Introduction
The disease is caused by an infectious agent from rickettsial family and is transmitted to humans by the bite of larval form of trombiculid mite known as chiggers. In India, there are many sporadic and epidemic cases reported from many parts, but still are grossly under-diagnosed because of lack of awareness, non-specific clinical scenario, low index of suspicion among physicians and paucity of diagnostic modalities for corroboration of diagnosis. The disease is easily confused with more prevalent diseases like dengue, chikungunya, malaria and leptospirosis because of similarities in presentation [1-5]. It is considered to be an important differential among causes of acute febrile illness and also one of the common cause of multi-organ dysfunction in Intensive Care Unit (ICU) patients. The spectrum of the disease extends from acute febrile illness to dysfunction of multiple organs. The initial manifestations are non-specific and include fever, myalgias, headache, nausea, vomiting and diarrhoea along with splenomegaly and generalised lymphadenopathy. There is also notable involvement of heart, lungs and nervous system as well due to hematogenous dissemination of the organism from the periphery.
There is indeed paucity of literature on the neurological spectrum of scrub typhus, however, central nervous system involvement is one of the known complication of this disease. We hereby, report case series of neurological manifestations of scrub typhus in seven patients presented to tertiary hospital from Jaipur, Rajasthan, India.
Case Series
Case 1
A 28-year-old male farmer by occupation and resident of Bandikui, Rajasthan, presented to Emergency Department (ED) with abnormal body movements and altered sensorium. As per the history given by patient’s elder brother, patient was apparently well six days back when he developed fever that was initially low grade progressing later to high grade from past four days, intermittent in nature and associated with difficulty in breathing from past three days. The patient had no associated co-morbidities. The patient was admitted in the local hospital where chest x-ray was suggestive of bilateral opacification in the lower lobes and was maintaining on intermittent oxygen support, when finally patient had suffered attacks of generalised tonic-clonic seizures with urinary incontinence, tongue bite and up-rolling of eyes. There were consecutive two such episodes with a seizure free interval of 4-5 minutes and finally patient became unresponsive. The patient was then, brought to our institute where he was urgently intubated in view of increased respiratory distress. The Glasgow Coma Scale (GCS) of the patient was E2VTM2 with pupils bilateral responsive and reactive to light and plantars were bilateral flexor. There was terminal neck rigidity present. His vitals were stable and Electrocardiogram (ECG) showed sinus tachycardia. The patient was maintained on volume control mode and broad-spectrum empirical antibiotics (piperacillin, tazobactam) along with antiepileptics (leviteracetam) were started. The Computed Tomography (CT) scan was normal with no signs of any intracranial haemorrhage. All the lab parameters of the patient are described in [Table/Fig-1] (case 1). The lumbar puncture revealed lymphocytic pleocytosis (70 cells) with high protein (86) and normal glucose and viral panel for cerebrospinal fluid was negative. The possibility of meningoencephalitis was kept with acute onset lower respiratory tract infection that could be bacterial or viral. The baseline serology test for tropical infections including dengue, chikungunya, leptospirosis and H1N1 were negative but IgM scrub typhus was found to be positive. The peripheral blood film for malarial parasite was also negative. Tablet Doxycycline (200 mg) was started on day three. The patient was extubated after five days and was then, transferred to the ward for further management. The MRI brain done showed hyperintensities on T2 weighted and FLAIR (Fluid Attenuated Inversion Recovery) sequences in the right temporoparietal cortex along with capsuloganglionic region as well suggestive of encepahalitis. The patient responded tremendously well with doxycycline was finally discharged after 14 days. The patient was further kept on follow-up on conservative management only.
Summarised description of cases 1, 2 and 3 (scrub typhus related meningoencephalitis).
