According to International Association for the Study of Pain, trigeminal neuralgia is defined as sudden, unilateral, severe, brief, stabbing, recurrent episodes of pain in the distribution of one or more branches of the trigeminal nerve [1]. It may be idiopathic or have secondary causes. However, some patients experience moderate intense continuous pain along the affected nerve distribution. The annual incidence of trigeminal neuralgia is 4 to 5 in 100,000 with a higher prevalence in women [2,3]. It is rare below the age of 40, though it can also affect paediatric population [4].
The latest classification of the International Headache Society distinguishes between Classic, Secondary and Idiopathic Trigeminal neuralgia [5]. Classic trigeminal neuralgia includes all cases without an established aetiology (those with potential vascular compression-typically atrophy or displacement of the fifth cranial nerve). If any of the investigations recognise any structural abnormality which is different from the vascular compression affecting the trigeminal nerve; then it is termed as Secondary trigeminal neuralgia. It includes multiple sclerosis plaques, tumours in cerebellopontine angle, AV malformations and abnormalities of the skull base. When evaluation and imaging is normal, it is then termed as idiopathic trigeminal neuralgia [5].
Most clinicians see only a few patients because of the rareness of the disease with an estimated prevalence of 0.3%, and it is clinically evident that this is both misdiagnosed and undertreated [6]. These patients present a marked reduction in the quality of life in view of the nature and severity of pain [7].
The aim of this study was to evaluate the clinical profile and radiological imaging features in trigeminal neuralgia patients. This may help in a better understanding of the disease along with an early and appropriate management in these patients.
Materials and Methods
A cross-sectional study was conducted using the medical records of 60 adult patients with Trigeminal Neuralgia who attended the Neurology outpatient department at Travancore Medical College, Kollam between June 2015 and June 2020. This study was approved by Institutional Ethics committee Review Board (TMC/069/20).
Inclusion criteria and Exclusion criteria:
Patients diagnosed with trigeminal neuralgia as per the Criteria of the International Headache Society (ICHD 3), were included in the study [5]. Patients were excluded if: (a) with atypical facial pain (as per ICHD3); (b) not fulfilling the criteria for trigeminal neuralgia; (c) patients with prior history of neurosurgery procedure; (d) patients with prior history of trauma; (e) patients whose work up is incomplete/MRI is not done; (f) associated connective tissue disorder.
The following variables were studied: (a) Age; (b) Gender; (c) Dental treatment/tooth extraction; (d) Severity of pain based on Numeric Pain Rating scale {0-No Pain, 1 to 3- Mild Pain, 4 to 6- Moderate Pain and 7 to 10- Severe Pain}; (e) Trigger factors- chewing, touch, brushing teeth, eating, talking, breeze; (f) Side- left/right/bilateral; (g) Area involved V1/V2/V3/V1+V2/V2+V3/V1+V2+V3; (j) Sensory abnormalities: hypoesthesia, hyperesthesia, allodynia, hypoalgesia; (h) MRI.
MRI Imaging
MRI Brain of the 60 patients in the study was conducted with 1.5T Siemens unit system. The protocols used were: axial T1, T2, FLAIR, 3D CISS, postcontrast T1 series in case of suspicious lesions. Neurovascular compression with atrophy or displacement in the trigeminal nerve root, structural lesion, infarct, demyelinating plaque, space occupying lesion was assessed.
Based on the subtypes of trigeminal neuralgia (Classical, Secondary and Idiopathic), various clinical features were analysed.
ICHD-3 Criteria for Diagnosis of Trigeminal Neuralgia [
5]
Recurrent paroxysms of unilateral facial pain in the distribution(s) of one or more divisions of the trigeminal nerve, with no radiation beyond, and fulfilling criteria B and C
Pain has all of the following characteristics:
lasting from a fraction of a second to 2 minutes
severe intensity
electric shock-like, shooting, stabbing or sharp in quality
Precipitated by innocuous stimuli within the affected trigeminal distribution
Not better accounted for by another ICHD-3 diagnosis.
