A Rare Presentaion of Adrenocortical Carcinoma
Raju Kamlakarrao Shinde1, Sangita Jogdand Shinde2, Shubham Satyaprakash Gupta3, Sajika Pramod Dighe4, Fadi Mohamed Kallam5
1 Professor, Department of Surgery, Datta Meghe Institute of Medical Sciences, DMIMS, Sawangi, Wardha, Maharashtra, India.
2 Professor and Head, Department of Pharmacology, Datta Meghe Institute of Medical Sciences, DMIMS, Sawangi, Wardha, Maharashtra, India.
3 Resident, Department of Surgery, Datta Meghe Institute of Medical Sciences, DMIMS, Sawangi, Wardha, Maharashtra, India.
4 Resident, Department of Surgery, Datta Meghe Institute of Medical Sciences, DMIMS, Sawangi, Wardha, Maharashtra, India.
5 MBBS Student, Datta Meghe Institute of Medical Sciences, DMIMS, Sawangi, Wardha, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Shubham Satyaprakash Gupta, F 18, Yashodabai Hostel, Sawangi Meghe Hospital, Wardha, Maharashtra, India.
E-mail: sg2638@gmail.com
Adrenocortical Carcinoma (ACC) is a rare tumour, with an annual incidence of approximately one per million. Almost all cases occur in patients aged 40 to 50 years, but there is a minor peak in occurrence among children younger than 5 years. It demonstrates no significant gender predilection. At the time of presentation, ACC tend to be very large and have usually spread beyond the confines of the adrenal gland. The presentation of this tumour may vary, either it can present as virilisation or Cushing’s syndrome or both. The authors present their experience of a rare presentation of an asymptomatic ACC with a large size of tumour mass with no metastasis with just complain of burning micturition in a 55-year-old male patient which was difficult to diagnose clinically. The patient is doing well after surgical management.
Computed tomography, Cushing’s syndrome, Radical nephrectomy, Serum cortisol
Case Report
A 55-year-old male patient had complains of burning micturition with acute retention of urine since 15 days. The patient had no history of fever, pain or lump in abdomen, haematuria or polyuria or nocturia, loss of appetite or loss of weight, breathlessness or jaundice. Patient had neither cushingoid features nor any co-morbid conditions (hypertension, diabetes, tuberculosis or bronchial asthma). The patient also had no history of any previous medical or surgical interventions.