| Case 1 | Case 2 | Case 3 |
|---|
| Demographic characteristics | 28/Male | 54/Male | 37/Male |
| Farmer | Retired | Farmer |
| Rural living | Rural living | Rural living |
| Chief complaint | Fever × 6 daysBreathing difficulty × 3 daysConvulsions × 1 dayAltered mental state × 1 day | Fever × 4 daysCough × 4 daysAltered sensorium × 1 day | Fever × 7 daysCough × 3 daysAltered sensorium × 2 days |
| Past history | Not significant | Chronic Obstructive Airway Disease (COPD) from past 15 years | Chronic Obstructive Airway Disease (COPD) from past 10 years |
| Drug history | None | Bronchodilators | Bronchodialtors |
| Family history | Not significant | Not significant | Not significant |
| General condition | Respiratory distress | Irriatable and drowsy | Drowsy and labored breathing |
| Rash/Eschar | Absent | Absent | Absent |
| Neurolgical examination | Glassgow Coma Scale (GCS) E2VTM2Pupils responsivePlantars flexorsNeck rigidity + | E2V2M4Pupils anisocoriaPlantars extensor withdrawalNeck rigidity presentKernig’s positive | E1V2M2Pupils sluggish reactivePlantars muteNeck rigidity presentKernigs positive |
| Chest Radiograph (CXR) | Bilateral pneumonia | Bilateral lobar pneumonitis | Bilateral basal pneumonitis with syn-pneumonic effusion |
| ECG | Sinus tachycardia | Normal | Sinus bradycardia |
| Arterial Blood Gas (ABG) | | Type 1 respiratory failure | Type 1 respiratory failure |
| Urgent intervention | | IntubatedBroad-spectrum antibiotics(pipercillin-tazobactam and linezolid) | IntubatedBroad-spectrum antibiotics(cefoperazone-sulbactam and linezolid) |
| Investigations | | | |
| Complete Blood Count (CBC) | Normal TLC with increase neutrophills | Normal | Leucocytopenia with thrombocytopenia |
| Liver Function Test (LFT) | S. Bil-2.2 mg/dLSgot/Sgpt--640/220 | SGOT/SGPT 780/124S. BIL Normal | SGOT/SGPT 220/180S. BIL Normal |
| Renal Function Test (RFT) | N | BUN 120 mg/dLS. CREAT 2.27 mg/dL | BUN 88 mg/dLS. CEAT 1.78 mg/dL |
| Electrolytes | N | S. Na 118 mEq/L | S. Na 122 mEq/L |
| Fever profileDengueChikungunyaScrub typhusBrucellosisLeptospirosisWidalH1N1 | + | + | + |
| Cerebrospinal Fluid (CSF) panelCells (mm3)Cell typeProtein (mg/dL)Sugar (mg/dL) | 70Lymphocytes (predominant)8674 | 70Lymphocyte (predominant)80 | 90Polymorphs (predominant)18365 |
| Viral CSF panel | Negative | Negative | Negative |
| Additional investigation | | | |
| Imaging MRI/NCCT/NCV | T2 Weighted image showed hyperintensities in right temporo-pareital cortex along with capsuloganglion region | NCCT Head showing hydrocephalus changes | NCCT Head showing impending hydrocephalic changes[Table/Fig-2] |
| Diagnosis | Scrub Typhus Related Meningoencephalitis | Scrub Typhus Related Meningoencephalitis | Scrub Typhus-Related Meningoencephalitis |
| Differential diagnosis* | | | |
| Treatment | Ceftriaxone 1 gm iv bd for 7 days + Doxycycline 100 mg bd for 10 days | Ceftriaxone 1 gm iv bd for 10 daysDoxycycline 100 mg PO bd for 10 daysDexamethasone 6 mg iv od for 7 daysSyp glycerol 30 mL every 6 hourly for 7 days | Ceftriaxone 1 gm iv bdVancomycin 1 gm in 500 normal saline iv bdDoxcycline 100 mg PO bdDexamethasone 6 mg iv odSyp glycerol 30 mL every 6 hourly |
| Outcome | Recovery and discharge after 14 days. | Died after five days | Died after two days |
| Follow-up | Kept on symptomatic build (multivitamin+ calcium) up therapy for two weeks | Died | Died |
*(the differential diagnosis in all three of the above cases was kept as meningoencephalitis with acute onset lower respiratory tract infection likely rickettsial or viral but positive serology of IgM scrub typhus substantiated the diagnosis to be scrub typhus related meningoencephlaitis)
CXR: Chest X-ray, Eye Opening (E), Verbal Response (V), Motor Response (M); ECG: Electrocardiogram; ABG: Arterial blood gas analysis CBC: Complete blood count; TLC: Total leukocyte count; RFT: Renal function test; LFT: Liver function test; SGOT: Serum glutamic oxaloacetic transaminase; SGPT: Serum glutamic pyruvic transaminase; S Bil: Serum billirubin; BUN: Blood urea nitrogen; S. Creat: Serum creatinine; S Na: Serum sodium; MRI: Magnetic resonance imaging; NCCT: Non contrast computed tomography; NCV: Nerve conduction velocity study
Case 2 and 3
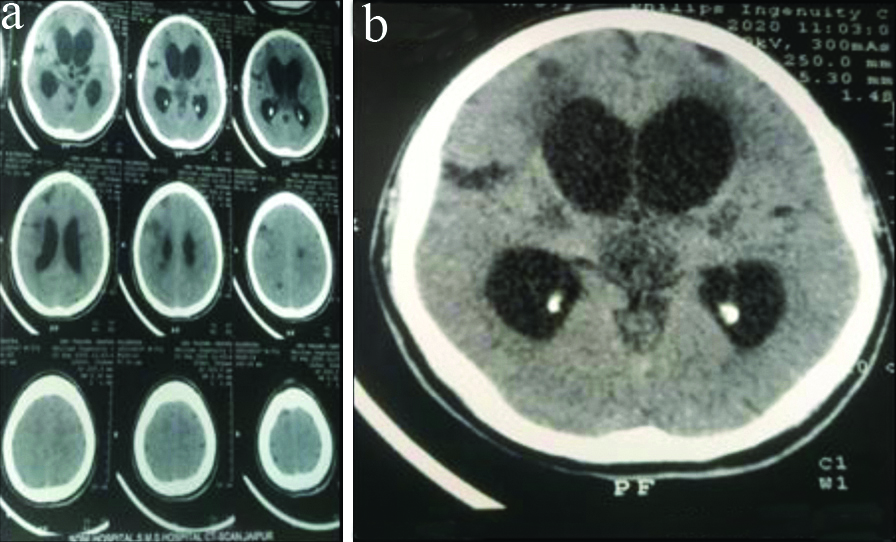
These two cases were also present with fever, lower respiratory tract symptoms and altered sensorium. The following were their hallmark features of case 1, 2 and 3 as illustrated in the [Table/Fig-1] below. For case 3 Non-Contrast Computed Tomography (NCCT) head showing impending hydrocephalic changes is shown in [Table/Fig-2].
