The AP is a commonly performed it is an invasive procedure done in emergency as well as inpatient settings for detecting patients’ metabolic and ventilatory status. Patients usually experience pain and discomfort during this procedure [1]. The Spanish Society of Pneumology and Thoracic Surgery (SEPAR) suggested the use of local anaesthetic agent like lidocaine before carrying out the AP procedure as this would minimise or avoid pain experienced during the procedure [2]. The probable reasons for infrequent use of local anaesthesia may be because of need to wait for few minutes prior to radial artery puncture, pain caused by infiltration of anaesthetic drug, anatomical distortion, which produces difficulty in locating the arterial pulse and moreover, it had not demonstrated significant effect in reducing pain experienced by participants during the procedure [2-5]. An urgent radial AP would need a local anaesthetic agent with rapid action and easy application. There is a considerable amount of literature showing the use of ethyl chloride spray and ice pack before intravenous cannulation, sport medicine and minor surgery [2]. Both the anaesthetic modalities work on the principle of cryoanalgesia yet there is lack of conclusive evidence regarding their efficacy to reduce pain during radial AP and superiority over traditional methods [4,5].
The present study was done with the aim to evaluate the efficacy of chloride spray versus ice pack application in reduction of pain intensity during radial AP.
Materials and Methods
A randomised controlled parallel group trial was carried out with outcome assessor blinding. Trial was performed among patients admitted in pulmonary high dependency unit of a tertiary care hospital and data were collected during November 2018 to December 2018. The study was conducted as per guidelines of Helsinki declaration for conducting the clinical trials, the standards of good clinical practices and Indian legislation. This trial was approved from Institutional Ethical Committee vide letter no. ECR/736/Inst/UK/2015 dated 05/04/2018 and it was registered in the Clinical Trial Registry of India vide registration no. REF/2018/04/019292. A voluntary informed written consent was obtained from each participant before enrolling into the trails. Participants aged 18 to 60 years, who were admitted in the hospital and prescribed ABG analysis either routine or on emergency basis were included in the study. However, participants who had decreased level of consciousness (Glasgow coma scale score <15), developmental delay, radial artery fistula, negative Allen’s test, history of drug reaction to ethyl chloride and cold stress, under influence of alcohol and undergoing active treatment for pain management were excluded.
No similar study was found, thus sample size was calculated based on pilot study results using sample size calculation software (G power software by http://www.ats.ucla.edu/stat/gpower/pairedsample.htm) [6]. Pilot study results of 20 participants (10 in each arm) revealed that mean pain scores were 2.78±0.16 and 2.90±0.18 among ethyl chloride (experimental arm A) and ice pack (experimental arm B), respectively. With 5% level of significance and 80% power, 26 participants were required in each arm. In this study, 60 participants were included after considering 20% attrition rate. Participants were enrolled in the study using consecutive sampling technique and then they were assessed for confirmation of eligibility criteria, before they were finally recruited in the trial. Recruitment of participants under this trial was terminated at the time when calculated sample size was achieved for both arms. Participants were randomly assigned to experimental arm A and experimental arm B. Randomisation was done using computer generated random list and allocation concealment was performed by sequentially arranged opaque sealed envelopes.
The blood sample was taken from radial artery by the primary investigator only. The patient’s wrist was extended in the supine position and a rolled towel was placed under the wrist to provide position. By using a standardised 23-guage heparinised needle by fixing radial artery with left indexed figure of the performer and puncturing the artery at an angle of 30-45°. A firm pressure was applied for approximately 2-3 minutes to stop the bleeding and pressure time was five minutes or more for patients who were on anticoagulants or had high blood pressure. When more than one puncture was needed; the procedure was carried out again with same protocol. Participants assigned to experimental arm A underwent radial AP as per institutional protocol in addition application of ethyl chloride spray (Ethyl Chloride I.P. 100% w/v manufactured by Jiana Lifesciences, Mumbai) at puncture site for three seconds just before to the procedure. According to the manufacturer’s instructions; a distance 12-18 centimeters was maintained to skin from which it was sprayed. While participants assigned to experimental arm B received ice-pack application for three minutes before radial AP. Another investigator which was blinded to the procedure measured the pain experienced by the participants and development of haematoma because of procedure. In this trial, level of pain intensity was primary outcome variable. Participants were asked to report level of pain intensity during radial AP and measured immediately after procedure using pain numeric rating scale, which quantify level of pain from 0 (indicate no pain) to 10 (indicate the worst pain thinkable). The secondary outcome variable was presence of haematoma, success of first attempt and time taken for puncture. Haematoma was assessed within two hours of procedure by the same blinded assessor.
