Plasma Cell Rich Osteomyelitis: A Rare Entity
Prakhar Maheshwari1, Rajesh Kumar Maheshwari2, Anuradha Kusum3, Digvijay Agarwal4
1 Junior Resident, Department of Orthopaedics, Himalayan Institute of Medical Sciences, Dehradun, Uttarakhand, India.
2 Professor, Department of Orthopaedics, Himalayan Institute of Medical Sciences, Dehradun, Uttarakhand, India.
3 Professor, Department of Pathology, Himalayan Institute of Medical Sciences, Dehradun, Uttarakhand, India.
4 Assistant Professor, Department of Orthopaedics, Himalayan Institute of Medical Sciences, Dehradun, Uttarakhand, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rajesh Kumar Maheshwari, Himalayan Institute of Medical Sciences, Dehradun-248140, Uttarakhand, India.
E-mail: prakharmaheshwari80@gmail.com; rajesh1969m@yahoo.co.in
Plasma cell rich osteomyelitis is a rare finding characterised by a plethora of plasma cells localised in the affected bone without the typical clinical features of infection. It usually affects the metaphysis of long bones with a radiological appearance as a dense thickening of bone without sequestrum formation. We present an atypical case of plasma cell osteomyelitis with a lesion in the metaphysis as well as the diaphysis of the humerus without sclerosis but with sequestrum formation. An 11-year-old girl was brought to OutPatient Department (OPD) with complaints of post-traumatic pain and swelling at left shoulder and proximal arm since one and a half months with aggravation of symptoms since last 10 days. Patient had also been treated for Urinary Tract Infection (UTI) by a paediatrician who prescribed antibiotics and antipyretics because of which fever subsided but the pain persisted. The x-ray of left shoulder with arm revealed a fracture of surgical neck of humerus with cortical irregularity noted in the mid-shaft of humerus along with lamellated periosteal reaction suggestive of post-traumatic osteomyelitis with a pathological fracture. Clinicoradiologic diagnosis of pathological fracture of left neck of humerus was made with an underlying neoplastic or infective aetiology. An open biopsy was taken from left proximal humerus. Histopathological examination showed plasma cells in