NCCT head showing impending hydrocephalus changes in axial section as illustrated in case 3 with image a showing complete NCCT film and image b showing magnified view of single axial cut section.
Case 4
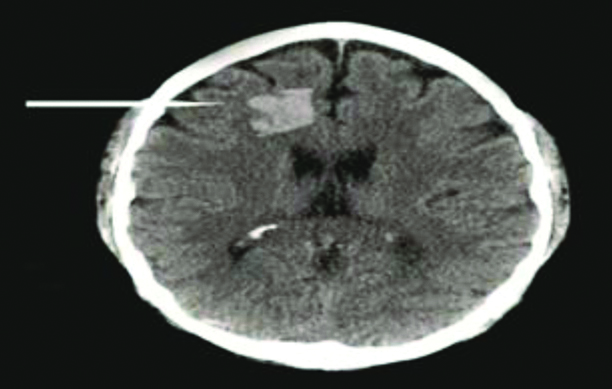
A 64-year-old male resident of Bharatpur (Rajasthan) presented to Medicine OutPatient Department (OPD) with a complaint of generalised mylagias since a week followed by fever past five days. The patient also complained of headache from past two days moderate-to-severe in intensity mainly localised to anterior half. There was no history of any trauma. The patient was chronic smoker. There was no other significant medical, family or social history. The general physical and neurological examination along with all lab reports is mentioned in [Table/Fig-3]. The fever profile of the patient for chikungunya, dengue, malaria and widal agglutination test were all negative. In view of rising cases of scrub typhus in the medicine wards, possibility of scrub typhus in view of fever and maculopapular rash was suspected and four fold increase in IgM scrub typhus titre was found to be positive. The patient was initiated on ceftriaxone and doxycycline and fever of the patient also responded. The patient was afebrile after two days. On day third of admission, patient was still complaining of headache that persisted despite giving analgesics and antipyretics. The following day NCCT head was done in view of persisted headache and it was suggestive of focal hyperdensity in the left frontal parietal region suggesting intra cerebral haemorrhage as shown in [Table/Fig-4] and CT angiography brain was suggestive of no abnormality. The neurosurgeon opinion was taken and patient was advised conservative treatment approach on anti-oedema measures and prophylactic antiepileptics were initiated. The patient was then discharged on 8th day of admission.
Summarised description of cases 4 (scrub typhus related intra cerebral haemorrhage), 5 (scrub typhus related gullain barre syndrome), 6 (scrub typhus related cerebral venous thrombosis) and 7 (scrub typhus related cerebellitis), (the possibility of other differential diagnosis was kept and each differential was thoroughly evaluated based on relevant investigations).
| Case 4 | Case 5 | Case 6 | Case 7 |
|---|
| Demography | 64/Male | 20/Male | 20/Male | 40/Male |
| Farmer | Student | Student | Farmer |
| Rural living | Rural living | Rural living | Rural living |
| Chief complaint | Fever × 5 daysHeadache × 2 days | Fever × 5 daysBilateral lower limb weakness × 1 day | Fever × 7 daysDifficulty breathing × 3 daysConvulsions × 1 day | Fever × 6 daysHeadache/vomiting × 4 daysDifficulty walking × 1 day |
| Past history | Chronic obstructive airway disease | Not significant | Not significant | Not significant |
| Drug history | Bronchodilators | Not significant | Not significant | Not significant |
| Family history | Not significant | Not significant | Not significant | Not significant |
| General condition | ConsciousIrritableFebrile | Conscious oriented | ConfusedDrowsy | Conscious oriented |
| Rash/Eschar | Maculopapular rash over trunk | Absent | Absent | Absent |
| Neurolgical examination | E4V5M6 | E4VTM1b/l plantars muteDTR’S absentPower 1/5Sensory and bowel bladder intact | E3V3M5pupils responsive and reactiveplantars extensorsno neck rigidity | E4V5M6Dysdiadokinesia +Finger nose finger test +Knee heel test +DTR +Plantars flexorsSpeech normalNystagmus not found |
| CXR | Normal | Normal | Bilateral pneumonia | Normal |
| ECG | Normal | Normal | Sinus tachycardia | Normal |
| Urgent intervention | | Electively intubated and put on ventilator in view of decrease single breath count. | | |
| Investigations | | | | |
| CBC | Normal | Normal | LeucocytopeniaThrombocytopenia | Thrombocytopenia |
| LFT | Normal | Normal | SGOT/SGPT 780/1100S. bilirubin normal | Normal |
| RFT | Normal | Normal | Blood Urea Nitrogen (BUN) 110 mg/dLS. Creatinine 2.31 mg/dL | Normal |
| Electrolytes | Normal | Normal | Normal | Normal |
| Fever profileDengueChikungunyaScrub typhusBrucellosisLeptospirosisWidalH1N1 | + | + | + | + |
| CSF panelCELLS (mm3)Cell typeProtein (mg/dL)Sugar (mg/dL) | Not doneNot specified | 5Not specified17084 | Not doneNot specified | 2Not specified2396 |
| Viral CSF panel | --------------- | Negative | ---------------- | Negative |
| Additional investigation | | | Coagulation panel normal | |
