A Rare Case of Adult-onset Best Disease
Siddharam S Janti1, Shinisha Damodaran Paul2, Stephen Sudhakar Karunakaran3
1 Professor, Department of Ophthalmology, Chettinad Hospital and Research Institute, Chennai, Tamil Nadu, India.
2 Assistant Professor, Department of Ophthalmology, Chettinad Hospital and Research Institute, Chennai, Tamil Nadu, India.
3 Head and Professor, Department of Ophthalmology, Chettinad Hospital and Research Institute, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Shinisha Damodaran Paul, 3/23, United Colony, Medavakkam, Chennai-600100, Tamil Nadu, India.
E-mail: shinishapaul@gmail.com
Best Disease also known as Vitelliform Macular Dystrophy (VMD), classically presents with defective central vision. Macula which is responsible for the central vision and colour perception is affected. Individuals affected by Best disease, initially have normal vision followed by decrease in central visual acuity as well as metamorphopsia. The case presented a 49-years-old female with complaints of progressive and painless defective Vision of her Left Eye (LE) with previous history of diabetes. A well-circumscribed single greyish lesion of size 0.5DD was noted in the macula, which was conformed to be Best disease.
Choroidal neovascular membrane, Defective central vision, Vitelliform macular dystrophy
Case Report
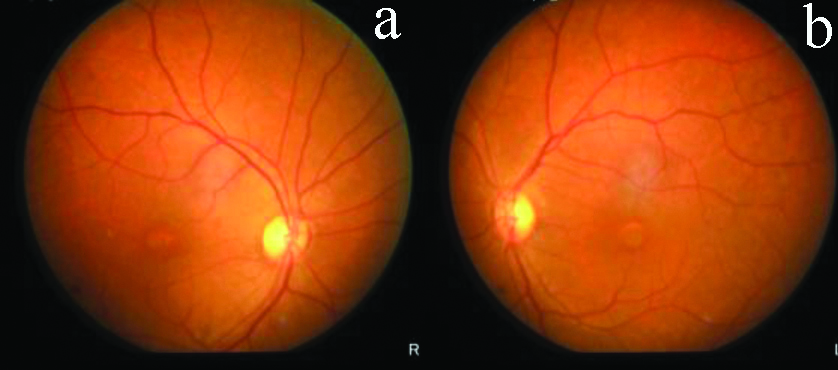
A 49-years-old female presented with complaints of progressive and painless defective vision of her Left Eye (LE) over a period of 8 months. There was no history of trauma or any other associated symptoms. The patient was known diabetic for three years. On examination, eyes were orthophoric. Both eyes had clear cornea, normal anterior chamber depth, normal iris pattern and clear lens. Visual acuity in her Right Eye (RE) was 6/9 improving to 6/6 and LE was 6/24 improving to 6/12. Colour Vision was normal. Fundus examination revealed normal disc and vessels in both the eyes. A well-circumscribed single greyish lesion of size 0.5DD was noted in the macula (LE>>RE) [Table/Fig-1a,b]. The rest of retina and peripheral retina was normal.
Fundus photo of RE and LE showing well-circumscribed lesion in the macula.
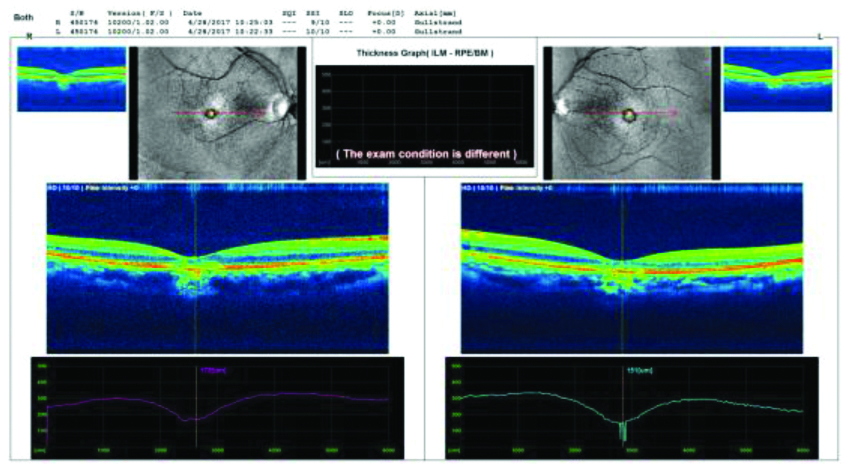
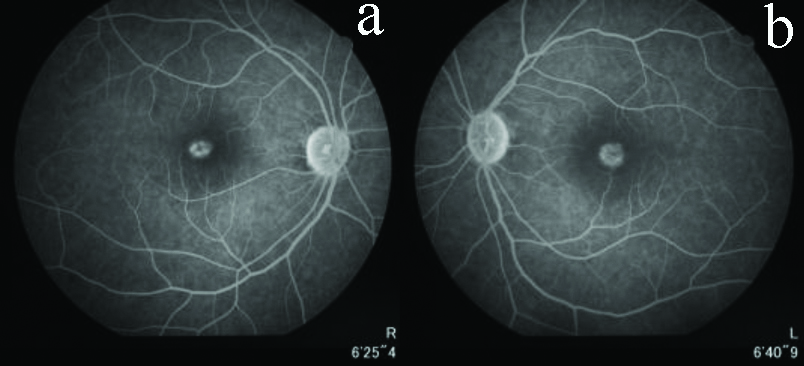
Routine blood investigations and systemic investigations were normal. Optical Coherence Tomography (OCT) was done which showed discontinuity of Retinal Pigment Epithelial (RPE) membrane and ellipsoid layer with Sub RPE deposits as shown in [Table/Fig-2]. Fundus Fluorescence Angiography (FFA) of both the eye showed normal disc and an area of hyperfluorescent center with hyperfluorescent borders at the macula in early phase with total hyperfluorescence in late phase. The rest of the retina appeared normal [Table/Fig-3a,b]. The patient was subjected to Electro-oculogram (EOG). EOG showed decrease in Arden Ratio of 1.3. Based on these findings, diagnosis of Adult-onset Best disease was made. The patient is on follow-up to identify any development of Choroidal Neovascular Membrane (CNVM) and there is no cure for this disease.