sheets having abundant basophilic cytoplasm, round to eccentric nuclei and perinuclear hoff along with lymphocytes and few polymorphs with surrounding area showing fibrosis, oedema and hyperemia. A diagnosis of chronic plasma cell osteomyelitis was rendered, which is an uncommon condition without specific clinical findings and an ambigious cause. Histopathology is the definitive tool for obtaining an accurate diagnosis and we strongly recommend a meticulous histopathological examination correlated with clinico-radiological description for a correct diagnosis in order to avoid an increased frequency of diagnosis of neoplastic plasma cell lesion as well as for advocating the correct treatment. This case is discussed for presentation of plasma cell osteomyelitis and also to report a case of chronic primary plasma cell rich osteomyelitis with atypical clinical features.
Immunolabelling, Plasmacytoma, Sclerosis
Case Report
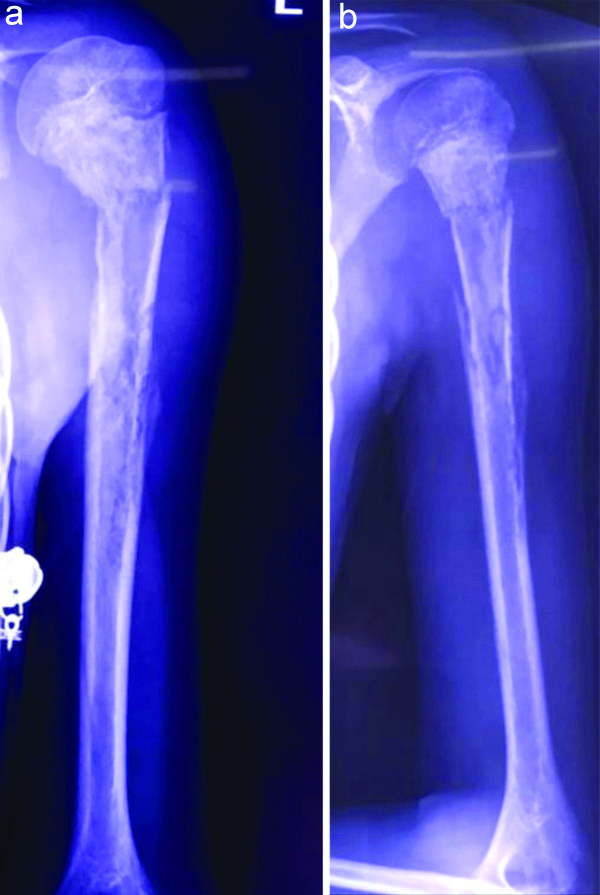
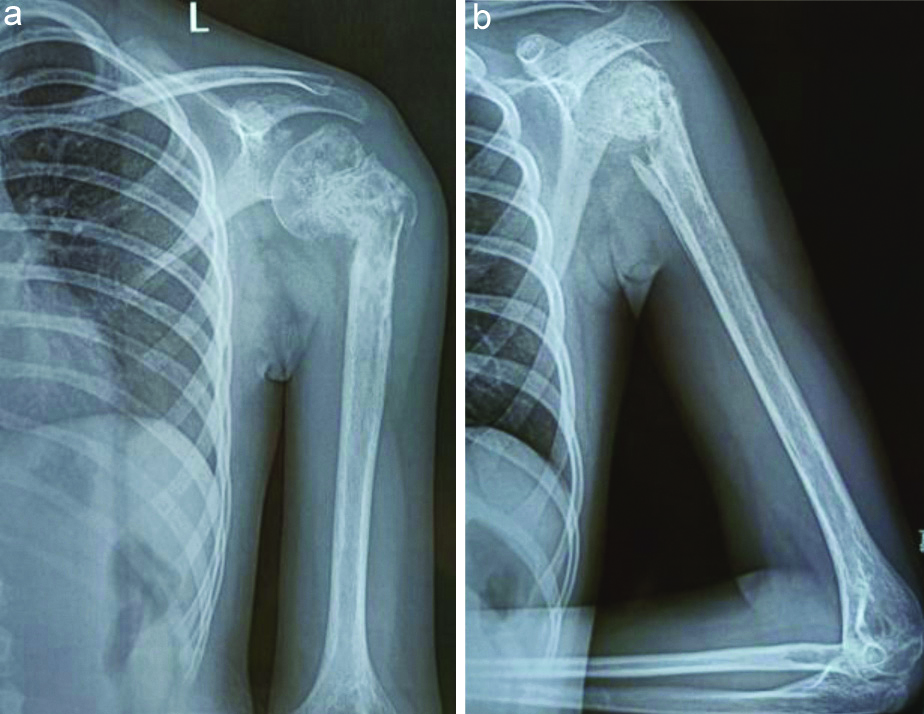
An 11-year-old girl was brought to the Orthopaedics OPD with complaints of pain and swelling at left shoulder and proximal arm since one and a half months following a trivial trauma with aggravation of aforementioned symptoms in the past 10 days. A history of on and off low grade fever for two months was present. A local examination revealed a diffuse circumferential swelling present over left shoulder and proximal arm. Soft tissue over shoulder and proximal arm did not show any signs of involvement. A local rise of temperature and tenderness was appreciated over proximal third of left arm with an abnormal mobility at surgical neck of humerus. Bony irregularity was palpated at the diaphyseal region of left humerus. The movements at left shoulder were extremely painful and distal neurovascular status was intact. Radiographs showed a fracture of the surgical neck of humerus with cortical irregularity noted in the mid shaft of humerus along with lamellated periosteal reaction as shown in [Table/Fig-1a,b].
a,b) X-ray suggestive of fracture of surgical neck of humerus with cortical irregularity and periosteal reaction in diaphyseal region, a) Anteroposterior view and b) Lateral view.