Statistical Analysis
Data were entered in Excel sheet and transferred to the statistical computer and analysed using a SPSS package, IBM SPSS 23.0. An Intention-To-Treat (ITT) analysis was carried out. As continuous variables were not normally distributed, therefore, comparison between the groups on pain score was done by using Mann-Whitney U test while categorical data were analysed using chi-square test. The incidences of haematoma development were analysed using frequency and percentage, while differences in pain perception between groups were measured using Fisher’s-exact test. We considered p-value<0.05 for statistical significance for all comparisons.
Results
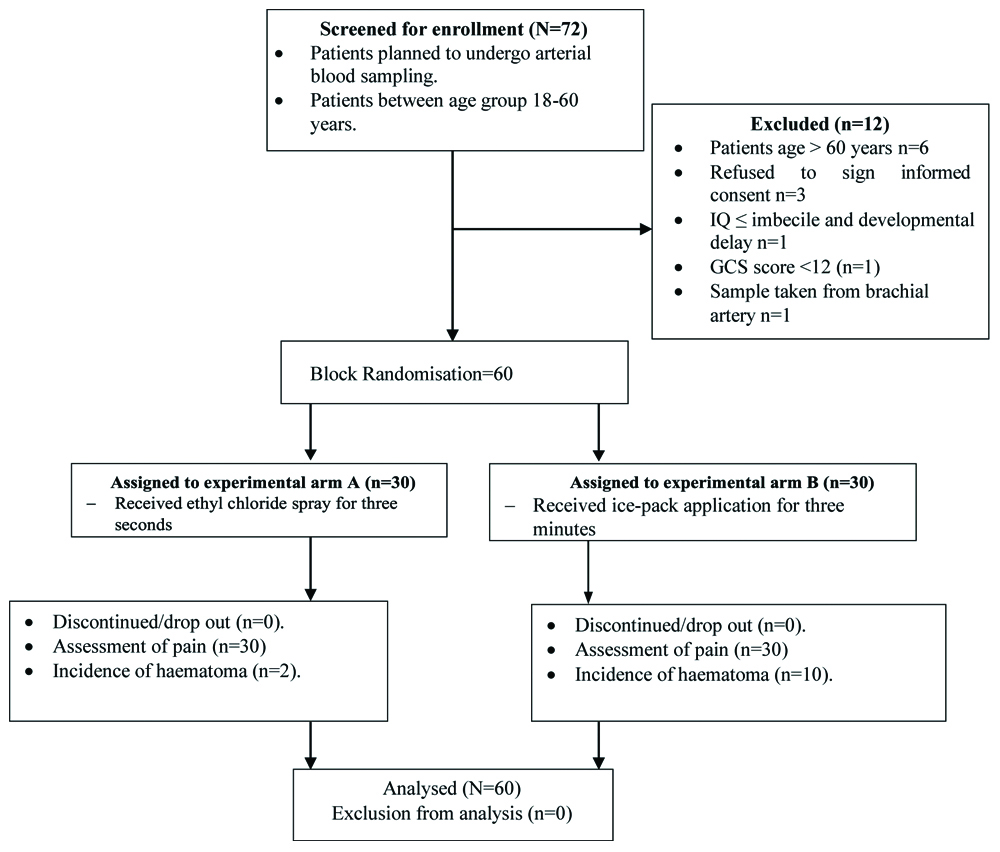
A total of 72 participants were enrolled from aforementioned department during November 2018 and December 2018. Out of 72 participants who were evaluated for recruitment, 12 were excluded because they did not meet inclusion criteria of the study Sixty participants completed the trial, 30 in each group. [Table/Fig-1] presents the CONSORT diagram of participants.
CONSORT diagram of participants.
The mean age±SD of participants in the experimental arm A and experimental arm B were 50±9 and 45±10, respectively. The distribution of participants’ age was significantly different between the groups (p=0.03). On contrary all other demographic variables of participants were well matched and no significant difference was noted between the groups [Table/Fig-2].