Optical Coherence Tomography (OCT) showing discontinuity of RPE and ellipsoid layer with Sub Retinal Pigment Epithelial (RPE) deposits.
Fundus Flourescein Angiography (FFA) showing hypofluorescent center with hyperfluorescent borders at macula.
Discussion
Best Vitelliform macular dystrophy is an autosomal dominant disease with variable penetrance [1]. Defect in the long arm of chromosome 11 (11q12-q13) has been linked to the disease [2]. Petrukhin K et al., first identified the retina-specific gene and designated it as VMD2 [3]. Protein which is encoded by this gene was proposed as bestrophin. The disease starts at the age of 3-15 years but usually is detected later, since there is no significant vision loss. The macula has abnormal deposits of lipofuscin pigment which was described by Weingeist TA et al., [4]. In the initial stages of the disease, a bright yellow cyst forms in the RPE beneath the macula which shows sunny-side-up egg appearance on fundus examination. Visual acuity may be normal or near normal. Peripheral vision remains unaffected throughout the progression of the disease.
If the cyst ruptures, fluid and yellow deposits from the cyst spreads throughout the macula, giving the appearance of scrambled egg. Further, there is atrophy of the macula and underlying RPE which leads to further deterioration of central vision.
The clinical stages have been described as follows:
Stage 0: Normal macula but Abnormal Electro-oculography (EOG)
Stage 1: RPE disruption in the macular region and FFA showing window defects.
Stage 2: A well-circumscribed, circular, yellow-opaque, homogeneous yolk-like macular lesion. FFA reveals marked hypofluorescence in the zone covered by the lesion.
Stage 2a: The contents become less homogeneous and develop a “scrambled-egg” appearance. FFA shows partial blockage of the fluorescence with non-homogeneous hyper fluorescence.
Stage 3: The lesion develops a fluid level of a yellow-coloured vitelline substance. FFA shows inferior hypofluorescence from the blockage by the vitelline material, along with superior hyperfluorescent defects.
Stage 4a: The lesion has typical orange-red colour with atrophic RPE and visibility of the choroid. FFA shows hyper fluorescence without any leakage.
Stage 4b: Fibrous scarring of macula. FFA shows hyperfluorescence without any leakage.
Stage 4c: Choroidal neovascularisation or appearance of subretinal haemorrhage. FFA shows hyperfluorescence as a result of neovascularisation and leakage.
Electro-oculogram is the diagnostic test for Best disease which shows decrease in Arden ratio, the normal value being 1.5. This can differentiate Best disease from Adult-onset Vitelliform Macular Dystrophy in which the Arden ratio will remain normal. The disease has variable prognosis. Some carriers never express their phenotype, while few others maintain better than 20/40 vision in both eyes. In one study, 88% of the patients retained 20/40 or better visual acuity and only 4% of the patients had 20/200 or worse visual acuity in the better eye.
There is no known treatment for the disease [5]. The patient has to be observed for development of any CNVM which can cause dramatically decreased vision. It is important to establish the correct diagnosis and monitor this condition. Comprehensive ocular examination of the patient’s family members to rule out any early signs of this rare eye condition is recommended.
Conclusion(s)
Hence, the case was presented for its rarity, since Best disease occurs at early stages of life whereas this patient presented as adult, time of onset of best disease. One should also be aware of the importance of EOG as it can confirm various retinal disorder.
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? NA
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: May 06, 2020
Manual Googling: Sep 24, 2020
iThenticate Software: Oct 28, 2020 (4%)
[1]. Deutman AF, Hoyng CB, Macular Dystrophies. In: Schachat AP, Hengst TC, editorsMedical Retina 2001 3rd edMosbyLondon:1226 [Google Scholar]
[2]. Stone EM, Nichols BE, Sterb LM, Kimura AE, Sheffield VC, Genetic linkage of vitelliform macular degeneration to chromosome 11q13Nat Genet 1992 1:246-50.10.1038/ng0792-2461302019 [Google Scholar] [CrossRef] [PubMed]
[3]. Petrukhin K, Koisti MJ, Bakall B, Li W, Identification of the gene responsible for Best’s macular dystrophyNature Genet 1998 19:241-47.10.1038/9159662395 [Google Scholar] [CrossRef] [PubMed]
[4]. Weingeist TA, Kobrin JL, Watzke RC, Histopathology of Best’s macular dystrophyArch Ophthalmol 1982 100:110810.1001/archopht.1982.010300400860167092654 [Google Scholar] [CrossRef] [PubMed]
[5]. Chowers I, Tiosano L, Audo I, Grunin M, Boon CJ, Adult-onset foveomacular vitelliform dystrophy: A fresh perspectiveProgress in Retinal and Eye Research 2015 47:64-85.10.1016/j.preteyeres.2015.02.00125681578 [Google Scholar] [CrossRef] [PubMed]