The World Health Organisation (WHO) suggests only a limited number of antibiotics with good intracellular access and confirmed clinical effectiveness for the treatment of brucellosis [6]. The present study evaluated eight years’ experience with brucellosis in a tertiary care teaching hospital in Kerala, India focusing on the clinical findings, occupational history, laboratory parameters, treatment and outcome of the patients.
Materials and Methods
A retrospective observational study was conducted in Jubilee Mission Medical College, Thrissur, a Tertiary Care Teaching Hospital in central Kerala, India including all patients with a positive culture for Brucella melitensis during a period of eight years (1/6/2011 to 31/5/2019). Identification of these isolates was done by Vitek 2 compact system (BioMerieux, India Ltd.,). The clinical records of culture proven brucellosis cases were analysed six monthly every year from medical records library for collecting data regarding the demographic characteristics such as age, gender, residency, exposure history, clinical spectrum of infection, antibiotic therapy and outcome of the patients. The follow-up was done with the help of the contact details (telephone numbers) available in the clinical records of the patient after discharge from the hospital. The mean follow-up period was of six months.
Definitions used
Relapse: Reappearance of the symptoms after initial improvement followed by treatment within a month after the end of the prescribed regimen [7].
Cure: No recurrence of symptoms and signs during the six-month follow-up period [7].
Statistical Analysis
After coding, data was entered and analysed in Microsoft Excel version 10 and percentages were calculated for different parameters.
Results
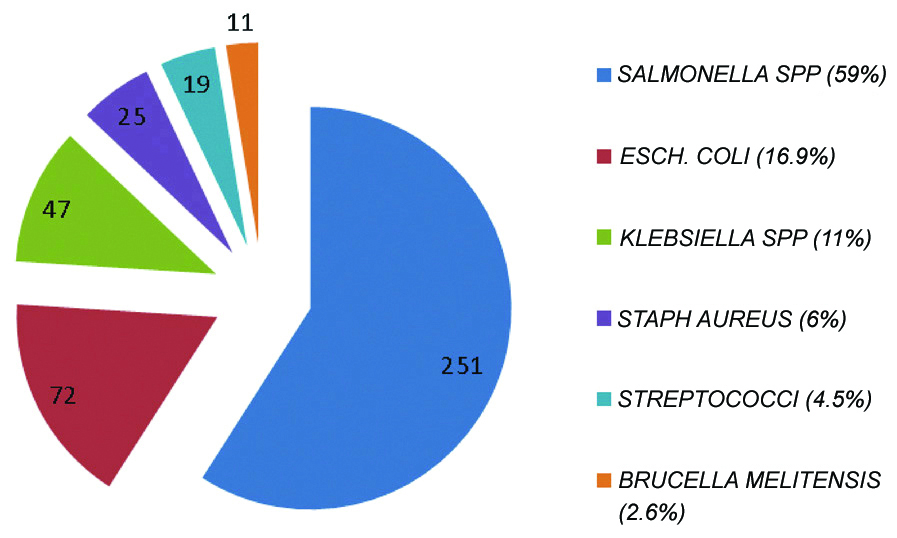
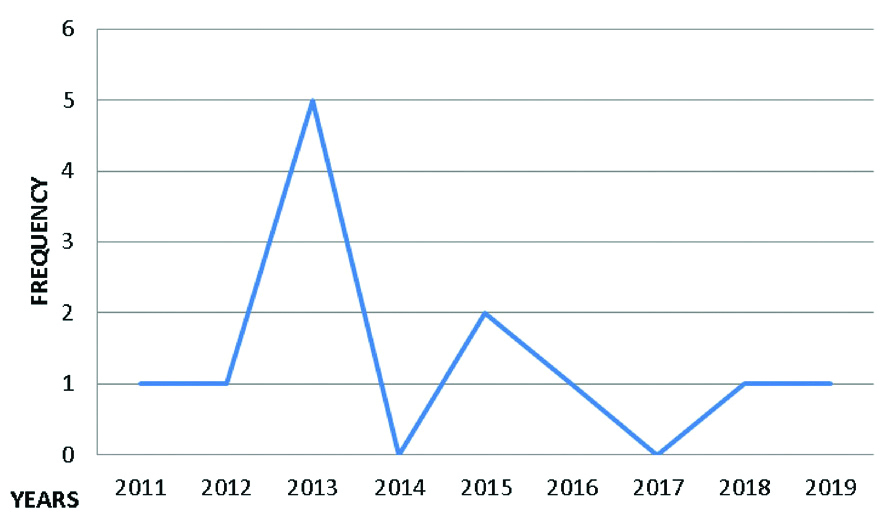
Twelve cases of Brucella melitensis were reported from the Department of Microbiology, Jubilee Mission Medical College, Thrissur, Kerala, India during this eight year period. Eleven of them were PUO cases (from non-repetitive blood samples) and one a soft tissue infection case (breast abscess). A total of 52880 blood samples were processed in Microbiology Department over a span of eight years and among which 5182 (9.8%) blood cultures were from patients suspecting PUO. Blood culture positivity rate of the laboratory was 8.2% (425). The organisms isolated from blood culture are detailed in [Table/Fig-1]. The annual distribution of Brucella cases are summarised in [Table/Fig-2].
