Gout is a relatively common condition in the population today. With progressing of the treatment of the hyperuricaemia, the case of producing a tophus decreases year by year. On the other hand, people who are leaved without treatment is increasing, and severe cases are also seen. Intra-articular tophus is rare, but some cases have been reported in the knee. In this, a case of 33-year-old man who had an intra-articular mass of the knee by gout tophus, causing the limitation of the range of motion is reported. The patient didn’t improve with conservative treatment, so he had to undergo surgery. After arthroscopic excision of the tumour, the patient was symptom free. There had been no recurrence of symptoms at the two-year follow-up.
Arthroscopy, Gouty tophi, Intra-articular tumour knee
Case Report
A 33-year-old male presented with right knee pain and difficulty in walking, since 5 months. The patient was on medication for the same but the pain gradually worsened and range of motion became worse, making him difficult to climb the stairs. The patient was diagnosed hyperuricaemia five years ago, but treatment was not continued due to no symptom. There was no history of previous trauma and gouty attack.
Physical examination revealed marked swelling of the entire right knee, but there was no rise in temperature and no tenderness. The range of motion was remarkably limited to 40 to 80 degrees. Aspiration of the knee joint released 150 mL of turbid yellow fluid with a lot of white debris. The patient had no palpable gouty tophi within the knee and there was no evidence of gouty tophi present anywhere in his body. The synovial fluid test detected numerous urate crystals but no bacteria. Blood tests revealed a uric acid level of 11.0 mg/dL (normal, 3.6-7.0 mg/dL) and a C-reactive protein level of 14.49 mg/dL (normal, <0.3 mg/dL).
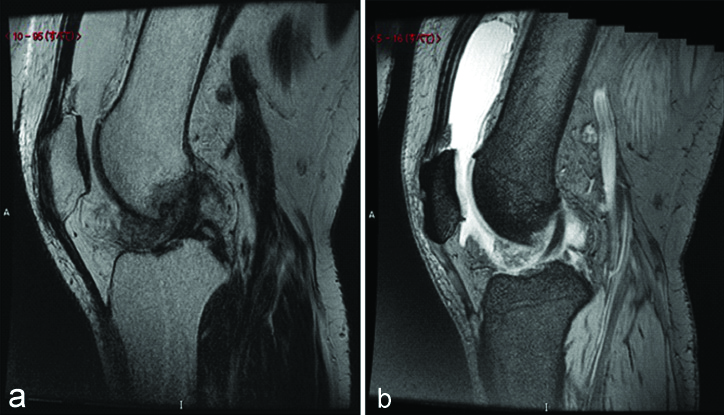
Plain radiographs did not show any abnormalities or calcifications. Magnetic Resonance Imaging (MRI) showed a vague oval-shaped mass of low to intermediate heterogeneous signal intensity on proton density images and intermediate to high on T2* weighted images in front of anterior cruciate ligament. The mass was 20×15×40 mm in size [Table/Fig-1]. With the tentative diagnosis of an intra-articular synovial tumour related to gout, arthroscopy was performed.
MRI showed a vague oval-shaped mass of low to intermediate heterogeneous signal intensity on proton density images (a) and intermediate to high on T2* weighted images (b) in front of anterior cruciate ligament.
