Effectiveness of Dry Needling and Low-Level Laser Therapy in Nonspecific Low Back Pain
Alagiathiruvevenkadam Ilayaraja1, MK Franklin Shaju2, Singh Sumer Singh3, Edwin Raj Gerald4, D Sathyanarayana5, R Ilayaraja Hema6
1 Assistant Professor, Department of Physiothearpy, Utar, Kajang, Selangor, Malaysia.
2 Professor, Department of Physiotherapy, RVS College of Physiotherapy, Coimbatore, Tamil Nadu, India.
3 Associate Professor, Department of Life Sciences, Singhania University, Pacheri Bari, Rajasthan, India.
4 Professor, Department of Physiotherapy, RVS College of Physiotherapy, Coimbatore, Tamil Nadu, India.
5 Senior Physiotherapist, Pain Clinic, Lakkshmi Physiotherapy Centre, Coimbatore, Tamil Nadu, India.
6 PG Assistant, Computer Science, Vikas International School, Madurai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Alagiathiruvevenkadam Ilayaraja, Kajang, Selangor, Malaysia.
E-mail: drilayaraja@gmail.com
Introduction
Musculoskeletal spinal disorders are an immense problem in industrialised societies resulting in tremendous personal and economic costs. Younger adults (30 to 60-year-old) are more likely to experience Low Back Pain (LBP) from the disc space or from back muscle strain or other soft tissue strain. Experiencing it earlier in life may lead to recurrent and chronic LBP in adulthood. Dry Needling (DN) which are utilised to treat low back torment in current patterns. Low Level Laser Treatment (LLLT) is utilised to treat LBP by concentrating on the trigger focuses.
Aim
To identify the effectiveness of DN and LLLT in the management of selected outcome variables among patients with nonspecific LBP.
Materials and Methods
The Quasi experimental study was conducted among a total of 30 subjects who met the inclusion criteria. The subjects were divided into 15 each as group A (DN) and group B (LLLT). The Numerical Pain Distress Scale (NPDS), Quebec Back Pain Disability Scale (QBPDS) and lumbar flexion range of motion were assessed, before and after two weeks of intervention program to identify the effectiveness. Data analysis was done through SPSS and graph pad, using paired t-test and independent t-test.
Results
Both groups have shown improvement after two weeks of intervention treatment program. Both groups showed significant difference in relieving pain, reducing disability and improving lumbar range of motion on nonspecific LBP individually. However, there was no significant difference found between the groups, thus null hypothesis was accepted and rejecting the alternate hypothesis.
Conclusion
Both the techniques are equally effective in reducing the pain, disability level and improving range of motion individually after two weeks of intervention.
Numerical pain distress scale, Quebec back pain disability scale, Range of motion
Introduction
The Lower Back Pain (LBP) accounts for most of the common musculoskeletal pain conditions treated. In over all, about 40% of people have LBP at some point in their lives. The difficulty most often begins between 20 and 40 years of age [1]. A study had reported that approximately 12-80% of younger population, mainly student’s experience LBP. Functional disability associated with LBP might not be the main concern in a younger population. However, experiencing it earlier in life may lead to recurrent and chronic LBP in adulthood [2].
Dry Needle (DN) is one of the common procedures, which is used to treat LBP in current trends. DN is a part of modern Western medicine principles, and supported by research [3]. DN can be used to treat for a variety of musculoskeletal problems [4]. Muscles are thought to be a primary contributing factor to the symptoms. DN can be used as part of complex treatment for chronic musculoskeletal pain and can be applied by family physicians, rheumatologists, orthopedic surgeons, physiatrists, pain specialists, dentists, and physical therapists [5]. DN is the first step in breaking the pain cycle, as research shows it will decrease muscle contraction, reduce chemical irritation, improve flexibility and decrease pain. Needle penetration will cause micro-trauma and micro bleeding localised inflammation [6]. The founder of DN Academy, states DN as methods which can help in providing the healthcare professionals a great tool to serve their patients with great result in conjunction to other therapeutic modalities [7].