Demographic profile of study participants N=60.
| Characteristics | Ethyl spray experimental arm A (n=30) (%) | Ice pack experimental arm B (n=30) (%) | Total (N=60) | p-value |
|---|
| Age (mean±SD) | 50±09 | 45±10 | 47±10 | 0.03* |
| Gender |
| Male | 24 (40) | 25 (42) | 49 (82) | 0.74 |
| Female | 06 (10) | 05 (08) | 11 (18) |
| Education status |
| Higher secondary | 12 (20) | 18 (30) | 30 (50) | 0.29 |
| Graduate | 02 (03) | 01 (02) | 03 (05) |
| Uneducated | 16 (27) | 11 (18) | 27 (45) |
| Habitat |
| Urban | 04 (07) | 09 (15) | 13 (22) | 0.12 |
| Rural | 26 (43) | 21 (35) | 47 (78) |
| Type of admission |
| Emergency | 21 (35) | 18 (30) | 39 (65) | 0.42 |
| Routine | 09 (15) | 12 (20) | 21 (35) |
| Co-morbidity |
| Yes | 13 (22) | 17 (28) | 30 (50) | 0.30 |
| No | 17 (28) | 13 (22) | 30 (50) |
| Analgesic consumption |
| Yes | 02 (03) | 02 (03) | 04 (07) | 1.00 |
| No | 28 (47) | 28 (47) | 56 (93) |
| The incidence of any other pain |
| No | 25 (42) | 22 (37) | 47 (78) | 0.34 |
| Yes | 05 (08) | 08 (13) | 13 (22) |
| Experience of radial artery puncture |
| Yes | 21 (35) | 21 (35) | 42 (70) | 1.00 |
| No | 09 (15) | 09 (15) | 18 (30) |
| Use of anticoagulant therapy |
| Yes | 04 (07) | 03 (05) | 07 (12) | 0.68 |
| No | 26 (43) | 27 (45) | 53 (88) |
| History of drug allergy |
| No | 27 (45) | 23 (38) | 50 (83) | 0.16 |
| Yes | 03 (05) | 07 (12) | 10 (17) |
*p-value <0.05 is statistically significant; n: Number of participants; %: Percentage; SD: Standard deviation
Chi-square test applied
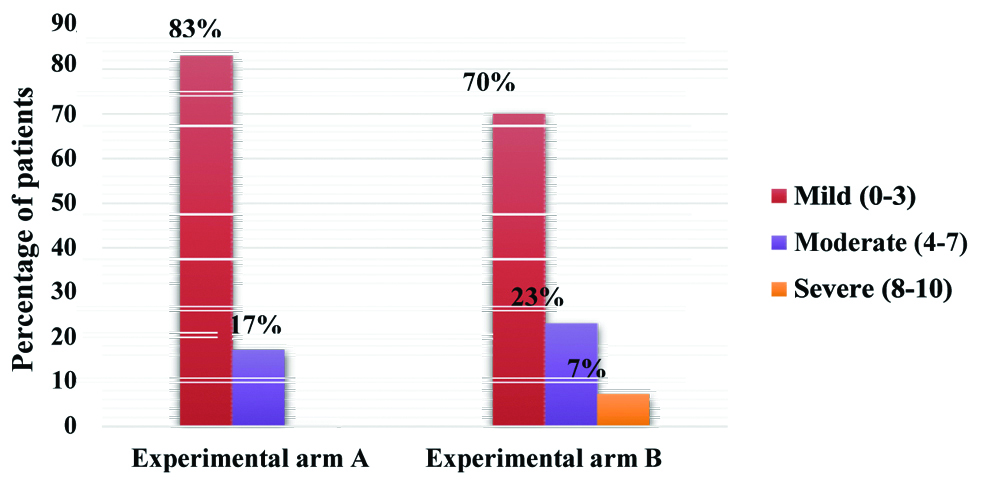
[Table/Fig-3] shows the mean pain score experienced by participants during radial AP were 2.5±1.2 in experimental arm A and 3.1±1.8 in experimental arm B. Differences on pain scores were analysed by Mann-Whitney U test; analysis revealed no significant difference between the groups. Scores of pain during radial AP were categorised into mild, moderate and severe and analysed by frequency and percentage [Table/Fig-4]. Mild pain was reported by 83% and 70% of participants in experimental arm A and experimental arm B, respectively. However, no participants in experimental arm A and 7% participants in experimental arm B reported severe pain during procedure.
Comparison of pain scores of study participants between the groups (N=60).
| Study groups | Mean±SD | Confidence interval (95%) | Z-value | p-value |
|---|
| Experimental arm A | 2.5±1.2 | 2.4-3.2 | -1.58 | 0.113 |
| Experimental arm B | 3.1±1.8 |
p-value <0.05 is statistically significant
Mann-Whitney U test applied
Pain severity distribution by pain numeric rating scale scores.