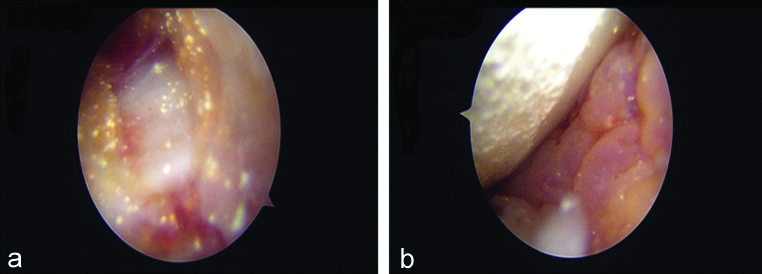
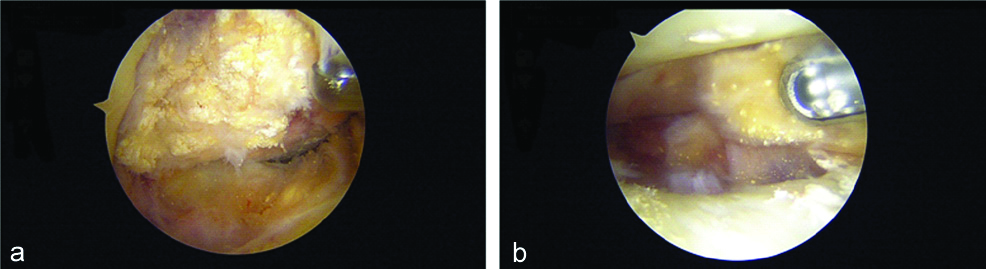
Arthroscopy revealed wide synovitis and a mass of white chalky urate crystals on the surface of the anterior cruciate ligament. No meniscal and ligamentous pathology could be seen, but the urate crystals were deposited throughout the joint on the surface of synovium, meniscus and articular cartilage [Table/Fig-2]. Partial defect of articular cartilage is seen in the medial condyle of the tibia. Extensive curettage of the tophi and the thickened synovium were performed carefully [Table/Fig-3]. When shaving the mass lesions, innumerable white granular debris was scattered. In addition to the debridement of the tophi, synovectomy was also performed extensively in the joint.
(a) The urate crystals were deposited throughout the joint on the surface of synovium, (b) meniscus and articular cartilage.
(a) Extensive curettage of the tophi and the thickened synovium were performed carefully. When shaving the mass lesions, (b) innumerable white granular debris was scattered.
The pathological diagnosis was chronic gouty synovitis with a lot of amorphous uric acid deposits surrounded by fibrous tissue and mild inflammatory reactions. After arthroscopic excision of the tophaceous mass, the patient had improved significantly in regard to pain and the range of motion and is able to sit in a lotus position now. The patient has been keeping a regular diet and taking benzbromarone 100 mg twice a day to control uric acid after the operation. There had been no recurrence of symptoms at two-year follow-up.
Discussion
Gout is a relatively common disease in the population today affecting more than 1 million people in Japan. It is caused by hyperuricaemia and the patient of the hyperuricaemia is more than 10 million people in Japan. It is called lifestyle-related disease [1].
Most hyperuricaemia patients are asymptomatic and untreated. So, there are a lot of patients who are not treated. Subcutaneous tophi occur in patients with a long duration of gout and high serum urate [2] and besides, it can be that the presence of intra-articular tophi is related to the long gout duration. Tophi have been found in about 10% of gout patients [3]. Gouty tophi are reported to occur in the auricle 39%, the first toes 17%, and the knee 2-4% [1]. Urate crystals deposited in local tissues coalesce into one another and grow larger, causing necrosis and fibrosis in the tissues. The granulomas thus formed are gouty tophi. In particular, it is often found in areas where the temperature is low, blood flow is poor, and mechanical stimulation is likely to occur [1].
Tophi are usually located in subcutaneous tissue and can be easily diagnosed without imaging evaluation [2]. Tophi deposits are well known to cause joint destruction, gouty nephropathy, concomitant septic infection, spinal cord compression and mechanical restriction to the range of the movement of the knee joint have also been reported [2-10].
Tophi are basically radiolucent and are unable to be visualised with radiographs. Computed Tomography (CT) is said to be the best method for delineating the gouty tophi [11,12]. Although CT examination was not performed this time, it is considered necessary from now on if gouty tophi is suspected. In general, MRI is very effective to get a differential diagnosis of an intra-articular mass. All the intra-articular tophi manifested low to intermediate signal intensity on both T1- and T2- weighted images [4,11,12]. The MRI appearance of gouty tophi is constant on T1-but quite variable on T2- weighted images. This variability in signal intensity could be depended on the content of calcium. So, it may be difficult to make a diagnosis using only the images. They cannot be considered specific to tophi, especially a nonspecific enhancement.
At MRI examination, the case is imaging under proton density weighted image and T2* weighted image to detect intra-articular lesions such as ligaments, meniscus and cartilage. In this case, the intra-articular mass was confirmed, but there were nonspecific findings and no diagnosis could be made.