Laser is one of the other advantageous techniques which are used to treat LBP by focusing on the trigger points. LLLT therapy uses red-beam or near-infrared laser with wavelength of 600-1000 nanometer (nm) and intensity of 5-500 mw to improve pain degree, joint stiffness and disability. Cold lasers are handheld devices used by the clinician and are often the size of a flashlight. The laser is placed directly over the injured area for 30 seconds to several minutes, depending on the size of the area being treated and the dose provided by the cold laser unit. During this time, the nonthermal photons of light that are emitted from the laser pass through the skin layers (the dermis, epidermis, and the subcutaneous tissue or tissue fat under the skin). This light has the ability to penetrate 2 to 5 centimeters below the skin at 90 mw and 830 nm. Despite a lack of consensus over its scientific validity, specific test and protocols for LLLT suggests that it may be mildly effective, but in most cases no better than placebo, in relieving short-term pain for arthritis, osteoarthritis, acute and chronic neck pain, tendinopathy, and possibly chronic joint disorders [8].
The NPDS (Visual analog scale) for pain and the QBPDS are validated methods for monitoring pain symptom/disability changes in LBP [9,10]. Since, the investigation’s outcomes in LLLT and DN viability in LBP significant varies [11]. Hence, the present study was conducted with an aim to perceive the effectiveness of DN and LLLT on nonspecific low-back desolation patients and moreover to recognise which of the treatment is more fruitful in treating the unclear LBP patients with in shorter period to clear the symptoms.
Materials and Methods
A Quasi experimental study was conducted at Coimbatore (Lakshmi, and Ideal physiotherapy center) and the Singhania University Hospital and Research Centre (Department of physiotherapy), Pacheri Bari, Rajasthan. The duration of the study was from August 2017 to January 2018. The G power analysis tool was utilised to choose the sample size with the reference of previous study [12].
Inclusion criteria: Patients aged between 20 to 40 years, LBP lasting for more than thirty days or longer, nonradiating pain patients, nonspecific mechanical back pain.
Exclusion criteria: The patients with trauma or surgery over lumbar region, received intra-articular corticosteroid during the last 6 months, pregnant or lactating mothers, ongoing co-intervention program, severe cardiovascular, hepatic, renal, or haemopoietic diseases, neurological deficits (sensory or motor), heart pacemaker, type I or decompensated diabetes, uncontrolled systemic arterial hypertension, infectious back pain and inflammatory back pain. Outcome measures were pain intensity in numeric pain distress scale [9], functional disability measured in QBPDS [10], lumbar flexion range of motion by using Schober’s test [13]. Measurement tools of this study were numeric pain distress scale (Visual Analog Scale, 0-10), QBPDS 0-100 points, inch tape, marker pen and hydraulic couch.
After attaining the university research Ethics committee approval, (SU/SOR/2017/103389) a total of 36 subjects with the age of 20 to 40-year-old patients of nonspecific LBP were selected. Due to exclusion criteria, four subjects were excluded. Remaining 32 patients who met the inclusion criteria were selected and equally divided for each group. During the period of study, two subjects were not able to commit for their treatment due to personal reasons, so they withdrew from the study. Only 30 subjects participated throughout the period of study. Those who are taking DN treatment as assigned as Group A and LLLT treatment was assigned as Group B. NPDS [14] and QBPDS questionnaire was issued to fill up by the subjects and also lumbar flexion range of motion were assessed as per the procedure by therapist. Each subject was treated with 2 weeks of period and observed. Intervention duration were 30 to 45 minutes/day, 3 sessions/week. All the subjects of group A and group B, after 2 weeks of intervention program, the post test assessment of NPDS, QBPDS, lumbar flexion range of motion were analysed [Table/Fig-1,2] [15,16].