| Imaging MRI/NCCT/NCV | Intracerebral haemorrhage[Table/Fig-4] | Nerve Conduction Velocity (NCV) suggestive of demyelinating affection of nerves of all four limbs | MRI s/o thrombus in superior saggital sinus[Table/Fig-5] | Enhancement of cerebellar hemispheres L> R[Table/Fig-6] |
| Diagnosis | Scrub typhus related Intra cerebral haemorrhage | Scrub typhus associated GBS | Scrub typhus associated cerebral venous thrombosis | Scrub typhus related cerebellitis |
| Differential diagnosis | Intracerebral haemorrhage due to? smoking? vasculitis(CT Angiography Brain Normal) | Lower motor neuron type of quadriparesis cause infections? viral fevers | Hypercoagulable states likeDeficiency of protein c/protein s/anti thrombin 3 hyperhomocysteinemia APLA antibodies
(Ruled out on Basis of Coagulation Panel) | CerebellitisCausesInfectious? viral fevers Post-infectious
(Not Evaluated All Viral Fevers as Scrub Typhus Already Positive) |
| Treatment | Mannitol 100 cc iv tds with tapering for seven days Syp glycerol 30 mL 6-hourly Phenytoin 10 mg/kg body weight IV for seven days followed by oral maintenance for five months
| IVIg 0.04 g/kg/d for five daysDoxycycline 100 mg po bd | Piperacillin tazobactam 4.5 gm iv tds for 7 days Doxycycline 100 mg bd PO for 14 days UFH 5000 IU TDS for 5 days WARFARIN 3 mg for 1 month followed by 2 mg for 4 months with PT-INR monitoring
| Ceftriaxone 1 gm iv bd for 10 days Doxycycline 100 mg bd PO for 14 dyas Dexamethasone 6 mg iv od for 7 days Mannitol 100 cc iv tds for 7 days with gradual tapering
|
| Outcome | Discharged after eight days. | Discharged with recovery of power after 14 days | Discharged | Discharged with residual right side weakness |
| Follow-up | Residual weakness recovered after one month period and medication (mannitol + phenytoin) stopped thereafter | Residual weakness recovered after one week of discharge | Patient follow-up on leviteracetam and warfarin for three months with no convulsions thereafter. | Follow-up on dexamethasone and glycerol for one month period with no residual weakness after 1.5 months |
ALPA: Antiphospholipid Antibodies; GBS: Gullain barre syndrome; ICH: Intracerebral haemorhage; MRI: Magnetic resonance imaging; NCCT: Non contrast computed tomography; NCV: Nerve conduction velocity study; CBC: Complete blood count; TLC: Total leukocyte count; RFT: Renal function test, LFT: Liver function test; SGOT: Serum glutamic oxaloacetic transaminase; SGPT: Serum glutamic pyruvic transaminase; S Bil: Serum billirubin; BUN: Blood urea nitrogen; S. CREAT: Serum creatinine; DTR: Deep tendon reflexes
NCCT head showing focal intra parenchymal haemorrhage.
The summarised description of this case is given below in the [Table/Fig-3] along with other cases 5 to 7.
Case 5
A 20-year-old male resident of Alwar (Rajasthan) presented to ED with a chief complaint of fever since five days and lower limb weakness since one day. The fever was gradual in onset, intermittent in nature, not associated with chills and rigor and subsided with medication. The night before arrival in the ED, patient had took his dinner and went to bed to wake up in the morning and found weakness in both of his legs. On arrival in the emergency, the weakness has progressed to a state to unable to stand with support. The weakness was pure motor type. Eventually patient had developed breathing difficulty on the night of admission and his single breath count was below 10. Hence, the patient was electively intubated and put on ventilator. The detailed neurological examination is given in [Table/Fig-3]. All of the lab parameters of the patient were normal but IgM scrub typhus was found to be positive as patient was hailing from the endemic zone of scrub typhus of Rajasthan. The probable diagnosis of Gullain Barre Syndrome (GBS) was kept. The patient was initiated on immunoglobulins as 0.04 g/kg/d for a period of five days along with doxycycline course. Later lumbar puncture suggestive of albumin cytological dissociation with cells 5/mm3 and proteins 170 mg/dL. The nerve conduction study showed demyelinating affection of upper and lower limb nerves. The patient condition gradually improved symptomatically and was extubated with the return of respiratory effort. Finally, the power was regained in the limbs and patient was discharged after 14 days.
{The summarised description of this case is given in the [Table/Fig-3] along with other cases 4, 6 and 7}.