On clinical examination, patient was moderately built with no pallor, icterus, cyanosis, clubbing or lymphadenopathy. Abdomen was soft, non-tender, bowel sounds present in all four quadrants with no distension, guarding or rigidity. Patient underwent Ultrasound Sonography test (USG) of abdomen and pelvis which was suggestive of a large lesion in the right adrenal gland with heterogenous enhancement. Differentials considered were; metastasis or ACC. Fat between the lesion and surrounding structure was well-maintained. There was a calculus at right vesico-ureteric junction with resultant proximal mild hydroureter and hydronephrosis with non-obstructive calculus in lower calyx of the right kidney.
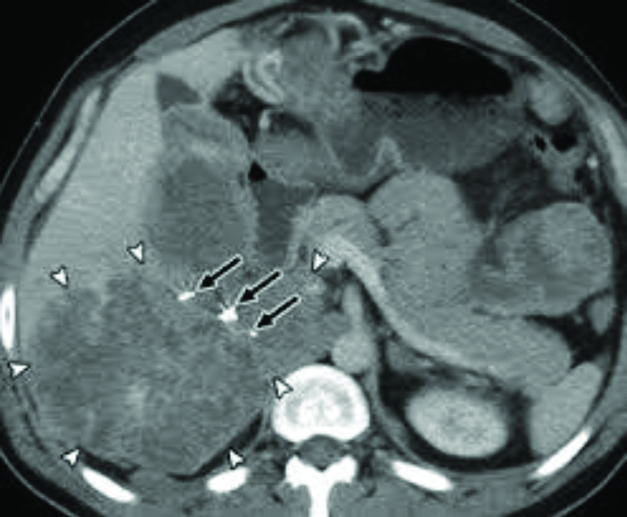
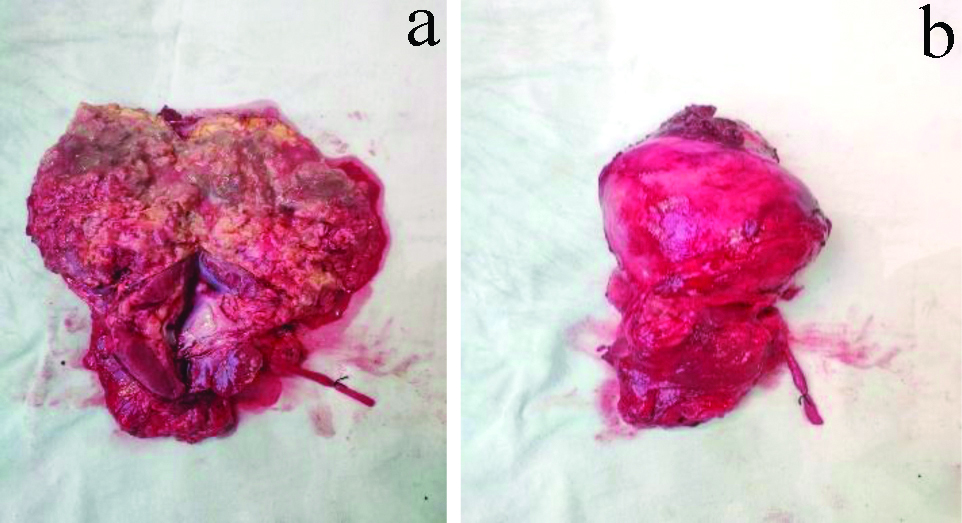
Patient then underwent Contrast-Enhanced Computed Tomography (CECT) abdomen and pelvis which revealed a right sided Vesicoureteric Junction (VUJ) calculus of 5×5 mm in size and an astonishing finding of a large solid cystic lesion of size 12×9.5×10 cm in the right adrenal gland with heterogeneous enhancement [Table/Fig-1]. It showed mild vascularity on doppler and compressed kidney downward and also inferior surface of liver parenchyma which was suspicious of adrenocortical tumour. Fat plane between the lesion and the surrounding structures were well-maintained. Blood Investigations reports were as follows: Serum Cortisol (8 AM) 17.2 μg/dL; Serum Cortisol 6.17 μg/dL; Serum Dehydroepiandrosterone Sulfate (DHEAS) 7200 μg/mL; Urine Metanephrines 220 μg/24 hours. Hence, the patient was provisionally diagnosed with ACC with subclinical Cushing’s syndrome. Based on the CT finding, a decision of exploratory laparotomy was taken. Intraoperatively, a large mass was found on upper surface of right kidney arising from adrenal gland with infiltration to inferior surface of the liver and upper pole of kidney [Table/Fig-2].
CT scan image of Adrenocortical carcinoma of the right adrenal gland (marked with arrow).
Macroscopic aspect- On the cut section, the tumour was nodular, with grayish solid areas, with hemorrhages and necrotic zones, separated by fibrous septa (a and b).
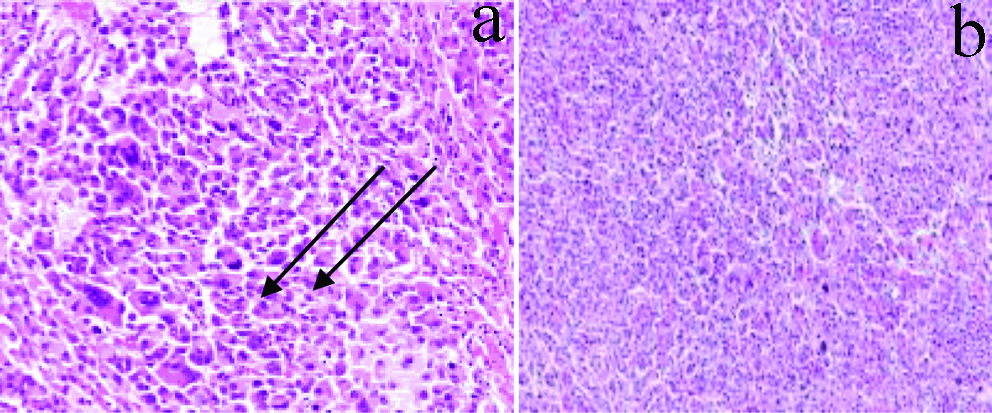
Histopathological examination of the adrenal tumour showed a well-vascularised tumour. There were large, polygonal tumour cells, with basophilic, eosinophilic, or vacuolated cytoplasm, focally with intracytoplasmic hyaline globules [Table/Fig-3]. Hence, Right Adrenalectomy with Right Nephrectomy and wedge resection of liver was done. The postoperative period of the patient was uneventful. Histopathology report revealed oncocytic type of ACC (T.N.M. Staging of pT3, pNx, pMx) with infiltration into the peripheral fat while no infiltration into the kidney, liver, lymph node, blood vessel and ureter. The patient is advised to take tab mitotane 1 gm for five years and follow-up every three months. At present, the patient is asymptomatic and carries out his daily routines.