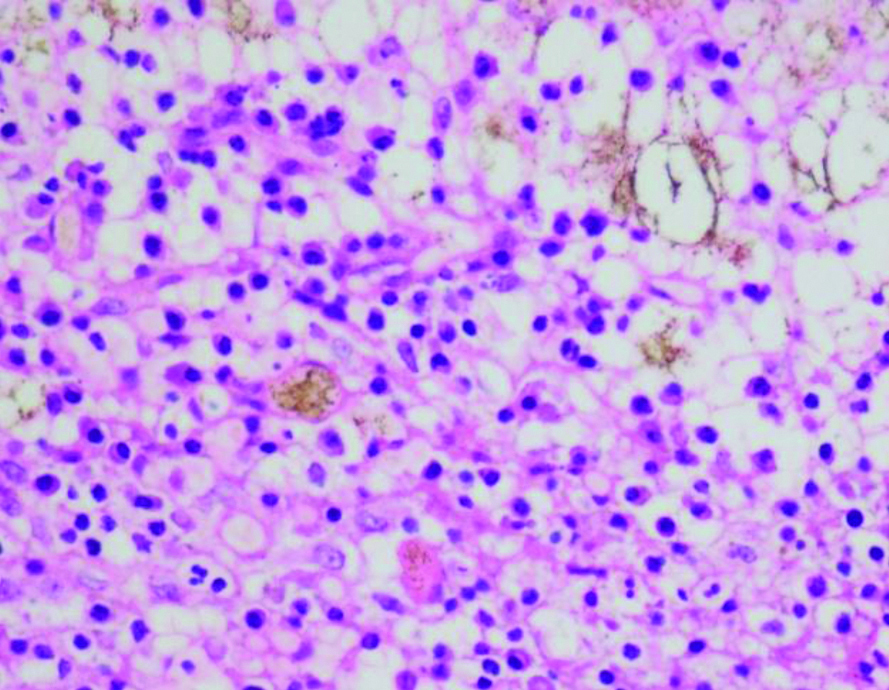
Laboratory blood investigations revealed a normal total leucocyte count with 48.5% neutrophils, 41% lymphocytes, 3.8% eosinophils, 0.2% basophils and an Erythrocyte Sedimentation Rate (ESR) of 17 mm/hr. A differential diagnosis was made including Ewing’s sarcoma and osteomyelitis of proximal humerus. A differential diagnosis of osteosarcoma was ruled out in view of absence of its classical radiology and on basis of clinical parameters in index case. A core biopsy from the lesion was performed and specimen was sent for histopathological examination, culture-sensitivity and cartridge-based nucleic acid amplification testing. Cartridge-based nucleic acid amplification testing report was negative for Mycobacterium tuberculosis. Gross specimen examination revealed multiple greyish-brown to greyish-white soft to bony tissue pieces together measuring 8×7×2 mm received and decalcification done, prior to routine processing. On light microscopic examination, Haematoxylin and Eosin (H&E) stained sections exhibited bony trabeculae, with intervening tissue showing many plasma cells having abundant basophilic cytoplasm, perinuclear hoff, round to eccentric nuclei along with lymphocytes and few polymorphs. Surrounding area showed fibrosis, oedema and hyperaemia with no evidence of malignancy [Table/Fig-2].