Case 6
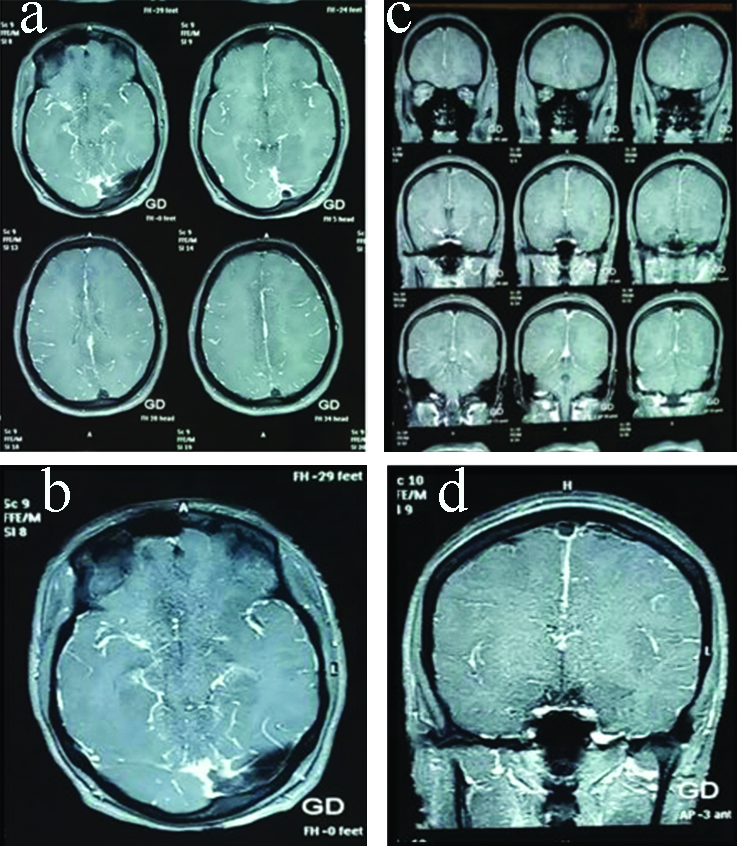
A 20-year-old male resident of Alwar, Rajasthan arrived in ED with complain of fever from past seven days and shortness of breath from past three days and abnormal body movements from past one day. The patient was apparently well seven days back when he developed fever that was intermittent in nature not associated with chills and rigor, initially low grade and gradually progressed to high grade from past three days but subsided with antipyretics. The above mentioned complaint was also associated with shortness of breath from past three days that was insidious in onset and gradually progressive in nature, initially precipitated with moderate activity but eventually progressed to be present at rest not associated with chest pain, haemoptysis, palpitiations and syncopal attacks. There was no significant past history or drug history. In view of above situation, patient was admitted in local hospital nearby and was maintaining on oxygen support, when he developed convulsions since morning that were generalised in nature associated with tongue bite, urinary incontinence, up-rolling of eyes, frothing from mouth followed by a state of post-ictal state of drowsiness. The patient was finally referred to our institute. At the time of admission, saturation was 91% on oxygen support with bilateral pneumonitis in the lower zones on chest x-ray. The patient was irritable, confused with GCS of E3V3M5, pupils were responsive and reactive to light, plantars were bilateral extensors and deep tendon reflexes were all present. There was no nuchal rigidity or any signs of meningeal irritation. The patient was started on broad-spectrum antibiotics like pipercillin-tazobactam and linezolid along with anti-epileptics (leviteracetam). The fever profile was normal but IgM scrub typhus titres were significantly raised. The MRI brain showed loss of flow signals in superior sagittal sinus, bilateral transverse sinus and sigmoid sinus with multiple collateral formation seen over right occipital lobe [Table/Fig-5]. The coagulation profile of the patient was within normal limit. Finally, the probable diagnosis was scrub typhus induced bilateral pneumonitis with cerebral venous thrombosis was kept. The patient was kept on doxycycline, piperacillin tazobactam, unfractionated heparin and later on warfarin along with antiepileptics (detailed in the [Table/Fig-3]). The condition of the patient responded dramatically well with a seizure free period and clearing of x-ray was obtained after four weeks period. Eventually, patient was discharged warfarin and anti-epileptics and was kept on follow-up as of now (three months) on tablet leviteracetam.
MRI brain showing loss of flow signals in superior sagittal sinus, bilateral transverse sinus and sigmoid sinus with multiple collateral formation seen over right occipital lobe. Image a and b are axial section and image c and d are saggital section.
{The summarised description of this case is given in the [Table/Fig-3] along with other cases 4, 5 and 7}.
