Demineralisation and dental caries around orthodontic brackets is a significant problem faced by the patients undergoing fixed appliance therapy as well as by the clinician. Fixed orthodontic treatment creates retentive areas around brackets for the accumulation of food debris which successively leads to enamel demineralisation and dental caries [1]. The accumulation of plaque around the orthodontic bracket brings about demineralisation of enamel which is the earliest macroscopic evidence of caries [2]. Dental plaque is mainly composed of acid-producing bacteria which lowers the pH around the brackets and makes the teeth susceptible to dental caries and demineralisation [3]. Enamel demineralisation initially appears as white spot lesions occurring in the subsurface region, thereby leaving approximately 10-30 μm of enamel intact due to supersaturation of fluorapatite. As a result, this subsurface demineralisation causes a change in the refractive index of enamel and manifests clinically as a milky white opacity or also known as white spot lesions [4].
Oral hygiene becomes more difficult in patients undergoing fixed orthodontic treatment and decalcification of the enamel surface adjacent to these appliances is frequent. If they are left untreated, they progress to produce carious cavitation, and presents as aesthetic problems [5]. These white spots can also be seen one month after fixed appliances and in some patients even after 6 or 12 months [6]. There are various methods of detecting enamel demineralisation, such as the visual-tactile method which is the most commonly used. The other non-invasive technique to detect white spot lesions is Quantitative Light-induced Fluorescence (QLF), DD, Fibreoptic Transillumination (FOTI) and Electrical Conductance (EC) [7]. Elastomeric ligatures which are most commonly used to hold the archwire in the slot, can promote plaque accumulation around it leading to enamel demineralisation. The use of self-ligating brackets eliminates the accumulation of plaque around it as the ligating system is incorporated into the bracket [8]. Therefore, the aim of the present study was to quantify and compare enamel demineralisation scores using DD in subjects undergoing orthodontic treatment with passive self-ligation brackets and conventional brackets at various time intervals.
Materials and Methods
This prospective study was conducted in a university hospital setting. Adult subjects aged 20 to 35 years who were undergoing orthodontic treatment at the Department of Orthodontics, Saveetha Dental College were selected for this study. The study was started by January 2019 and completed by March 2020 and the total duration of the study was one year and two months, but the patients were evaluated for a year only. Ethical clearance to conduct this study was obtained from the Scientific Review Board of the hospital (SRB/SDC/MDS/002/01). Informed consent was taken prior to starting orthodontic treatment. Type of malocclusion and the level of crowding was not considered while recruiting the study subjects.
Inclusion Criteria
Adult patients (20-35 years) scheduled for 022 MBT (3m Gemini brackets) or passive self-ligation (Damon 3mx, Ormco)
Patients with a full complement of teeth all types of malocclusion cases were included.
Exclusion Criteria
Patients with fluorosis, enamel hypoplasia and other anomalies of tooth number and morphology.
Sampling
A total of 19 subjects scheduled for orthodontic treatment starting from January-February 2019 were randomly and equally allotted to either of the two groups. No specific randomisation technique was followed and the choice of the appliance was entirely based on patient’s willingness. A total of 57 teeth in the 19 patients were evaluated for demineralisation. The tooth numbers selected in an individual patient were 13, 11 and 23. A total of 27 anterior teeth were included in the control group (conventional ligation, 3m Gemini MBT brackets) and 30 were included in the experimental group (self-ligation group, Damon 3mx Ormco). All patients underwent standard orthodontic bonding protocols like scaling and polishing before the placement of brackets and the same bonding system was used in both groups.
In the conventional group, elastomeric modules (Ormco) were used for securely ligating the arch wire to the brackets. At monthly intervals, oral hygiene instructions were reinforced but plaque scores were not checked. The sample size was calculated using G*Power analysis version 3.1.9.4 with the power of 0.95 based on the study conducted by Polat O et al., with the effect size set at 0.94 [9].