Light microscopy showing abundance of plasma cells characterised by blue rounded cells (H&E:X400).
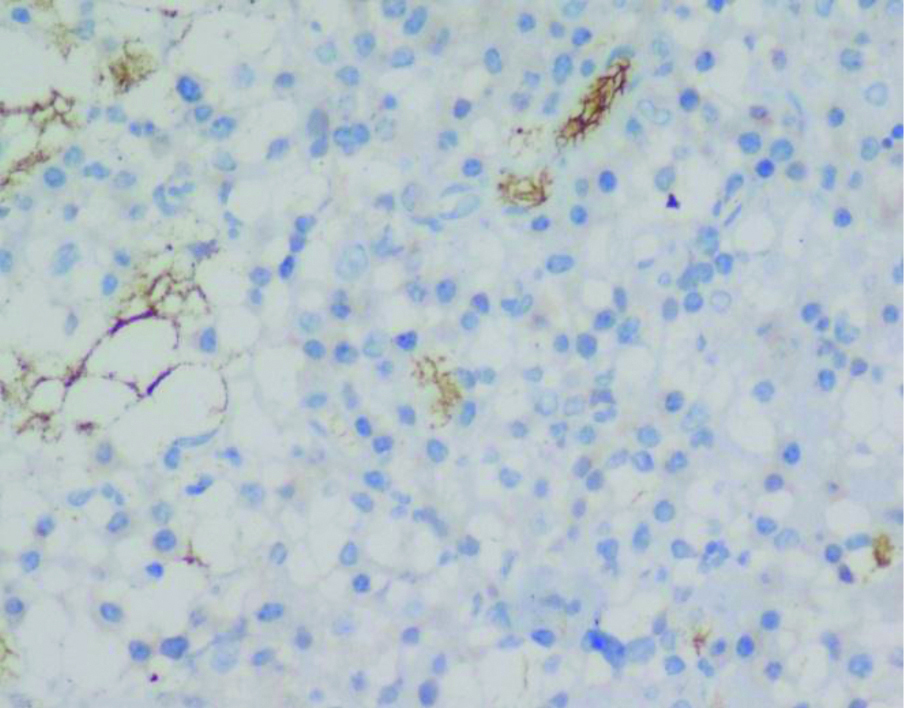
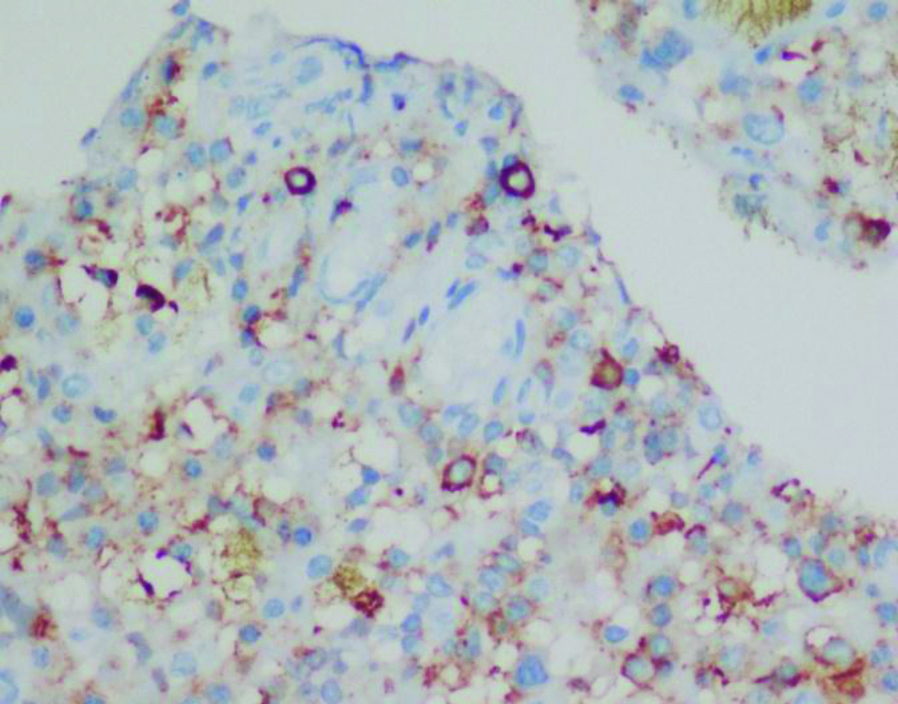
Based on light microscopy, provisional diagnosis of a plasma cell rich lesion was made with advice for further immunohistochemistry tests to rule out neoplastic conditions like Ewing’s sarcoma as it contained round cells which are similar to a plasmacytoma picture. Immunohistochemistry was performed with two markers: CD99, CD138 where lesion was found negative for CD-99 suggesting negativity for Ewing’s sarcoma while a positive expression for CD-138 indicating plasma cell presence [Table/Fig-3,4].
Absence of brown granules in cytoplasm suggestive of negativity for CD99 marker (IHC CD99:X400).
Presence of brown granules in cytoplasm suggestive of positivity for CD138 marker (IHC CD138:X400).
Sample was sent to the microbiology laboratory for culture and revealed growth of Staphylococcus aureus. Patient was given a U-slab splintage for six weeks, prescribed antibiotics based on culture sensitivity along with Non Steroidal Anti-Inflammatory Drugs (NSAIDs) and at six weeks follow-up post-biopsy, fracture union was appreciated [Table/Fig-5a,b] and patient advised to continue with splintage for further protection of the bone.
X-ray suggestive of signs of union in progress in a varus tilt, a) Anteroposterior view and b) Lateral view.