Case 7
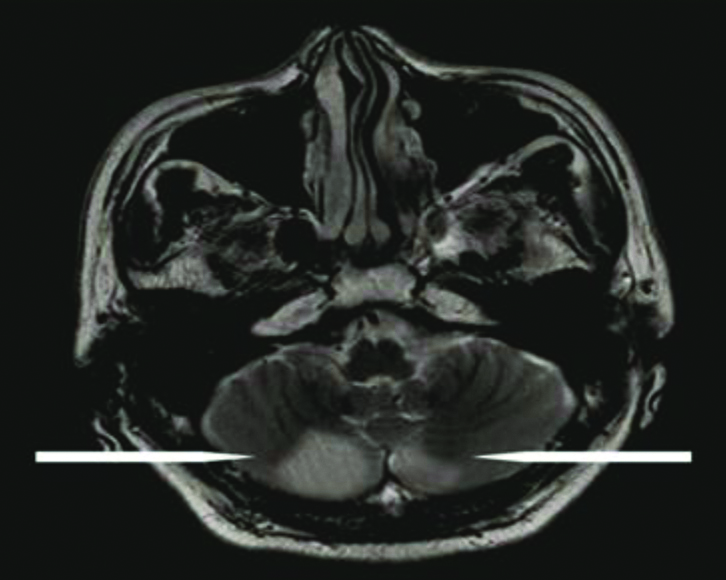
A 40-year-old male resident of Jhunjhunu, Rajasthan, farmer by occupation came to emergency with a complaint of difficulty in walking or increase in tendency to fall while walking since morning. The patient also gave the history of fever since past six days associated headache and vomiting from past four days. The urgent NCCT head done in the emergency was within normal limits with no obvious signs of intracranial haemorrhage. The neurological examination of the patient given in [Table/Fig-3]. All lab parameters were within normal limit except for thrombocytopenia. In view of fever with decrease platelet count, a thorough search for tropical infections revealed positive serology for scrub typhus. The routine CSF biochemistry and cell count, cell type was also remarkably normal along with negative viral panel-herpes simplex virus, ebstein barr virus and cytomegaloviruses. The MRI brain as shown in [Table/Fig-6] showed enhancement in cerebellar hemispheres that was more in left then right along with hyperintensities in the left temporal horn as well. The patient was finally put on ceftriaxone 2 gm and doxcycline 200 mg along with prophylactic anti-oedema measures to prevent development of hydrocephalus. The patient condition improved and was discharged after 20 days with some residual weakness in right lower limb but still the ataxia was markedly improved with minimal swaying.
MRI showing cerebellitis more in left then right cerebellar hemispheres.
The summarised description of this case is given below in the [Table/Fig-3] along with other cases 4, 5 and 6.
Discussion
The Orientia tsutsugamushi is a gram negative coccobacilli which belong to rickettsial class of infection, is obligatory intracellular organism responsible for causation of scrub typhus. The disease majorly predominates in the terrains of South-East Asia and Western Pacific Regions thereby regarding this geography as tsutsugamushi triangle [6]. It was first populated in Japan, where the term tsutsugamushi was given, meaning small and dangerous creatures. The mode of transmission to the humans is mainly by the bite of larval stage of trombiculid mite, known as chiggers. The mite belongs to leptotrombidium deliense group. The life cycle of Orientia is maintained by transovarian transmission of the mite thereby, making the chiggers to be infective. The chiggers is the only stage that feeds on host and inoculates infective organism into the skin of the host. The natural reservoir host of the chiggers is wild rats, over which the chiggers usually feed upon. The humans are actually considered to be accidental host that inhabit the infection when come in contact with the infected chiggers that are mainly found in areas of heavy scrub vegetations especially during the wet seasons, in the crop fields or in the terrains of dense woods and mountainous zones. Therefore, the disease is more common among the people working outdoors with major exposure to soil. The eschar is considered to be pathognomonic hallmark of scrub typhus is often inconspicuous and is often evident in only 50% of the patients [7]. In India, the disease have been documented in many parts mainly Himachal Pradesh, many states of eastern and southern India especially during monsoon and post-monsoon period [8-12]. In Rajasthan, the disease is encountered in the rural areas of Bharatpur, Karauli, Alwar and Dausa (North-Western Rajasthan).
By thoroughly searching the online database of Pubmed, Google Scholar, Cochrane Library using mesh words like “Scrub Typhus”, “meningoencephalitis”, “neurological manifestations”, “cerebellitis” and “myelitis”, able to found out some of the literature that corroborates the details about prevailing data of neurological manifestations of scrub typhus as depicted in [Table/Fig-7] [10,13-16]. Most of the literature on scrub typhus neurological manifestations is individual case reports and there are very few case series available. Also, there is huge paucity of literature from India.
Compilation of research showing neurological manifestations in scrub typhus.