ICHD-3 Criteria for Diagnosis of Classical Trigeminal Neuralgia [
5]
Recurrent paroxysms of unilateral facial pain fulfilling criteria Trigeminal neuralgia
Demonstration on MRI or during surgery of neurovascular compression (not simply contact), with morphological changes (atrophy or displacement) in the trigeminal nerve root.
ICHD-3 Criteria for Diagnosis of Secondary Trigeminal Neuralgia [
5]
Recurrent paroxysms of unilateral facial pain fulfilling criteria for Trigeminal neuralgia, either purely paroxysmal or associated with concomitant continuous or near-continuous pain
An underlying disease has been demonstrated that is known to be able to cause, and explaining the neuralgia
Not better accounted for by another ICHD-3 diagnosis
ICHD-3 Criteria for Diagnosis of Idiopathic Trigeminal Neuralgia [
5]
Recurrent paroxysms of unilateral facial pain fulfilling criteria for Trigeminal neuralgia,
Neither Classical trigeminal neuralgia nor Secondary trigeminal neuralgia has been confirmed by adequate investigation
Not better accounted for another ICHD-3 diagnosis.
ICHD-3 Criteria for Diagnosis of Atypical Facial Pain [
5]
Facial and/or oral pain fulfilling criteria B and C
Recurring daily for >2 hours/day for >3 months
Pain has both of the following characteristics:
poorly localised, and not following the distribution of a peripheral nerve
dull, aching or nagging quality
Clinical neurological examination is normal
A dental cause has been excluded
Statistical Analysis
Data was analysed with SPSS statistical software. (SPSS, version 20.0, Chicago, IL, USA). Categorical variables were presented in number and percentage and were compared using Chi-square test. A p<0.05 was considered statistically significant.
Results
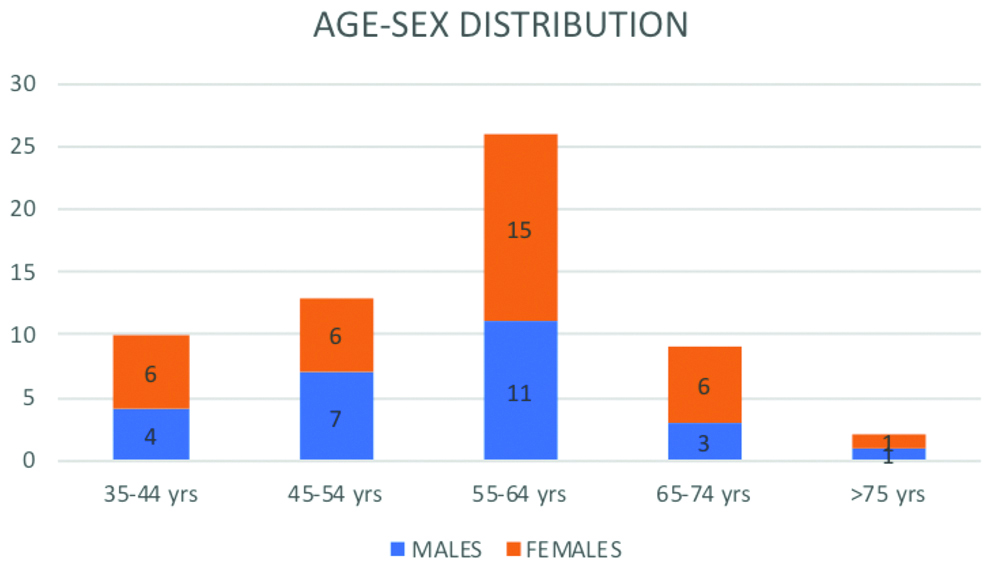
Among the 60 patients studied with trigeminal neuralgia, 26 (43.3%) were males and 34 (56.7%) were females. About 25 had maxillary nerve division distribution (41.7%), 57 patients experienced shock/lancinating pain (95%), touch and breeze as common trigger factors in 54 (90%). The median age among males was 52.4 years and females were 56.5 years [Table/Fig-1].