a) (40X), b) (10X)- Microscopically, at low power view, the clusters of polygonal-shaped cells seen with eosinophilic cytoplasm (arrows), well-defined nucleoli, and atypical mitoses with haematoxylin and eosin stain.
Discussion
The ACC is a rare endocrine cancer with poor outcome or prognosis. It is usually larger than 4 cm and metastasises to liver, lung or lymph nodes at time of diagnosis. The worldwide incidence is 0.5-1 case/million/year. ACC has bimodal age distribution at childhood and the fourth decades of life and incidence of female to male ratio is approximately 1.5:1 [1]. Similarly, in this case, size of the tumour was found to be 12×9.5×10 cm with infiltration into the peripheral fat with no infiltration into the kidney, liver, lymph node, blood vessel and ureter. Mainly, ACC is a non-functioning mass. Patient usually presents with abdominal discomfort or flank pain due to the mass effect. Nevertheless, some of ACC [2] can produce hormones such as corticosteroid, aldosterone [3] or sex steroid [4]. As such, patient with incidental finding of adrenal mass should be evaluated for signs and symptoms of hormone hyper secretion. Patients with functioning ACC may present with clinical symptoms of Cushing syndrome such as round face, easy bruising, truncal obesity, proximal muscle weakness, hyperglycaemias and/or osteoporosis, hyperpigmentation of skin, high blood pressure, headache, depression, decreased libido, decreased fertility, erectile dysfunction and fatigue. Non-functioning ACC patients complain of abdominal discomfort and back pain. The reported patient was comparatively asymptomatic and only had burning micturition.
Diagnosis is done by measurement of serum cortisol, Dehydroepiandrosterone sulphate (DHEAS), catecholamines and dexamethasone suppression test. Imaging studies like ultrasound, CT abdomen pelvis and Magnetic Resonance Imaging (MRI) are useful to evaluate the tumour. ACC frequently presents with metastasis which has to be evaluated by preoperative staging CT scan. CT scan is useful in assessment of central tumour necrosis, calcifications, size, benign adenomas and carcinomas. Typical cases of ACC on CT scan show large unilateral adrenal mass with irregular edges. Macroscopic features of ACC which are suggestive of malignancy include a weight of more than 500 grams, presence of areas of calcification or necrosis and a grossly lobulated appearance. Histologic findings include numerous mitotic scanty cytoplasm. Mainstay of management of ACC is total resection (R0), which is the only potentially curative therapeutic modality [5] for localised ACC. Resection of tumour can ameliorate signs and symptoms of Cushing as well as its complications such as cardiovascular disease and osteoporosis. It has been revealed in several studies that Mitotane can be used as adjuvant therapy in cases of nonoperable ACC or aggressive adrenal gland tumours. It’s mechanism of action is unknown but it is believed that Mitotane is cytotoxic to adrenal gland and it selectively damages zona reticularis and zona fasciculate layer of adrenal cortical tissue [6-8].
Thus, medical management is only supportive and is given as an adjuvant therapy in the form of mitotane 1 gm. This drug has been used for more than 50 years, and continues to be the key element of medical treatment of ACC [9]. According to recent data, it probably exerts effects through the down-regulation of the mitochondrial respiratory chain [10]. An author has showed that mitotane treatment allows prolonging patients’ survival [11]. In another study, patients in stage II treated with mitotane after surgery had a better prognosis for this stage [12]. In the present case, patient underwent right Adrenalectomy with right Nephrectomy and wedge resection of liver and was advised tab mitotane 1 gm for five years and follow-up every three months. Patient at present is doing absolutely well with his daily routine activities and is asymptomatic.