| Study | Scrub typhus subjects | Findings |
|---|
| Misra UK et al., [10] | 37 | 13 meningo encephalitis (35%)6 encephalitis (16%)9 encephalopathy (24%) |
| Sardana v and Shringi P [13] | 5 | 2 meningo encephalitis2 Acute Disseminated Encephalomyelitis (ADEM)1 cerebral venous sinus thrombosis |
| Rana A et al., [14] | 37 | 15 meningoencephalitis (40%)4 cerebellitis (11%)2 cerebral haemorrhages (5%)1 sixth nerve palsy (2%)1 acute transverse myelitis (2%) |
| Vishwanathan S et al., [15] | 65 | 17 meningits (26%) |
| Kim DM et al., [16] | 89 severe infection | 23 meningitis (11.3%) |
As explained previously that clinical spectrum of scrub typhus is variable ranging from non-specific febrile illness to involvement of multiple organs, due to haematogenous dissemination of the infection [17]. The multiple Central Nervous System (CNS) manifestations in scrub typhus can either be due to direct invasion into CNS territory like meningitis, meningoencephalitis, seizures or can be due to some immune mediated mechanism based on molecular mimicry phenomena like GBS, myelitis [18,19]. Out of all, meningoencephalitis was the most common (42.2%) manifestation being reported, that corroborates with other previous studies done Misra UK et al., [20]. The scrub typhus should be considered in the differential diagnosis of subacute meningitis like tubercular meningitis as evident in present study as well. Also, pure or isolated cerebellitis is rarely reported with scrub typhus infection but can occur along with meningoencephalitis as evident in study done by Gupta S et al., [11]. There are few case reports where scrub typhus is implicated in the causation of cerebrovascular accidents [21,22]. The organism has the potential for causing thrombotic and haemorrhagic manifestations by causing vessel wall inflammation presenting as vasculitis and perivasculitis with superimposed endothelial dysfunction and coagulopathies, hence causing haemorrhages. The reason for endothelial dysfunction following vasculitis is mainly the cytokine storm that damages the integrity of endothelium and leakage of fluid occurs. In response to the cytokine release, the inflammatory pathways are up regulated causing polymorphs recruitment and platelet aggregation leading to occurrence of thrombotic complications as well [23,24]. The thrombosis if happened in the venous sinuses of the brain can lead to cerebral venous thrombosis as evident in present case. The cerebral venous thrombosis following scrub typhus is very rare and only three cases are reported so far. The exclusion of hypercoagulability panel and evidence of scrub typhus infection could be the possible etiology. Scrub typhus is also associated with GBS as evident in very few case reports previously [25,26]. GBS is an immunologically mediated demyelinating polyneuropathy majorly associated with preceding gastrointestinal or respiratory infection. It is rarely associated with scrub typhus. The potential mechanism is multiple including formation of immune complex antibodies occluding the vasa nervosum or inflammatory mediators damaging the nerves [27,28].
For microbiological diagnosis of scrub typhus, serological test is highly valuable based upon micro-immunofluorescence assay. Other available test is Polymerase Chain Reaction (PCR), Enzyme Linked Immunosorbent Assay (ELISA), latex agglutination test and indirect haemagglutination. In index study, of seven patients of scrub typhus, with all patients belonging to rural background, and all patients have significant raised titres of IgM scrub typhus antibodies on ELISA. The sensitivity of ELISA is 100% and specificity is 95% tests [29].
Conclusion(s)
Despite of central nervous system involvement as one of the known complication of scrub typhus, there is indeed paucity of literature over this important topic. In this context, we endeavour to present some of the neurological manifestations of scrub typhus that are otherwise likely to be missed because of low index of awareness among the treating physicians thereby, corroborating the need for early diagnosis and treatment.
Declaration of Conflict of Interest
All radiographic images could not be procured from the records.
[1]. Cowan GO, Friman G, Gunther G, Rickettsial infections. In: Gordon C (ed.)Manson’s Tropical Diseases 2003 21st edLondonElsevier Health Sciences:891-906. [Google Scholar]
[2]. Sharma A, Mahajan S, Gupta ML, Kanga A, Sharma V, Investigation of an outbreak of scrub typhus in the Himalayan region of IndiaJpn J Infect Dis 2005 8:208-10. [Google Scholar]
[3]. Vivekanandan M, Mani A, Priya YS, Singh AP, Jayakumar S, Purty S, Outbreak of scrub typhus in PondicherryJ Assoc Physicians India 2010 58:24-28. [Google Scholar]
[4]. Saifudheen K, Kumar KG, Jose J, Veena V, Gafoor VA, First case of scrub typhus with meningoencephalitis from Kerala: An emerging infectious threatAnn Indian Acad Neurol 2012 15:141-44.10.4103/0972-2327.9500222566732 [Google Scholar] [CrossRef] [PubMed]