Details of blood culture isolates.
Annual distribution of Brucella cases.
Demographic and exposure details of these 12 positive cases were collected. Distribution of cases based on districts of residence, Middle-east countries associated and departments in which patients got admitted is shown in [Table/Fig-3]. Presumed types of exposure of all the patients to the agent as per the history were outlined in [Table/Fig-4]. Out of 12 patients, nine (75%) were males and three were (25%) females with an age ranging from 25-57 years (mean age 37 years).
Demographic characteristics.
| Frequency | Percentage |
|---|
| Sex distribution |
| Male | 9 | 75 |
| Female | 3 | 25 |
| District wise case distribution |
| Palakkad | 6 | 50 |
| Thrissur | 5 | 41.7 |
| Malappuram | 1 | 8.3 |
| Distribution of imported cases (n=9) |
| Saudi Arabia | 6 | 66.7 |
| Sharjah | 1 | 11.1 |
| Oman | 1 | 11.1 |
| Abudubai | 1 | 11.1 |
| Admitted medical specialities |
| Medicine | 10 | 83.34 |
| Surgery | 1 | 8.3 |
| Orthopaedics | 1 | 8.3 |
Mode of transmission of Brucella spp among cases.
| Type of exposure | Frequency | Percentage |
|---|
| Consumption of unpasteurised milk products or contact with animals | 11 | 91.7 |
| Other (close personal contact) | 1 | 8.3 |
The severity of symptoms varied from mild illness to severe painful localised disease. Most of the cases (11/12) presented to the hospital after several weeks of mild non-specific complaints. Only one case presented as a localised painful lesion in the soft tissue. The illness duration prior to diagnosis ranged from seven to 120 days. All the patients gave history of fever and malaise. History of all culture proven Brucella spp patients were thoroughly taken with an emphasis on type of exposure they probably had to get the infection. Various clinical presentations and laboratory parameters of the 12 cases are summarised in [Table/Fig-5].
Clinical presentations and laboratory parameters of the brucellosis cases.
| Number of patients | Percentage |
|---|
| Symptoms |
| Fever | 12 | 100 |
| Malaise | 12 | 100 |
| Lower back pain and arthralgia | 10 | 83 |
| Gastrointestinal symptoms like vomiting, diarrhoea | 4 | 33 |
| Evening rise of temperature, weight loss, headache | 3 | 25 |
| Clinical findings |
| Hepatosplenomegaly | 5 | 41.7 |
| Lymphadenopathy | 4 | 33.3 |
| Splenomegaly alone | 3 | 25 |
| Osteo-articular involvement | 1 | 8.3 |
| Breast abscess | 1 | 8.3 |
| Endocarditis | 1 | 8.3 |
| Deranged laboratory parameters |
| Anaemia | 8 | 66.6 |
| Elevated erythrocyte sedimentation rate | 7 | 58.3 |
| Elevated liver enzymes | 7 | 58.3 |
| Thrombocytopenia | 5 | 41.7 |
| Leucopenia | 1 | 8.3 |
Blood samples of all the 11 PUO cases were indicated positive by automated blood culture system (BacT/Alert, BioMerieux India Ltd.,) in a mean detection time of three days. Blood and pus aspirate samples, on subculture yielded small greyish white non-haemolytic oxidase positive, urease positive, Gram negative cocco bacilli which were identified as Brucella melitensis by Vitek 2 compact system.
All the cases received doxycycline for minimum of six weeks. The treatment strategy followed is explained in [Table/Fig-6]. Two cases were lost to follow-up (including one endocarditis case and the other case of PUO) for which complete treatment history could not be traced. There was no death or relapses noted during six month follow-up.