The differential diagnosis based on MRI appearance also includes chronic rheumatoid arthritis, pigmented villonodular synovitis, chronic infectious arthritis and amyloidosis [5,9]. In synovium, there was a nonspecific swelling histologically and graphically, joint fluid was nonhaemorrhagic, culture test was negative and there was no rise in fever, so these were denied.
In this case, gouty arthritis was strongly suspected because hyperuricaemia and urate crystals in the synovial fluid were observed.
Ultimately, definitive diagnosis depends on surgery or biopsy. In a recent report, 26 patients with restricted range of motion due to gouty nodules in the knee joint gradually improved with conservative treatment [2]. However, in past reports, there are some reports which show that conservative treatment was difficult, but arthroscopic excision improved the symptoms in a short period of time [Table/Fig-4]. So, it was decided to have surgery [3-8].
Comparison of the present case findings against published cases [3-8].
| Authors name | Age/Sex | Chief complaint | Clinical findings | Radiological findings | MRI | Provisional diagnosis | Differentials | Other investigations performed | Final diagnosis | Outcome |
|---|
| Kobayashi K et al., [3] | 34/M | Knee pain swelling | Hydrops ROM: 0-20 muscle atrophy of thigh | Bipartite patella bone cyst-like lesion | Bone cyst-like lesion | Gouty tophi | - | Histologic exam. | Gouty tophi | Arthroscopical excision →improved |
| Li TJ et al., [4] | 53/M | Knee pain swelling | Some effusion ROM: 5-120 tenderness Present | Nothing | Synovial tumour | Synovial neoplasm | PVNS | Histologic exam. | Gouty tophi | Arthroscopical |
| Alejandro EB et al., [5] | 53/M | Knee pain locking | Hydrops unable to full extension | Nothing | No image | Meniscal lesion | - | - | Gouty tophi | Arthroscopical |
| Soumya C and Hakan I [6] | 67/M | Knee pain swelling locking | Unable to fully extend and flex | Mild Osteo arthritis | No image | Meniscal lesion | Torn cruciate ligament loose body | CT; soft tissue calcification | Gouty tophi | No arthroscopy medication →improved |
| Amber H et al., [7] | 29/M | Knee pain swelling locking | Hydrops ROM: 30-100 | Nothing | Nonspecific mass | Synovial sarcoma | PVNS infectious arthritis amyloidosis | Histologic exam. | Gouty tophi | Arthroscopical |
| Raymond GS et al., [8] | 42/M | Knee pain locking catching | Hydrops ROM: 20 degree | Osteophyte mild Osteo arthritis | Tears along the posterior horn of both menisci | Meniscal lesion | Other intra-articular condition | - | Gouty tophi | Arthroscopical excision →improved |
| Present case | 33/M | Knee pain swelling | Hydrops rom: 40-80 | Nothing | Oval-shaped mass | Synovial mass (tumour) | Other intra-articular condition | Histologic exam. | Gouty tophi | Arthroscopical excision →improved |
MRI: Magnetic resonance imaging; PVNS: Pigmented villonodular synovitis; CT: Computed tomography; ROM: Range of motion
The diagnosis of significant intra-articular gouty tophi covering the articular cartilage and menisci was made, intraoperatively. When debriding the tophi from the femur and tibia, we must be more careful of the underlying articular cartilage and avoid iatrogenic damage leading to a poor clinical result [8]. It is very important to curette the tophi as soft as possible, using a small curet and a standard arthroscopic shaver. The basis of treatment for hyperuricaemia is drug therapy [1,2,6,13]. The goal is to keep proper blood uric acid levels to prevent some complications. In cases, where functional disorders such as chronic pain and range of motion do not improve even after conservative treatment, surgical treatment should be considered positively. Arthroscopic excision of the tumour is a minimally invasive and highly effective treatment [3-5,7-9,13-15].
Conclusion(s)
If conservative therapy is not effective to relieve the pain and improve the function in the knee, surgical excision should be considered. Arthroscopic excision of the tumour is very effective and recommended.