Conclusion(s)
The reported patient did not show any of the clinical symptoms and hence was difficult to diagnose at first. Due to the restricted knowledge reservoir, genuine diagnostic and therapeutic courses are still unclear. Thus, there is a vast portion of medical field to be further explored in order to find an accurate treatment procedure for ACC and a cure is required, so that a patient has minimum chance of secondary tumour infiltration. It would also be good to diagnose asymptomatic cases as early as possible.
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? NA
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 01, 2020
Manual Googling: Sep 29, 2020
iThenticate Software: Nov 13, 2020 (2%)
[1]. Koschker AK, Fassnacht M, Hahner S, Weismann D, Allolio B, Adrenocortical carcinoma improving patient care by establishing new structuresExp Clin Endocrinol Diabetes 2006 144:45-51.10.1055/s-2006-92380816570232 [Google Scholar] [CrossRef] [PubMed]
[2]. Else T, Kim AC, Sabolch A, Raymond VM, Kandathil A, Caoilli EM, Adrenocortical CarcinomaEndocr Rev 2014 35:282-326.10.1210/er.2013-102924423978 [Google Scholar] [CrossRef] [PubMed]
[3]. Veron Esquivel D, Batiz F, Farias Vega A, Carrillo Gonzalez PA, Adrenocortical carcinoma, an unusual cause of secondary hypertensionBMJ Case Rep 2016 pii:bcr201621791810.1136/bcr-2016-21791827927710 [Google Scholar] [CrossRef] [PubMed]
[4]. Hatano M, Takenaka Y, Inoue I, Homma K, Hasegawa T, Sasano H, Feminizing Adrenocortical Carcinoma with Distinct Histopathological FindingsIntern Med 2016 55:3301-07.10.2169/internalmedicine.55.591227853073 [Google Scholar] [CrossRef] [PubMed]
[5]. Libé R, Adrenocortical carcinoma (ACC): Diagnosis, prognosis, and treatmentFront Cell Dev Biol 2015 3:4510.3389/fcell.2015.0004526191527 [Google Scholar] [CrossRef] [PubMed]
[6]. Berruti A, Grisanti S, Pulzer A, Claps M, Daffara F, Loli P, Long-term outcomes of adjuvant mitotane therapy in patients with radically resected adrenocortical carcinomaJ Clin Endocrinol Metab 2017 102:1358-65.10.1210/jc.2016-289428324035 [Google Scholar] [CrossRef] [PubMed]
[7]. Stigliano A, Cerquetti L, Lardo P, Petrangeli E, Toscano V, New insights and future perspectives in the therapeutic strategy of adrenocortical carcinoma (review)Oncol Rep 2017 37:1301-11.10.3892/or.2017.542728184938 [Google Scholar] [CrossRef] [PubMed]
[8]. Waszut U, Szyszka P, Dworakowska D, Understanding mitotane mode of actionJ Physiol Pharmacol 2017 68:13-26. [Google Scholar]
[9]. Fassnacht M, Kroiss M, Allolio B, Update in adrenocortical carcinomaJ Clin Endocrinol Metab 2013 98:4551-64.10.1210/jc.2013-302024081734 [Google Scholar] [CrossRef] [PubMed]
[10]. Hescot S, Slama A, Lombes A, Paci A, Remy H, Leboulleux S, Mitotane alters mitochondrial respiratory chain activity by inducing cytochrome c oxidase defect in human adrenocortical cellsEndocr Relat Cancer 2013 20:371-81.10.1530/ERC-12-036823696597 [Google Scholar] [CrossRef] [PubMed]
[11]. Terzolo M, Angeli A, Fassnacht M, Daffara F, Tauchmanova L, Conton PA, Adjuvant mitotane treatment for adrenocortical carcinomaN Engl J Med 2007 356:2372-80.10.1056/NEJMoa06336017554118 [Google Scholar] [CrossRef] [PubMed]
[12]. Fassnacht M, Johanssen S, Fenske W, Weismann D, Agha A, Beuschlein F, Improved survival in patients with stage II adrenocortical carcinoma followed up prospectively by specialized centersJ Clin Endocrinol Metab 2010 95:4925-32.10.1210/jc.2010-080320668036 [Google Scholar] [CrossRef] [PubMed]