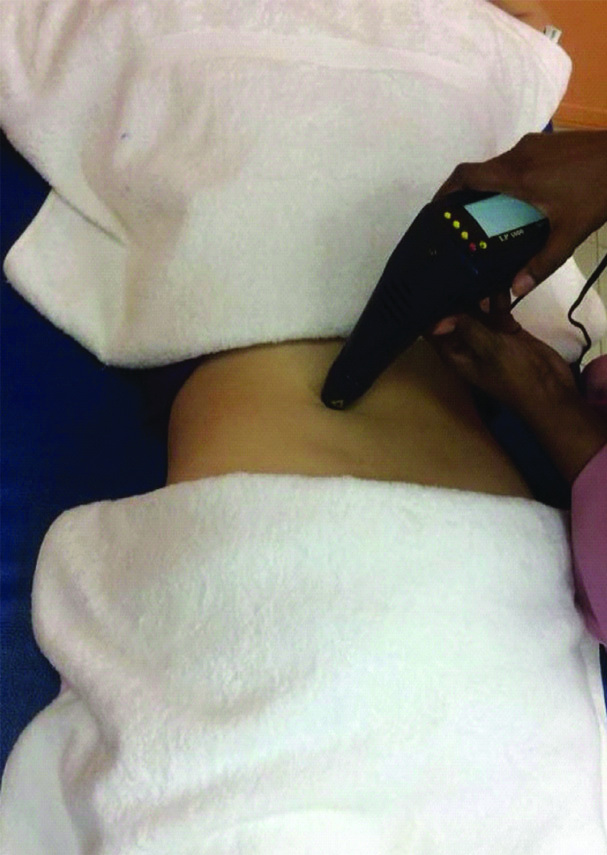
Application of Low Level Laser Therapy (LLLT).
Application of Dry Needling (DN).

Statistical Analysis
The data analysis was done by using descriptive statistics and inferential statistics. In descriptive statistics, mean±standard deviation is used and in inferential statistics, a pair t-test is used to find out difference within the group and independent t-test is used to find out the difference between the groups. p value less than 0.05 was considered as significant.
Results
Both groups shows extremely significant difference on pre-test and post-test evaluation [Table/Fig-3,4]. However, when it compares the post-test results, the two tailed values are 0.055 which was insignificant between the two groups [Table/Fig-5].
Pre-test Post-test score-NumericPain Distress Scale (NPDS)-Group A Dry Needling (DN).
| Group A | Mean | N | Std. deviation | Std. Error mean | Correlation | Sig. |
|---|
| DN pre-NPDS | 7.53 | 15 | 1.24 | 0.32 | 0.58 | 0.02 |
| DN post-NPDS | 3.53 | 15 | 2.03 | 0.52 |
Pre-test Post-test score-Numeric Pain Distress Scale (NPDS)-Group B (Laser).
| Group B | Mean | N | Std. Deviation | Std. Error mean | Correlation | Sig. |
|---|
| Laser pre-NPDS | 7.40 | 15 | 1.45 | 0.37 | 0.51 | 0.04 |
| Laser post-NPDS | 4.86 | 15 | 1.59 | 0.41 |
Post-test Values for Dry Needling (DN) Vs. LLLT–NPDS.
| Dry needling vs Laser | N | Mean | Std. Deviation | Std. Error mean | Sig. (2-tailed) |
|---|
| DN | 15 | 3.53 | 2.03 | 0.52 | 0.055 |
| Laser | 15 | 4.86 | 1.59 | 041 |
Both the groups shows extremely significant difference on pre-test and post-test evaluation [Table/Fig-6,7] as p-values were 0.006 and 0.01 which were significant. However, when it compares the post-test results, the two tailed values are 0.047 which was significant between the two groups [Table/Fig-8].
Pre-test post-test score- Quebec Back Pain Disability scale (QBPDS)-Group A.
| Group A | Mean | N | Std. Deviation | Std. Error mean | Correlation | Sig. |
|---|
| DN pre-QBPDS | 77.26 | 15 | 15.19 | 3.92 | 0.67 | 0.006 |
| DN post-QBPDS | 40.73 | 15 | 16.67 | 4.30 |
Pre-test post-Test score- Quebec Back Pain Disability scale (QBPDS)-Group B.