Discussion
Plasma cell osteomyelitis is a primary localised chronic haematogenous osteomyelitis with a clinically vague onset [1]. Good literature is available on sclerotic osteomyelitis of Garre and Brodie’s abscess but only scarce literature is available describing plasma cell osteomyelitis with no data describing its occurrence rate. It is thought to develop when body’s resistance is good and virulence of organism is restricted. Plasma cell osteomyelitis usually affects children and young adults, the most commonly involved site being the metaphysis of a long bone [2]. The male to female ratio is 3:2 [1] however, index case was of a female. The clinical course is slow and inactive with occasional symptoms of common cold with fever, especially of tonsillitis or sinusitis [1]. In a case reported by Reddy M et al., atypical features like involvement of the diaphysis and sequestrum formation were demonstrated [3]. Typical radiological picture as described in other case reports [3,4] appears to be sclerotic in nature in contrast to index case which exhibited no sclerosis on radiological assessment as well as lamellated periosteal reaction because of which a differential diagnosis of Ewing’s sarcoma was kept in mind. In index case, there was involvement of the metaphysis as well as the diaphysis of left humerus along with a pathological fracture at the surgical neck. The minimal soft tissue involvement compounded with radiological findings created a diagnostic dilemma oscillating between infective and neoplastic aetiologies. Although metaphysis is a common location for osteomyelitis in young age, a neoplastic condition like Ewing’s sarcoma cannot be excluded without a histopathological confirmation in this age. Exner described three distinctive zones on the basis of light microscopy, composed of infiltration of plasma cells with granulation tissue at the centre of the inflammatory focus (central zone), proliferation of fibrous tissue surrounding the centre (intermediate zone) and fibrous bone marrow with protein-rich fluid in the margin of the focus (peripheral zone) [1]. In a solitary plasmacytoma, the histological findings in the central and peripheral areas reveal a monotonous appearance, in which occasionally plasma cells are poorly differentiated with bizarre cells, and bone trabeculae show only process of destruction. It is sometimes, however, difficult to differentiate plasma cell osteomyelitis and plasma cell myeloma (solitary plasmacytoma) microscopically [1]. In index case, the pathologist reported presence of bony trabeculae, with intervening tissue showing many plasma cells. On immunohistochemistry, this case showed positivity for CD 138 confirming a plasma cell aetiology while being negative for CD 99 which excludes the diagnosis of Ewing’s sarcoma. Although the aetiology in many cases remains vague, the leading theory seems to suggest an occult infection, but on review of literature, culture positivity in only 8% of cases has been found in lesions involving bones other than the mandible [3]. Sampling errors or the sluggishness of the process may contribute to the low incidence of culture positivity [5]. Staphylococcus aureus has been proved as the causative organism in many cases as was found in index case [1]. A study suggested that the term “primary chronic osteomyelitis” should be used for this type of osteomyelitis making it possible to differentiate the condition from acute and secondary osteomyelitis as well as from other conditions, such as bone tumours [6]. This case of plasma cell osteomyelitis was atypical for reasons like involvement of both metaphysis as well as diaphysis and an absence of history of pus discharge. Few cases described in literature were mistaken for a malignant bone tumour and were treated with wide resection and bone grafting [1].
Conclusion(s)
In the event of a diagnostic dilemma, histopathology and immunochemistry is the only definitive tool for obtaining an accurate diagnosis to differentiate between a benign and malignant condition. It shows the importance of biopsy before proceeding with definitive treatment. Knowledge of this condition can give a better outcome, avoiding unnecessary investigations and procedures while preventing an overly increased frequency of diagnosis of Ewing’s sarcoma.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Aug 22, 2020
Manual Googling: Oct 21, 2020
iThenticate Software: Oct 28, 2020 (8%)
[1]. Yasuma T, Nakajima Y, Clinicopathological study on plasma cell osteomyelitisActa Pathol Jpn 1981 31:835-44.10.1111/j.1440-1827.1981.tb02808.x7304172 [Google Scholar] [CrossRef] [PubMed]
[2]. Adler CP, Inflammatory conditions of the bone: Bone diseases, Macroscopic, Histological, and Radiological Diagnosis of Structural Changes in the Skeleton 2013 New YorkSpringer [Google Scholar]
[3]. Reddy M, Kumar AV, Avinash GS, Surendra Y, A rare case of plasma cell osteomyelitis with a typical presentationInt J Res Orthop 2020 6:227-29.10.18203/issn.2455-4510.IntJResOrthop20195822 [Google Scholar] [CrossRef]
[4]. Gupta S, Gupta AK, Goyal T, Gupta P, Rao S, Plasma cell osteomyelitis: A rare entityJCDR 2019 13(7):ED05-ED06.10.7860/JCDR/2019/41712.12972 [Google Scholar] [CrossRef]
[5]. Kang L, Millett PJ, Mezera K, Weiland AJ, Chronic plasma cell osteomyelitis of the humerus associated with Shigella and FlavobacteriumJ Shoulder Elbow Surg 2001 10:292-94.10.1067/mse.2001.11308411408914 [Google Scholar] [CrossRef] [PubMed]
[6]. Jani L, Remagen W, Primary chronic osteomyelitisInt Orthop 1983 7(2):79-83.10.1007/BF002664556543824 [Google Scholar] [CrossRef] [PubMed]