Enamel demineralisation scores recorded with DD were taken at the time of bonding (T0), 3 months (T1) and 12 months (T2) into treatment. A technique similar to Staudt CB et al., was used to record the score. The sample teeth irrespective of whether carious or not were checked for demineralisation. Before carrying out the reading, DD calibration was carried out. The value in the display of DD had to agree with the reference value at 90° angle [Table/Fig-1,2 and 3]. Reference value is engraved on the surface of the calibration disk. The teeth were isolated with cotton rolls and air-dried for a few seconds; the DD pen (kavo, DD pen 2190) was placed on the tooth surface midway along the bracket sides (gingival, incisal, mesial, and distal). The tapered tip (tip A) was used at approximately 60 degrees to the tooth surface to allow measurement of the enamel closest to the bracket. The largest unit (maximum range, 0 to 99) was recorded for each of the four sides. Based on the manufacturer’s recommendations, readings <5 represent no lesions and values ≥5 to 99 represent increasing severity of lesions [10]. The individual scores of every tooth were added and a mean score for each patient was calculated. The recording of DD scores were all performed by the first author (AT) and to check the reliability of the measurements taken, the same author repeated the readings for 5 points after a one-week interval.
Calibrating the Diagnodent (DD) with the selection of probe tip to achieve specific zero baseline.

Calibration value in the display agrees with the reference value at 90° angle. Reference value is engraved on the surface of the calibration disk.
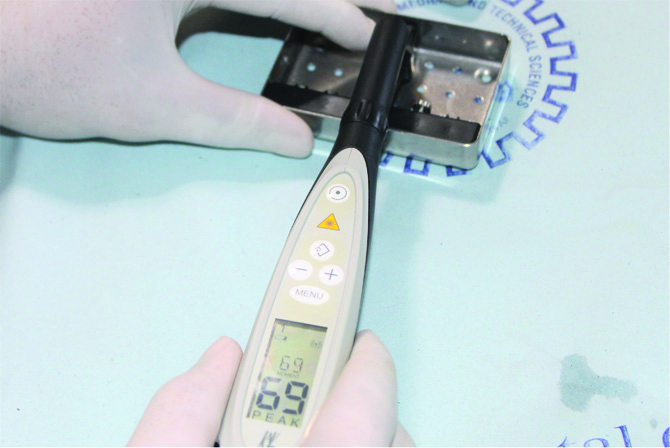
Representation of Diagnodent (DD) in patients’ mouth recording demineralisation score at T1.

Statistical Analysis
IBM Statistical Package for the Social Sciences (SPSS) version 20 was used for statistical analysis. The p-value was set at 0.05. Gender association was performed with chi-square test; one-way ANOVA test was carried out to evaluate the difference of mean DD scores at three time periods T0, T1 and T2 in both self-ligation group and conventional ligation group. Independent t-test was carried out to evaluate the difference of mean DD scores between self-ligation brackets and conventional ligation.
Results
The age range of subjects included in the study was 20-35 years; 9 males (27.44±2.4) and 10 females (26±0.9). [Table/Fig-4] represents the one-way ANOVA test indicating that in conventional ligation group, there was a statistically significant difference in the mean DD scores between T0 and T1 (p<0.05) and T0 and T2, statistically non-significant difference in the mean DD score between T1 and T2 (p>0.05) was noted. [Table/Fig-5] represents a one-way ANOVA test indicating that in the self-ligation group, a statistically significant difference was observed in the mean DD score between T0 and T1, T1 and T2 as well as T0 and T2 (p<0.05). [Table/Fig-6] represents Independent t-test to evaluate the difference of mean DD scores between self-ligation brackets and conventional ligation and it was found to be statistically non-significant at T0, T1 and T2 (p>0.05).