Details of brucellosis treatment regimens followed.
| Antibiotics | Frequency (N=10) | Percentage |
|---|
| Doxycycline 100 mg BD for 6 weeks plusGentamycin 120 mg IV OD for 10 days | 5 | 41.7 |
| Doxycycline 100 mg BD for 6 weeks plusStreptomycin 1 g IM OD for 2 weeks | 3 | 25 |
| Doxycycline 100 mg BD for 6 weeks plusRifampicin 600 mg/Day for 6 weeks | 2 | 16.6 |
(n=2 lost to follow up)
Discussion
Brucellosis is a zoonotic infection worldwide with more than 500,000 new cases annually with prevalence rate in some countries exceeds 10 cases per 100,000 population [1]. Brucella is classified as a Class B Bioterrorist agent [8] and its recent re-emergence had led to a renewed scientific interest in human brucellosis. B. melitensis is prevalent in Southeast Asian countries including India and mostly responsible for human brucellosis [5]. In many developing countries, brucellosis is endemic but remains under-diagnosed and under-reported because of its masquerading capability. Whether ingestion of contaminated dairy products or contact with infected animals has occurred is to be specially looked for. Detailed history taking from the patients is crucial especially in urban and non-endemic areas, and in cases of imported Brucella, in which travellers acquire the disease abroad and become ill in non-endemic settings [8]. In humans, the symptoms presents in majority of brucellosis cases are weight loss, undulant fever and night sweats. In endemic areas, it is one of the important causes of PUO and the reason for fever of prolonged duration [9]. Brucellosis results in mild chronic disease so that the diagnosis of the disease is difficult. In this study majority of cases (11/12) were diagnosed as PUOs. Some uncommon presentations of brucellosis include cutaneous and soft tissue lesions. In the present study, also there was a case of brucellosis with soft tissue infection presenting as breast abscess. An extremely rare manifestation of brucellosis in humans is Breast involvement but in animals it is common [10]. Based on a case series of brucellosis by Andriopoulos P et al, the reported prevalence of human brucellosis presenting as breast abscess is 0.7% [7].
The Middle-east countries are regarded as endemic for brucellosis. Analysing the demographic and occupational data in this study, it was found that 75% of the cases had a direct association with the Middle East countries in the form of occupational exposure or by ingestion of unpasteurised dairy products from there. A literature review of 505 imported cases of brucellosis including immigrants and foreign travellers illustrated that most imported cases were associated with travel and/or consumption of unpasteurised dairy products in or from endemic countries [11]. Brucella may enter the body through the gastrointestinal tract, the lungs or respiratory mucosal layers and spread through the blood and the lymphatic system to any other organ. Fresh milk and dairy products prepared from unpasteurised milk such as soft cheese, yoghurts and ice-creams may contain high amounts of the bacteria and consumption of these is an important cause of human brucellosis [12]. In the present study also, 91.7% of the brucellosis cases had given a history of consumption of unpasteurised milk in the form of fresh milk or milk shakes. In another study by Andriopoulos P et al., 84% of Brucella cases were by food borne transmission [7]. Thus, the main mode of brucellosis transmission is presumed to be through gastrointestinal route [13]. In this study, there was one case of human to human transmission of brucellosis probably sexually transmitted, where spouse of a brucellosis patient developed breast abscess. She presented with clinical features of breast abscess two months after the onset of her husband’s disease. The chance of the lady acquiring disease from her husband is high as the appearance of disease falls in the incubation period. In cases of brucellosis in humans, genitourinary complications such as prostatitis and epididymo-orchitis are seen and seeding of these organs could perhaps involve in the disease transmission from person to person which is extremely rare [14]. The mean age of the patients with brucellosis in this study was 37 years (ranging from 25-57 years) with a male preponderance (75%). Although brucellosis affects all age groups, in this study, young adults were more commonly found to be affected. The clinical expression of brucellosis, including the frequency and type of signs, symptoms and complications are influence by the age distribution of the study population [15]. A similar observation has been made by Patil DP et al., where the mean age of the patients was 31 years and 72.2% were males [16]. Consistent with this result, the majority of studies had a male preponderance [13]. Sex distribution of patients with brucellosis varies widely- There are studies showing either equal distribution [17] or, even predominance of female patients [18].