[5]. Goswami D, Hing A, Das A, Lyngdoh M, Scrub typhus complicated by acute respiratory distress syndrome and acute liver failure: A case report from Northeast IndiaInt J Infect Dis 2013 17:e644-45.10.1016/j.ijid.2012.12.02323402799 [Google Scholar] [CrossRef] [PubMed]
[6]. Vaz LS, Gupta NK, Outbreak of scrub typhus in Jammu-A reportMJAFI 2006 62:342-43.10.1016/S0377-1237(06)80103-6 [Google Scholar] [CrossRef]
[7]. Chunchanur SK, Scrub typhus in India- An impending threatAnn Clin Immun Microbiol 2018 1:1003 [Google Scholar]
[8]. Drevets DA, Leenen PJ, Greenfield RA, Invasion of central nervous system by intracellular bacteriaClin Microbiol Rev 2004 17:323-47.10.1128/CMR.17.2.323-347.200415084504 [Google Scholar] [CrossRef] [PubMed]
[9]. Schonberger LB, Hurwitz ES, Katona P, Holman RC, Bregman DJ, Guillain-Barré syndrome: Its epidemiology and association with influenza vaccinationAnn Neurol 1981 9(Suppl):31-38.10.1002/ana.4100907077224614 [Google Scholar] [CrossRef] [PubMed]
[10]. Misra UK, Kalita J, Mani VE, Neurological manifestations of scrub typhusJ Neurol Neurosurg Psychiatry 2015 86(7):761-66.10.1136/jnnp-2014-30872225209416 [Google Scholar] [CrossRef] [PubMed]
[11]. Gupta S, Grover S, Gupta M, Kaur D, Cerebellitis as a rare manifestation of scrub typhus feverBMJ Case Rep2020:13:e23399310.1136/bcr-2019-23399332414774 [Google Scholar] [CrossRef] [PubMed]
[12]. Gulati S, Maheshwari A, Neurological manifestations of scrub typhusAnn Indian Acad Neurol 2013 16(1):13110.4103/0972-2327.10770123661984 [Google Scholar] [CrossRef] [PubMed]
[13]. Sardana V, Shringi P, Neurological manifestations of scrub typhus: A case series from tertiary care hospital in southern east RajasthanAnnals of Indian Academy of Neurology10.4103/aian.AIAN_97_1933688133 [Google Scholar] [CrossRef] [PubMed]
[14]. Rana A, Mahajan SK, Sharma A, Sharma S, Verma BS, Sharma A, Neurological manifestations of scrub typhus in adultsTrop Doct 2017 47:22-25.10.1177/004947551663654327059055 [Google Scholar] [CrossRef] [PubMed]
[15]. Viswanathan S, Muthu V, Iqbal N, Remalayam B, George T, Scrub typhus meningitis in South India- A retrospective studyPLoS ONE 2013 8(6):e6659510.1371/journal.pone.006659523799119 [Google Scholar] [CrossRef] [PubMed]
[16]. Kim DM, Kim SW, Choi SH, Yun NR, Clinical and laboratory findings associated with severe scrub typhusBMC Infectious Diseases 2010 10:10810.1186/1471-2334-10-10820433689 [Google Scholar] [CrossRef] [PubMed]
[17]. Chung JH, Yun NR, Kim DM, Lee JW, Yoon SH, Kim SW, Case report: Scrub typhus and cerebrovascular injury: A phenomenon of delayed treatmentAm J Trop Med Hyg 2013 89(1):119-22.10.4269/ajtmh.13-009423716407 [Google Scholar] [CrossRef] [PubMed]
[18]. Levine HD, Pathologic study of thirty-one cases of scrub typhus fever with especial reference to the cardiovascular systemAm Heart J 1946 31:314-28.10.1016/0002-8703(46)90313-4 [Google Scholar] [CrossRef]
[19]. Ono Y, Ikegami Y, Tasaki K, Abe M, Tase C, Case of scrub typhus complicated by severe disseminated intravascular coagulation and deathEmerg Med Australas 2012 24:577-80.10.1111/j.1742-6723.2012.01600.x23039302 [Google Scholar] [CrossRef] [PubMed]
[20]. Lee SH, Jung SI, Park KH, Choi SM, Park MS, Kim BC, Guillain-Barré syndrome associated with scrub typhusScand J Infect Dis 2007 39:826-28.10.1080/0036554070126675517701724 [Google Scholar] [CrossRef] [PubMed]
[21]. Ju IN, Lee JW, Cho SY, Ryu SJ, Kim YJ, Kim SI, Two cases of scrub typhus presenting with Guillain-Barré syndrome with respiratory failureKorean J Intern Med 2011 26:474-76.10.3904/kjim.2011.26.4.47422205852 [Google Scholar] [CrossRef] [PubMed]
[22]. Wijesundere A, Guillain-Barre syndrome in Plasmodium falciparum malariaPostgrad Med J 1992 68(799):376-77.10.1136/pgmj.68.799.3761630986 [Google Scholar] [CrossRef] [PubMed]
[23]. Berkowitz AL, Thakur KT, Acute inflammatory demyelinating polyradic-uloneuropathy following malariaJournal of Clinical Neuroscience 2014 21(4):704-06.10.1016/j.jocn.2013.07.03124417794 [Google Scholar] [CrossRef] [PubMed]
[24]. Palanivel S, Nedunchelian K, Poovazhagi V, Raghunandan R, Ramachandran P, Clinical profile of scrub typhus in childrenIndian J Pediatr 2012 79:1459-62.10.1007/s12098-012-0721-022374234 [Google Scholar] [CrossRef] [PubMed]
[25]. Misra UK, Kalita J, Singh AP, Role of vascular endothelial growth factor (VEGF) in the neurological manifestations of dengue: A preliminary studyInflammation 2014 37:611-14.10.1007/s10753-013-9776-y24292799 [Google Scholar] [CrossRef] [PubMed]
[26]. Nand N, Aggarwal H, Sharma M, Singh M, Systemic manifestations of malariaJ Indian Acad Clin Med 2001 2:189-94. [Google Scholar]
[27]. Kalita J, Misra UK, Maurya PK, Shankar SK, Mahadevan A, Quantitative electromyography in dengue-associated muscle dysfunctionJ Clin Neurophysiol 2012 29:468-71.10.1097/WNP.0b013e31826be02923027105 [Google Scholar] [CrossRef] [PubMed]
[28]. Bal AM, Unusual clinical manifestations of leptospirosisJ Postgrad Med 2005 51:179-83. [Google Scholar]
[29]. Tandale BV, Sathe PS, Arankalle VA, Wadia RS, Kulkarni R, Shah SV, Systemic involvements and fatalities during chikungunya epidemic in India, 2006J Clin Virol 2009 46:145-49.10.1016/j.jcv.2009.06.02719640780 [Google Scholar] [CrossRef] [PubMed]