| Group B | Mean | N | Std. Deviation | Std. Error mean | Correlation | Sig. |
|---|
| Laser pre QBPDS | 78.86 | 15 | 13.34 | 3.44 | 0.64 | 0.010 |
| Laser post QBPDS | 51.80 | 15 | 12.09 | 3.12 |
Post-test values for DN vs. LLLT-Quebac back pain disability scale.
| DN vs Laser-Qbpds | N | Mean | Std. Deviation | Std. Error mean | Sig. (2-tailed) |
|---|
| DN | 15 | 40.73 | 16.67 | 4.30 | 0.047 |
| LASER | 15 | 51.80 | 12.09 | 3.12 |
Both the groups shows extremely significant difference on pre-test and post-test evaluation, with the two tailed p-value as 0.0001 [Table/Fig-9,10]. However, when it compares the post-test results between the two groups, the two tailed values were 0.276 which was insignificant between the two groups [Table/Fig-11].
Pre-test Post-test score Lumbar flexion Rom-Group A (Dry needling).
| Group A | Mean | N | Std. Deviation | Std. Error mean | Correlation | Sig. |
|---|
| DN pre Lumbar flexion ROM | 3.98 | 15 | 0.46 | 0.11 | 0.86 | 0.0001 |
| DN post Lumbar flexion ROM | 4.49 | 15 | 0.33 | 0.08 |
Pre-test Post-test score Lumbar flexion Rom-Group B (LLLT).
| Group B | Mean | N | Std. Deviation | Std. Error mean | Correlation | Sig. |
|---|
| Laser preLumbar flexion ROM | 4.30 | 15 | 0.59 | 0.15 | 0.97 | 0.0001 |
| Laser postLumbar flexion ROM | 4.66 | 15 | 0.50 | 0.12 |
Post-test values for DN vs. LLLT in Lumbar Flexion Rom.
| Dry need vs Laser-lumbar flexion rom | N | Mean | Std. Deviation | Std. Error Mean | Sig. (2-tailed) |
|---|
| DN | 15 | 4.49 | 0.33 | 0.08 | 0.276 |
| LLLT | 15 | 4.66 | 0.50 | 0.12 |
Discussion
Comparison of Laser, DN and Placebo Laser Treatments in Myofascial Pain Syndrome study noted a noteworthy decrease in pain at rest, at activity and increase in pain threshold as compared to other group. The study concluded that Laser therapy could be useful as a treatment modality in myofascial pain syndrome because of its non-invasiveness, ease, and short-term application [17]. In present study, DN is an invasive procedure whereas, laser is a non-invasive procedure, doesn’t show much difference, but both are applied in a short term application. In that short term application DN group shown slightly better than LLLT group B, but it was not significant.
An experimental study about “Early Effects of DN and LLLT in Chronic Tennis Elbow”, the study results for PRTEE score in DN and LLLT shown reduction in pain and disability of elbow. Both DN and LLLT patients were considered to be equally effective in chronic tennis elbow. However, after the first week of intervention, DN group was subjectively reported quick reduction tenderness over extensor origin [12]. In present study, short term application was there and DN group A shown slightly better than LLLT group B, but it was not significant. Additionally, 11 out of 15 patients who were treated with DN have encountered relief of pain after three sessions of period.
Limitation(s)
Less sample size, wide range of age group, specific region, specific ROM and short tern intervention period were the limitations of the study.
Conclusion(s)
Both DN and LLLT are similarly powerful in diminishing pain, disability level and improve function in patients with nonspecific LBP, after the two weeks of treatment program. However, comparatively both therapies don’t show much significant difference on relieving pain, reducing disability and improving range of motion for a nonspecific LBP patient. Studies with large sample size, with more specific groups, with specific duration of pain intensity is recommended for future studies.
