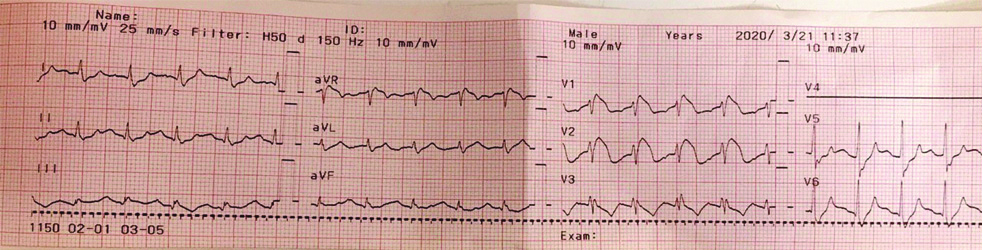
On 10th day, type I Brugada-ECG pattern (coved type ST- segment elevation and T wave inversion in precordial lead V1 and V2) presented in the ECG [Table/Fig-4]. Therefore, consultation by an electrophysiologist was requested and because of low risk stratification, the regular ECG monitoring of the patient was recommended. Finally, after eleven-day hospital stay, bradycardia and asystole occurred and the patient died despite CPR.
Electrocardiogram demonstrating Brugada type I pattern.
Discussion
In this case, type I Brugada-ECG pattern in an Iranian male patient with COVID-19 infection was presented. Brugada syndrome was firstly described in 1992 [1] with a heritable clinical entity which characterised by life-threatening arrhythmias in patients without structural heart disease and by an ECG pattern including coved-type ST- segment elevation in one or more precordial leads V1 to V3 (Brugada type I ECG pattern). Although a “Brugada syndrome” in its asymptomatic phase may be considered in the presence of a “Brugada type I ECG pattern” [2], they should not be used interchangeably
The Brugada-like ECG pattern is a transient condition and may be induced by number of conditions such as fever, hyperkalemia, hypokalemia, hypercalcaemia, cocaine abuse, and number of medications such as sodium channel blockers, heterocyclic antidepressants, and beta-adrenergic blockers [3]. Acute cardiac injury, acute coronary event, left ventricular systolic dysfunction, heart failure, and arrhythmia have been all described as cardiovascular complications in coronavirus disease 2019 [4].
Until now, COVID-19 has been reported to be the 13th major cause of death [5]. There is no proven effective treatment against the virus, and the impact on other conditions is also unknown. In addition, arrhythmogenic effect of COVID-19 infection on heart, either secondary to acquired conditions or co-morbidities or consequence of inherited syndromes, can be expected [6].
Recently, it has been reported that COVID-19 infection can unmask Brugada syndrome [7,8] and can also lead to Brugada-ECG pattern [9,10]. Febrile conditions can induce the Brugada-ECG pattern and trigger arrhythmias [11] and fever has been reported as the most common symptom of COVID-19 [12]. Due to febrile condition of COVID-19 infection, it has been reported as another etiology of such pattern. While, fever-induced Brugada is not a new finding [13], previous cases attributed the Brugada syndrome and Brugada-ECG pattern to febrile condition of COVID-19 infection [7,9].
It can be induced by any condition predisposing to fever rather than COVID-19 infection [13] and it may be due to the medical management of COVID-19 too. In other words, combination of hydroxychloroquine sulfate with antiviral drugs such as Lopinavir or antibiotics such as azithromycin in the treatment of COVID-19 may induce arrhythmias such as QT-prolongation [14,15]. However, patient in the present study presented type I Brugada-ECG pattern rather than QT prolongation.
Conclusion(s)
Brugada-ECG pattern may present due to the infection with COVID-19 or its febrile condition, or its medical management with hydroxychloroquine sulfate combined with antiviral treatment and antibiotics. Thus, physicians should consider Brugada-ECG pattern in the pre-cordial leads (V1 to V3) of ECG among patients with COVID-19 infection beside regular QT interval monitoring.