One-way ANOVA depicting the difference of mean Diagnodent (DD) scores at time period T0, T1 and T2 in conventional ligation group.
| Time period | Mean difference | Std. Error | Significance |
|---|
| Baseline (T0)- 3rd Month (T1) | -4.03 | 0.57 | <0.01 |
| 12th Month (T2) | -2.73 | 0.57 | <0.01 |
| 3rd Month (T1)- Baseline (T0) | 4.03 | 0.57 | <0.01 |
| 12th Month (T2) | 1.30 | 0.57 | 0.08 |
| 12th Month (T2)-Baseline (T0) | 2.73 | 0.57 | <0.01 |
| 3rd Month (T1) | -1.30 | 0.57 | 0.08 |
p<0.05 is statistically significant
One-way ANOVA depicting the difference of mean Diagnodent (DD) scores at time period T0, T1 and T2 in self- ligation group.
| Time period | Mean difference | Std. Error | Significance |
|---|
| Baseline (T0)-3rd Month (T1) | -4.35 | 0.32 | <0.01 |
| 12th month (T2) | -3.21 | 0.32 | <0.01 |
| 3rd Month (T1)-Baseline (T0) | 4.35 | 0.32 | <0.01 |
| 12th Month (T2) | 1.14 | 0.32 | 0.05 |
| 12th Month (T2)-Baseline (T0) | 3.21 | 0.32 | <0.01 |
| 3rd Month (T1) | -1.14 | 0.32 | 0.05 |
p<0.05 is statistically significant
Independent t-test depicting the difference of mean Diagnodent (DD) scores between self-ligation brackets and conventional ligation at T0, T1 and T2.
| Type of ligation time period | Mean±SD | Significance |
|---|
| Conventional ligation T0 | 0.16±0.10 | 0.14 |
| Self-ligation | 0.11±0.32 |
| Conventional ligation T1 | 4.19±1.81 | 0.69 |
| Self-ligation | 4.46±1.22 |
| Conventional ligation T2 | 2.89±1.22 | 0.30 |
| Self-ligation | 3.32±0.9 |
p<0.05 is statistically significant
[Table/Fig-7] represents a chi-square test to evaluate the difference of enamel demineralisation score between genders at the time period T0, T1 and T3. A statistically non-significant difference of DD scores at T0, T1 and T2 between genders (p>0.05) was noted.
Chi-square test to evaluate the association of gender with enamel demineralisation score at different time intervals.
| Time period | Chi-square value | p-value |
|---|
| T0 | 3.07 | 0.38 |
| T1 | 14.32 | 0.42 |
| T2 | 19.00 | 0.08 |
p<0.05 is statistically significant
The Cronbach’s test for intra-observer reliability (cronbach’s alpha=0.583) and it can be inferred that there was a moderate reliability when the measurements were repeated again by the same author.
Discussion
Passive self-ligation brackets have become very popular among orthodontists recently, there is a lot of literature on the various aspects of self-ligation, but literature on the effect on enamel demineralisation by the method of ligation is still lacking [11-14]. In the present study, an attempt was made to quantify the enamel demineralisation around passive self-ligation brackets and compare it with conventional brackets with elastomeric ligatures. It was observed that there was a statistically significant difference in the mean enamel demineralisation scores in both groups measured with DD between T0 and T1 as well as between T0 and T2 (p<0.05). Enamel demineralisation was higher at T2 in both groups compared to T0. Bonding of orthodontic brackets involves enamel etching and this leads to enamel demineralisation, hence it was sought to take the first measurement after 3 months (T1) and it was observed that at T1 there was significant demineralisation around brackets in both groups. At the end of 12 months (T2), enamel demineralisation was found more than the baseline values, but less than T1 values, hence it can be inferred that orthodontic bonding followed by treatment, subjects the teeth to demineralisation. Possible reasons can be acid etching and inadequate hygiene maintenance by the patients. The difference in DD scores to detect white spot lesions when compared between the two groups at the end of one year were not statistically significant (p>0.05). No significant association of white spot lesion occurrence with the gender of the patient was noted, hence other factors like oral hygiene maintenance and bacterial colonisation can be associated. Evaluation of plaque scores was not done at every visit but oral hygiene instructions were reinforced at every review visit.