According to the duration of symptoms, cases of brucellosis are classified arbitrarily as “acute” (less than eight weeks), “sub-acute” (from eight to 52 weeks), and chronic (more than 52 weeks). Acute brucellosis may progress to a more persistent disease with localised infections or a non-specific syndrome sometimes referred to as ‘chronic fatigue syndrome’ [16]. Complications observed can be very diverse including osteo-articular, gastrointestinal, hepato-biliary, respiratory or genitourinary [12]. In this study, acute and sub-acute type of presentations was commonly seen than the chronic type. The median illness duration prior to diagnosis was 47 days (range from seven to 120 days). Brucellosis duration prior to diagnosis is an important parameter, because it is directly correlated with the complication rate and unfavourable outcome [15]. Human brucellosis is considered as one of the “great imitators” because of its wide spectrum of clinical manifestations. The clinical features of brucellosis depend on the stage of the disease as well as the organs and systems involved [8]. In this study, fever and malaise (100%) were the predominant symptoms reported by the patients followed by low backache and arthralgia (83%) which was similar to that reported in previous literature [8,12]. Brucella spp after entering the gastrointestinal tract (most common route) localises the reticulo-endothelial system. According to Patil DP et al., the liver being the largest organ of reticulo-endothelial system is frequently affected resulting in hepatomegaly which is present in 32-63% of cases. The incidence of splenomegaly ranges from 29 and 56.6% of the cases. Anorexia, vomiting, diarrhea and constipation are other non-specific gastrointestinal manifestations of brucellosis [16]. In the present study hepatosplenomegaly (41.7%) was the most common clinical finding seen in the patients followed by lymphadenopathy (33.3%) and osteo-articular involvement (lumbosacral region) (8.3%). According to Andriopoulos P et al., splenomegaly (51%), osteo-articular involvement (42%), lymphadenopathy (31%) and hepatomegaly (25%) constituted the common clinical findings [7].
Mild haematologic abnormalities such as anaemia and leukopenia are associated with Brucella infection commonly [7]. In a case series by Dilek I et al., the incidence of anaemia, leucopenia and thrombocytopenia has been reported as 44 to 74%, 7.7% to 68% and 5% to 13.7%, respectively [19]. In this study, 66.6% patients had anaemia, 41.7% had thrombocytopenia, 8.3% had leucopenia, 58.3% had elevated liver enzymes and elevated Erythrocyte Sedimentation Rate (ESR). High incidence of anaemia and elevated ESR were also reported by Liu J and Zhao X and also by Sathyanarayanan V et al., [20,21]. The gold standard in diagnosis of brucellosis is identification of isolates from culture [22]. More culture positivity is with acute brucellosis than chronic or localised forms of disease [7]. Brucella is a slow growing bacterium and it may take weeks of incubation in blood culture bottles to get growth. The use of automated blood culture systems has shortened the time needed for detection. In this study, blood samples were incubated in automated machine BacT/ALERT and the bottles were flagged positive in a mean detection time of three days. One study reported a mean detection time of 51.2±8.2 hours using BacT/ALERT standard aerobic bottles [23] where as another group showed the mean detection time between 1.8 and 3.7 days (mean: 2.5 days) [24]. The identification was done by Vitek 2 compact system in present study.
According to WHO, oral doxycycline for six weeks combined with gentamycin or streptomycin during the first two to three weeks of therapy is effective for human brucellosis [6]. Five out of 12 cases (41.7%) were treated successfully with doxycycline in combination with gentamycin, three cases (25%) received doxycycline in combination with streptomycin and two cases (16.6%) were treated with doxycycline in combination with rifampicin. Follow-up details of two cases were lost (including one endocarditis case and the other case of PUO) for which complete treatment history could not be traced. There was no death or relapse noted during the six months follow-up. Brucella endocarditis involving aortic valve is a rare but most serious complication of human brucellosis. Though it was observed in less than two percentage of the brucellosis cases, it is the main cause responsible for up to 80% of infection-related deaths in brucellosis. This condition is conventionally managed by a combined medical and surgical approach. Surgical intervention includes valve replacement with adequate debridement [25]. Brucellosis, remains as a diagnostic puzzle in both endemic and non-endemic regions due to unusual presentations and non-specific symptoms. It is frequently overlooked, misdiagnosed, or diagnosed incidentally; therefore, physicians must be aware of such a treacherous illness and consider brucellosis in their differential diagnosis of febrile diseases with peculiar musculoskeletal or other focal findings.
Limitation(s)
It was primarily associated with challenges inherent to retrospective review of clinical and epidemiological data. As a result, information on the treatment and follow-up were missing for some cases. Health education regarding preventive aspects of the disease including vaccinating the animal reservoirs, consumption of pasteurised milk and milk products, avoiding occupational risk exposures, also could not be emphasised. Brucellosis, remains a diagnostic puzzle in both endemic and non-endemic regions due to unusual presentations and non-specific symptoms. It is frequently overlooked, misdiagnosed, or diagnosed incidentally; therefore, physicians must be aware of such a treacherous illness and consider brucellosis in their differential diagnosis of febrile diseases with peculiar musculoskeletal or other focal findings.
Conclusion(s)
Brucellosis is an infection with multiple presentations, and whether in an endemic region or not, a thorough history of exposure, travel and clinical suspicion are required for early diagnosis of brucellosis and to facilitate prompt therapy that helps in timely management of this infectious disease with a successful outcome.
(n=2 lost to follow up)