MRI: Magnetic resonance imaging; PVNS: Pigmented villonodular synovitis; CT: Computed tomography; ROM: Range of motion
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 18, 2020
Manual Googling: Sep 24, 2020
iThenticate Software: Oct 26, 2020 (20%)
[1]. Nakamura T, Treatment of hyperuricaemia and gout MedReview 2001 [Google Scholar]
[2]. Lu CC, Wei JCC, Chang CA, Chen CM, Tsai SW, Yeh CJ, Limited knee-joint range of motion in patients with tophaceous gout improved with medical treatment: A 18-months follow-upFront Med (Lausannne) 2020 7:710.3389/fmed.2020.0007432181257 [Google Scholar] [CrossRef] [PubMed]
[3]. Kobayashi K, Deie M, Okuhara A, Adachi N, Yasumoto M, Ochi M, Tophaceous gout in the bipartite patella with intra-osseous and intra-articular lesions: A case reportJ Orthop Surg 2005 13(2):199-202.10.1177/23094990050130021916131688 [Google Scholar] [CrossRef] [PubMed]
[4]. Li TJ, Lue KH, Lin ZI, Lu KH, Arthroscopic treatment for gouty tophi mimicking an intra-articular synovial tumour of the kneeArthroscopy 2006 22-8:910.e1-e3.10.1016/j.arthro.2005.06.03116904600 [Google Scholar] [CrossRef] [PubMed]
[5]. Alejandro EB, Stephan MC, Jose MSF, Jose MGH, Joaquina RDP Knee locking due to a single gouty tophusJ Rheumatol 2006 33:193-95. [Google Scholar]
[6]. Soumya C, Hakan I, Painful knee locking caused by gouty tophi successfully treated with allopurinolNat Clin Pract Rheumatol 2008 4:675-79.10.1038/ncprheum094519002128 [Google Scholar] [CrossRef] [PubMed]
[7]. Amber H, Singh VA, Azura M, Gouty tophi mimicking synovial sarcoma of the knee jointArch of Rheumatol 2012 27:208-11.10.5606/tjr.2012.035 [Google Scholar] [CrossRef]
[8]. Raymond GS, Michael M, Douglas R, Arthroscopic management of intra-articular tophaceous gout of the knee: A case report and review of the literatureJ Orthop Case Rep 2018 8(2):86-89. [Google Scholar]
[9]. Yu KH, Lien LC, Ho HH, Limited knee joint range of motion due to invisible gouty tophiRheumatology 2004 43:191-94.10.1093/rheumatology/keg47812949254 [Google Scholar] [CrossRef] [PubMed]
[10]. Wang W, Li Q, Cai L, Liu W, Lumbar spinal stenosis attributable to tophaceous gout: Case report and review of the literatureTher Clin Risk Manag 2017 13:1287-93.10.2147/TCRM.S14590629033576 [Google Scholar] [CrossRef] [PubMed]
[11]. Chen CK, Yeh LR, Pan HB, Yang CF, Lu YC, Wang JS, Intra-articular gouty tophi of the knee: CT and MR imaging in 12 patientsSkeletal Radiol 1999 28(2):75-80.10.1007/s00256005047710197451 [Google Scholar] [CrossRef] [PubMed]
[12]. Yu JS, Chung C, Recht M, Dailiana T, Jurdi R, MR imaging of tophaceous goutAm J Roentgenol 1997 168(2):523-27.10.2214/ajr.168.2.90162409016240 [Google Scholar] [CrossRef] [PubMed]
[13]. Kasper IR, Juriga MD, Giurini JM, Shmerling RH, Treatment of tophaceous gout: When medication is not enoughSemin Arthritis Rheum 2016 45(6):669-74.10.1016/j.semarthrit.2016.01.00526947439 [Google Scholar] [CrossRef] [PubMed]
[14]. Kumar S, Gow P, A survey of indications, results and complications of surgery for tophaceous goutN Z Med J 2002 115(1158):U109 [Google Scholar]
[15]. Lee SS, Lin SD, Lai CS, Lin TM, Chang KP, Yang YL, The soft-tissue shaving procedure for deformity management of chronic tophaceous goutAnn Plast Surg 2003 51(4):372-75.10.1097/01.SAP.0000067723.32532.9714520064 [Google Scholar] [CrossRef] [PubMed]