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: May 04, 2020
Manual Googling: Sep 26, 2020
iThenticate Software: Oct 27, 2020 (6%)
[1]. Casazza BA, Diagnosis and treatment of acute low back painAmerican Family Physician 2012 85(4):343-50. [Google Scholar]
[2]. Nordin NAM, Kaur D, Kanglun ASL, Low back pain and associated risk factors among health science undergraduatesSains Malaysiana 2014 43(3):423-28. [Google Scholar]
[3]. Simons DG, Travell JG, Simons LS, Myofascial pain and dysfunction: The trigger point manual 1999 Volume 12nd edBaltimore, MDWilliams and Wilkins [Google Scholar]
[4]. Tough EA, White AR, Cummings TM, Richards SH, Campbell JL, Acupuncture and dry needling in the management of myofascial trigger point painEuropean Journal of Pain 2019 13(1):03-10.10.1016/j.ejpain.2008.02.00618395479 [Google Scholar] [CrossRef] [PubMed]
[5]. Kalichman L, Vulfsons S, Dry needling in the management musculoskeletal painJ Am Board Family Medicine201023(5):640-46.10.3122/jabfm.2010.05.09029620823359 [Google Scholar] [CrossRef] [PubMed]
[6]. Gunn CC, Milbrandt WE, Little AS, Mason KE, Dry needling of muscle motor points for chronic low-back pain. Clinical trial with long-term follow-upSpine (Phila Pa 1976) 1980 5:279-91.10.1097/00007632-198005000-000116446774 [Google Scholar] [CrossRef] [PubMed]
[7]. Jain P, Manual of dry needling techniques. INDIA: PREF Publications 2015 :2 [Google Scholar]
[8]. Huang ZY, Ma J, Shen B, Pei FX, Kraus VB, The effectiveness of low-level laser therapy for nonspecific chronic low back pain: A systematic review and meta-analysisArthritis Research & Therapy 2015 (17):36010.1186/s13075-015-0882-026667480 [Google Scholar] [CrossRef] [PubMed]
[9]. Kopec JA, Esdaile JM, Abrahamowicz M, Abenhaim L, Wood-Dauphinee S, Lamping DL, The Quebec Back Pain Disability ScaleSpine 1995 20(3):341-52.10.1097/00007632-199502000-000167732471 [Google Scholar] [CrossRef] [PubMed]
[10]. Davidson M, Keating JL, A comparison of five low back disability questionnaires. Reliability and ResponsivenessPhysical Therapy 2002 82(1):8-24.10.1093/ptj/82.1.811784274 [Google Scholar] [CrossRef] [PubMed]
[11]. Chow R, Johnson M, Lopes-Martins R, Bjordal J, Efficacy of low-level laser therapy in the management of neck pain: A systematic review and meta-analysis of randomized. placebo or active-treatment controlled trialsLancet 2009 374(9705):1897-908.10.1016/S0140-6736(09)61522-1 [Google Scholar] [CrossRef]
[12]. Sukumar S, Mathias L, Rai S, Early effects of dry needling and low level laser therapy in chronic tennis elbowInternational Journal of Health Sciences & Research 2015 5(1):187-96. [Google Scholar]
[13]. Nabavi N, Mohseni-Bandpei MA, MozallaNezhad Z, Rahgozar M, Reliability of measuring lumbar range of motion using modified-modified schober’s test in health subjectsArchives of Rehabilitation 2011 12(3):16-s23. [Google Scholar]
[14]. Boonstra AM, Schiphorst Preuper HR, Reneman MF, Posthumus JB, Stewart RE, Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal painInternational Journal of Rehabilitation Res 2008 31(2):165-69.10.1097/MRR.0b013e3282fc0f9318467932 [Google Scholar] [CrossRef] [PubMed]
[15]. Description of Dry Needling in Clinical Practice. American Physical Therapy Association. Published 2013. http://www.apta.org/StateIssues/DryNeedling/ [Google Scholar]
[16]. Physical Therapists & amp. the Performance of Dry Needling. American Physical Therapy Association. Published January 2012. Accessed February 9, 2015. http://www.apta.org/StateIssues/DryNeedling/ [Google Scholar]
[17]. Ilbuldu E, Cakmak A, Disci R, Aydin R, Comparison of laser, dry needling, and placebo laser treatments in myofascial pain syndromePhotomed Laser Surg 2004 22(4):306-11.10.1089/pho.2004.22.30615345173 [Google Scholar] [CrossRef] [PubMed]