A white spot appears as opaque, white coloured and smooth surface caries [15]. Gorelick L et al., reported that there was an increased prevalence of white spot lesions during treatment and it has been reported that 50% of the patients had one or more White Spot Lesions (WSLs) at the end of treatment [16]. In the present study, 8% of the total 57 teeth assessed had developed white spot lesions at the end of 12 months. It has been reported in the literature that different methods of ligation have an effect on the occurrence of white spot lesions [8,9,17,18]. According to Akin M et al., patients treated with self-ligation had a low prevalence of white spot lesions as compared to conventional ligation [17]. These findings are not in consensus with the present study as the white spot lesion incidence was reported at the end of one year rather than at the end of full treatment and DD was used in contrast to photographic assessment by Akin M et al. In contrast to the findings of Akin M et al., it was reported by Buck T et al., that the method of ligation does not have any effect on the occurrence of enamel demineralisation; rather proper oral hygiene instructions play a pivotal role [18] which is similar to the present study. The study by Buck T et al., is in consensus to the present study as the white spot lesions incidence was measured at one year into treatment and DD was used to assess WSLs development [18]. A study by Polat O et al., reported findings similar to the present study and concluded that there was no significant difference in terms of white spot lesion formation between the conventional straight wire and self-ligation brackets and that it largely depended on the patients’ oral hygiene status [9]. A study conducted by Park JH et al., observed that elastomeric rings encouraged non-significantly more plaque accumulation and significantly more demineralisation compared to similar brackets without elastomeric rings or self-ligating brackets but they did not evaluate demineralisation between conventional ligation and self-ligating brackets [8].
There are different methods of detecting an early enamel demineralisation like traditional visual inspection, radiography, fluorescence methods and electrical conductivity. The most common method used for detection is the visual inspection. Demineralisation of the enamel and microporosity affects the transmission of light within the enamel. Thus, the enamel layer loses its bright colour and appears opaque white due to optical refraction [19]. With the advent of DD in 1998, quantification of enamel demineralisation has become simple and accurate. The tooth surface is illuminated with laser light (wavelength of 655 nm) and some of this light is re-emitted as near-infrared fluorescent light. The tooth surface with increased bacterial by-products emits an increased fluorescent light and thus, the difference between sound and decayed areas are recognised. This instrument has a high sensitivity to detect and quantify incipient caries lesion [20]. However, there are few limitations of DD such as the diameter of the tip is large (>1 mm), inaccurate readings in the presence of stains, biofilms and composite resins. Also, limited accessibility to the embrasures can lead to inaccurate readings of interproximal surfaces [21,22]. In the present study, enamel demineralisation is quantified with the help of DD because of its high sensitivity and accuracy.
There is abundant literature available on the level of S. mutans around self-ligation and conventional ligation [23-26]. Pandis N et al., conducted a study to evaluate the level of salivary S. mutans around self-ligating brackets and conventional ligation. It was reported that there was no significant difference in the level of S. mutans between self-ligation and conventional ligation, but the enamel demineralisation was not measured with the help of DD [26]. Similarly, studies reported that bracket types did not have an effect on the S. mutans level [23-25,27].
Limitation(s)
Limitations of the present study include a limited sample size, oral hygiene assessment was not performed and age association on the incidence of white spot lesions was not a part of the study. A long-term assessment for the appearance of white spot lesions could not be performed in the study. The study recommend further randomised trials to assess enamel demineralisation over a longer period of time.
Conclusion(s)
The enamel demineralisation happens irrespective of the type of ligation. There is no difference in enamel demineralisation scores at the end of one year during orthodontic treatment, between self-ligation and conventional ligation, hence the method of ligation does not influence enamel demineralisation.
p<0.05 is statistically significant
p<0.05 is statistically significant
p<0.05 is statistically significant
p<0.05 is statistically significant