Association between clinical features and gender.
| Clinical features | Male (N=26) | Female (N=34) | Total (N=60) | p-value* |
|---|
| Side of face |
| Left | 10 (38.4%) | 14 (41.2%) | 24 (40%) | 0.8315 |
| Right | 16 (61.6%) | 20 (58.8%) | 36 (60%) |
| Division of nerve |
| V2 | 11 (42.3%) | 14 (41.2%) | 25 (41.7%) | 0.8385 |
| V3 | 9 (34.6%) | 10 (29.4%) | 19 (31.7%) |
| V2+V3 | 6 (23.1%) | 10 (29.4%) | 16 (26.6%) |
| Pain character |
| Shock like/Lancinating | 24 (92.2%) | 33 (97.1%) | 57 (95%) | 0.5018 |
| Throbbing | 1 (3.9%) | 1 (2.1%) | 2 (3.3%) |
| Dull | 1 (3.9%) | 0 (0%) | 1 (1.7%) |
| Pain severity |
| 1-3 | 6 (23.1%) | 9 (26.4%) | 15 (25%) | 0.1357 |
| 4-6 | 18 (69.2%) | 22 (64.7%) | 40 (66.7%) |
| 7-10 | 2 (7.7%) | 3 (8.9%) | 5 (8.3%) |
| Others |
| Trigger factors | 24 (92.3%) | 30 (88.2%) | 54 (90%) | 0.6023 |
| Acute spontaneous pain | 24 (92.3%) | 33 (97%) | 57 (95%) | 0.8751 |
| Previous dental treatment/procedure | 18 (69.2%) | 20 (58.8%) | 38 (63.3%) | 0.4701 |
| No sensory findings | 24 (92.3%) | 31 (91.1%) | 55 (91.6%) | 0.6023 |
*Analysis was using Pearson’s chi-square test
About 26 patients (43.3%) were in the age group 55-64 years. Of the total 34 females in the study group, 15 (44.1%) were in 55-64 year age group [Table/Fig-2].
Based on the MRI findings 31 patients (51.7%) showed neurovascular compression with atrophy or displacement in the trigeminal nerve root (Classical trigeminal Neuralgia). MRI of five patients (8.4%) revealed- Schwannoma (1), Meningioma (1), Demyelination (2) and Infarct (1) (Secondary trigeminal neuralgia). About 24 (39.9%) had normal MRI findings (Idiopathic trigeminal neuralgia). In the study, hypoesthesia was the only sensory examination finding found in all the five patients of secondary trigeminal neuralgia. 90% of patients had trigger factors; the most common of which were touch (86.6%) and breeze (70%). Involvement of dual divisions (V2 and V3), absence of trigger factors and evidence of hypoesthesia were found in all patients of Secondary Trigeminal neuralgia (p<0.001) [Table/Fig-3].
Correlation between clinical features and subtypes.