*The value in the patient was above the normal interval
†The value in the patient was below the normal interval
INR: International normalised ratio
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? No
For any images presented appropriate consent has been obtained from the subjects. No
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Sep 05, 2020
Manual Googling: Oct 20, 2020
iThenticate Software: Oct 30, 2020 (8%)
[1]. Brugada P, Brugada J, Right bundle branch block, persistent ST segment elevation and sudden cardiac death: A distinct clinical and electrocardiographic syndrome: A multicenter reportJournal of the American College of Cardiology 1992 20(6):1391-96.10.1016/0735-1097(92)90253-J [Google Scholar] [CrossRef]
[2]. Delise P, Probst V, Allocca G, Sitta N, Sciarra L, Brugada J, Clinical outcome of patients with the Brugada type 1 electrocardiogram without prophylactic implantable cardioverter defibrillator in primary prevention: A cumulative analysis of seven large prospective studiesEP Europace 2018 20(FI1):f77-85.10.1093/europace/eux22629036426 [Google Scholar] [CrossRef] [PubMed]
[3]. Antzelevitch C, Brugada P, Brugada J, Brugada R, Brugada syndrome: From cell to bedsideCurrent Problems in Cardiology 2005 30(1):09-54.10.1016/j.cpcardiol.2004.04.00515627121 [Google Scholar] [CrossRef] [PubMed]
[4]. Bansal M, Cardiovascular disease and COVID-19Diabetes & Metabolic Syndrome: Clinical Research & Reviews 2020 14(3):247-50.10.1016/j.dsx.2020.03.01332247212 [Google Scholar] [CrossRef] [PubMed]
[5]. Poorolajal J, Neglected major causes of death much deadlier than COVID-19Journal of Research in Health Sciences 2020 20(2):e0047810.34172/jrhs.2020.1332814695 [Google Scholar] [CrossRef] [PubMed]
[6]. Wu CI, Postema PG, Arbelo E, Behr ER, Bezzina CR, Napolitano C, SARS-CoV-2, COVID-19, and inherited arrhythmia syndromesHeart Rhythm 2020 17(9):1456-62.10.1016/j.hrthm.2020.03.02432244059 [Google Scholar] [CrossRef] [PubMed]
[7]. Chang D, Saleh M, Garcia-Bengo Y, Choi E, Epstein L, Willner J, COVID-19 Infection Unmasking Brugada SyndromeHeartRhythm Case Rep 2020 6(5):237-40.10.1016/j.hrcr.2020.03.01232292696 [Google Scholar] [CrossRef] [PubMed]
[8]. Pasquetto G, Conti GB, Susana A, Leone LA, Bertaglia E, Syncope, Brugada syndrome, and COVID-19 lung diseaseJournal of Arrhythmia 2020 36(4):768-70.10.1002/joa3.1237532778849 [Google Scholar] [CrossRef] [PubMed]
[9]. Vidovich MI, Transient Brugada-Like Electrocardiographic Pattern in a Patient With COVID-19JACC: Case Reports 2020 2(9):1245-49.10.1016/j.jaccas.2020.04.00732309815 [Google Scholar] [CrossRef] [PubMed]
[10]. van de Poll S, van der Werf C, Two patients with COVID-19 and a fever-induced Brugada-like electrocardiographic patternNeth Heart J 2020 28(7-8):431-36.10.1007/s12471-020-01459-132643073 [Google Scholar] [CrossRef] [PubMed]
[11]. Amin AS, Meregalli PG, Bardai A, Wilde AA, Tan HL, Fever increases the risk for cardiac arrest in the Brugada syndromeAnnals of Internal Medicine 2008 149(3):216-17.10.7326/0003-4819-149-3-200808050-0002018678856 [Google Scholar] [CrossRef] [PubMed]
[12]. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Clinical characteristics of Coronavirus Disease 2019 in ChinaNew England Journal of Medicine 2020 382(18):1708-20.10.1056/NEJMoa200203232109013 [Google Scholar] [CrossRef] [PubMed]
[13]. Betancor IH, Garduño JAO, Prera RAJ, Ojeda FB, To the Editor-Is it really COVID-19?Heart Rhythm Case Rep 2020 6(7):P47110.1016/j.hrcr.2020.04.02032373463 [Google Scholar] [CrossRef] [PubMed]
[14]. Choi Y, Lim HS, Chung D, Choi JG, Yoon D, Risk evaluation of Azithromycin-Induced QT prolongation in real-world practiceBio Med research international 2018 2018:1574806https://doi.org/10.1155/2018/157480610.1155/2018/157480630406128 [Google Scholar] [CrossRef] [PubMed]
[15]. Yang Z, Prinsen JK, Bersell KR, Shen W, Yermalitskaya L, Sidorova T, Azithromycin causes a novel proarrhythmic syndromeCirculation: Arrhythmia and Electrophysiology 2017 10(4):e00356010.1161/CIRCEP.115.003560 [Google Scholar] [CrossRef]