| Type | Classical (n=31) | Secondary (n=5) | Idiopathic (n=24) | Total (n=60) | *p-value |
|---|
| Side of face |
| Left | 13 (41.9%) | 3 (60%) | 8 (33.3%) | 24 (40%) | 0.5150 |
| Right | 18 (58.1%) | 2 (40%) | 16 (66.7%) | 36 (60%) |
| Division of nerve |
| V2 | 20 (64.5%) | 0 (0%) | 5 (20.8%) | 25 (41.7%) | <0.001 |
| V3 | 11 (35.5%) | 0 (0%) | 8 (33.3%) | 19 (31.7%) |
| V2+V3 | 0 (0%) | 5 (100%) | 11 (45.9%) | 16 (26.6%) |
| Pain radiation |
| Within the division | 31 (100%) | 0 (0%) | 13 (54.1%) | 44 (73.3%) | 0.9116 |
| Outside the division | 0 (0%) | 5 (100%) | 11 (45.9%) | 16 (26.7%) |
| Pain character |
| Shock like/Lancinating | 31 (100%) | 2 (40%) | 24 (100%) | 57 (95%) | 0.0856 |
| Throbbing | 0 (0%) | 2 (40%) | 0 (0%) | 2 (3.3%) |
| Dull | 0 (0%) | 1 (20%) | 0 (0%) | 1 (1.7%) |
| Pain severity |
| 1-3 | 8 (25.8%) | 3 (60%) | 4 (16.6%) | 15 (25%) | 0.1510 |
| 4-6 | 20 (64.5%) | 1 (20%) | 19 (79.1%) | 40 (66.7%) |
| 7-10 | 3 (9.7%) | 1 (20%) | 1 (4.3%) | 5 (8.3%) |
| Others |
| Trigger factors | 31 (100%) | 0 (0%) | 23 (95.8%) | 54 (90%) | <0.0001 |
| Acute spontaneous pain | 31 (100%) | 2 (40%) | 24 (100%) | 57 (95%) | 0.1673 |
| Previous dental treatment/procedure | 20 (64.5%) | 0 (0%) | 18 (75%) | 38 (63.3%) | 0.0636 |
| No Sensory findings | 31 (100%) | 0 (0%) | 24 (100%) | 55 (91.6%) | <0.0001 |
*Analysis was using Pearson’s Chi-squared test; p<0.05 was considered statistically significant
Discussion
Trigeminal neuralgia, though uncommon is a disturbing and disabling pain disorder. Despite a typical clinical presentation, it can sometimes be missed in an outpatient setting.
In the study, among the 60 patients studied with trigeminal neuralgia, 56.7% were females. The median age among males was 52.4 years and females were 56.5 years. Most common age group was between 55-65 years. In the study by Rai A et al., 55% were males, with average age of 58.97 years for males and 59.96 years for females [8]. Maarbjerg S et al., did a prospective systematic study of clinical characteristics in 158 patients. The prevalence of women (60%) was significantly higher than that of men with average age of onset 52.9 years [9]. In the study by Katheriya G et al., peak age of onset was between the 5th and the 6th decades of life. Females (59.2%) were more predilected for neuralgia than males [10]. These studies results were in agreement with present study results.
In the present study, right side of the face was more commonly involved than the left. Both sides were equally affected in the study by Rai A et al., [8]. In most of the studies, it has been observed that the right side of the face was affected more frequently than the left side [9,10].
Regarding the division of trigeminal nerve involved, it was found that maxillary (V2) and mandibular (V3) divisions were involved in 25 (41.7%) and 19 (31.7%) patients, respectively, while in remaining 16 (26.6%) patients, both V2 and V3 nerves were involved. The result was in consistent with the study by Rai A et al., [8]. Mandibular nerve was more commonly involved in the study by Katheriya G et al., [10]. However, all these studies had same observation that the combinations of V2+V3 were less common as similar to present study.
The diagnosis of trigeminal neuralgia is highly dependent on the character, duration and severity of the pain. In the study, the most commonly described character was shock like/lancinating (95%) with a severity of 4-6 (66.7%) on the Numerical pating pain scale. The most common pain descriptor was shock like pain in Rai A et al., study, stabbing pain in Maarbjerg S et al., study and sharp pain in Jainkittivong A et al., study [8,9,11].
Sensory findings (hypoesthesia) were observed in 8.4% patients. The most common trigger factors in the study were touch and breeze. In the study by Maarbjerg S et al., chewing and touch were the most common trigger factors and significant proportion of surgery naïve patients had sensory abnormalities [9].
The pain of trigeminal neuralgia is sometimes falsely attributed to dental origin [12]. In the study, previous dental treatment/procedure was undertaken by 63.3% of patients. In the study by Rai A et al., 13.33% underwent dental treatment [8]. Furthermore, Jainkittivong A et al., described that many patients with trigeminal neuralgia have lost teeth because of unnecessary extractions; odontogenic pain being a common misdiagnosis [11]. Thus, serious caution should be taken in cases where it may be perceived initially as an episodic toothache.
In the present study based on MRI correlation, Classical trigeminal neuralgia was the most common sub type that showed neurovascular compression with atrophy or displacement of trigeminal nerve root [Table/Fig-4]. In the study by Masur H et al., about 33.3% of patients had no neurovascular contact in MRI [13]. In a study by Nevan G et al., 62% had vessels seen abutting, or immediately adjacent to the trigeminal nerve on the side of their symptoms [14]. Analysis by Antonini G et al., showed that trigeminal root entry zone neurovascular contact was detected in 76% of symptomatic nerves [15].
MRI 3D-CISS axial image showing neurovascular impingement of right trigeminal nerve.
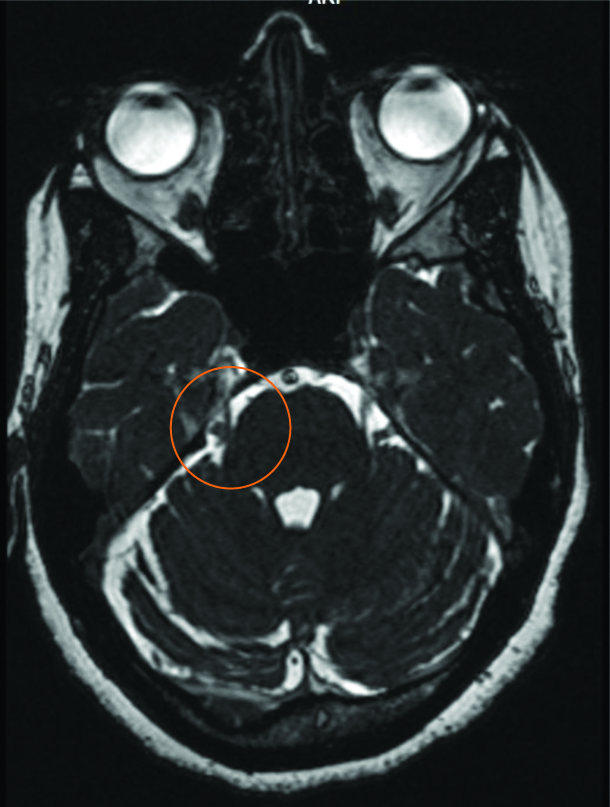
In present study, when the clinical features were compared between the various three subtypes, division of trigeminal nerve, trigger factors and no sensory findings were found to be statistically significant. Involvement of dual divisions (V2 and V3), absence of trigger factors and evidence of sensory finding were suggestive of Secondary Trigeminal neuralgia.
Limitation(s)
The greatest limitation of the study was the retrospective design and the conclusions were based on observation from a single study centre. Also, the sample size was relatively low. Thus, a prospective multicentre study is required.
Conclusion(s)
Trigeminal neuralgia though uncommon is a treatable cephalalgia which can have a major impact on the quality of life. The study determined the general clinical characteristics and MRI findings among trigeminal neuralgia patients. The common demographic and clinical features include female pre-ponderance, right side presentation, maxillary nerve division distribution, shock/lancinating pain with touch and breeze as common trigger factors. As some of them had a previous dental treatment or procedure, dentists need to be aware of this entity. Classical trigeminal neuralgia was the most common subtype. Involvement of dual divisions (V2 and V3), absence of trigger factors and evidence of sensory finding were more suggestive of Secondary Trigeminal neuralgia.
*Analysis was using Pearson’s chi-square test
*Analysis was using Pearson’s Chi-squared test; p<0.05 was considered statistically significant