Differences on incidences of haematoma development within two hours of procedure were analysed by the Fisher’s-exact test; analysis revealed incidence of haematoma was significantly high in experimental arm B as compared to experimental arm A (33.33 vs. 6.66%; p=0.010). While success at first attempt and time taken for puncture were not significant differ between the groups [Table/Fig-5].
Incidence of haematoma, number of attempt and extraction time N=60.
| Experimental arm A (n=30) (%) | Experimental arm B (n=30) (%) | p-value |
|---|
| Haematoma (within 2h) | | | |
| Present | 02 (6.66) | 10 (33.33) | 0.010* |
| Absent | 28 (93.33) | 20 (66.67) | |
| Success at first attempt | 26 (86.67) | 27 (90) | 0.68 |
| Time taken for puncture | | | |
| ≤35 seconds | 20 (66.67) | 18 (60) | 0.41 |
| >35 seconds | 10 (33.33) | 12 (40) | |
*p-value <0.05 is statistically significant; %: Percentage
Fisher’s-exact test applied
Discussion
Radial AP is common procedure in emergency and intensive care units for ABG analysis. Unfortunately, this procedure is very painful and causes anxiety and emotional distress for patients [7]. Application of topical anaesthesia is common practice to alleviate pain during radial AP. Also, cryoanalgesia has been suggested as an alternative option to topical anaesthesia in alleviating pain due to AP [2]. Ethyl chloride and ice generate anaesthetic effect by cooling a specific part of skin but the exact mechanism of their anaesthetic effect is still unclear. However, various mechanisms like reduced nerve conduction velocity, prevention of oedema formation at the site of infiltration, inhibition of pain-producing substances, decrease muscle spasm and expression of endorphins have been proposed. Although, use of cryoanalgesia in reducing pain during radial AP has been less explored and studied in clinical practice [8-10].
The present study demonstrates that application of ethyl chloride and ice pack before radial AP had no significant difference in reducing pain associated with procedure. To the best of authors’ knowledge, there has been only one clinical trial which compared vapocoolant to ice pack and findings of above trial were in consensus to present study, where it concluded that both groups had similar median pain score during intravenous catheter placement [11]. However, that study was conducted among children aged between 9-18 years. On contrary, another study compared the efficacy of vapocoolant and ice in reducing pain during intra-dermal antibiotic skin test [12]. Study reported that 84% participants experienced ice application more effective and only 2% participants’ preferred vapocoolant in pain reduction.
Previous studies have assessed the effect of ice on pain associated with AP [13,14]. Both studies found that ice pack application at puncture site just before to procedure showed significant reduction of pain during AP. These findings are similar with present study trial finding where majority of participants experienced mild pain during procedure. Another study showed contradictory findings, reported no significant difference between experimental group (ice pack application) and control group (no treatment) in pain numeric rating scale scores during intravenous catheter placement [15]. Moreover, 39% of participants experienced that ice application was more painful than routine procedure. These findings reinforced the idea to have a shorter duration (3 minutes) of ice application than 10 minutes in that study.
Recently, four studies that examined the efficacy of ethyl chloride in pain reduction during AP presented contradictory findings. Two studies were in agreement with findings of present study, did not noted significant differences in pain experienced by participants during AP with or without application of ethyl chloride [2,4]. Another study compared vapocoolant to lidocaine in reducing pain associated AP procedure [17]. That study demonstrated vapocoolant was significantly more effective in pain reduction than lidocaine, which shows its practical utility as an alternative solution for a local anaesthesia. While contradictory findings showed by other study in which EMLA found more effective than vapocoolant in pain reduction during intravenous cannulation of arteriovenous fistula [18]. The difference in the results among the two trials could be because of reduced time of application i.e., two seconds; whereas, in present trial it was three seconds. Another possible explanation to discrepancies in the results could be small sample size (n=41) included in that study whereas present trial included 60 patients [19].
The incidences of haematoma formation in both the experimental arms were assessed. There is no literature available that has compared the haematoma incidence after using both the interventions and these findings are unique to this trial. However, further research is needed to get insight into this phenomenon. One of the previous study had conflicting findings with no significant difference in the incidence of haematoma formation upon moist application of ice on subcutenous heparin site [20]. With regard to success of first attempt and time taken for puncture present findings were in loop with the trial which reported no significant difference between the groups [2,13].
Limitation(s)
This was a single centre study and sample size was small. In addition, both interventions were different and therefore, participants and the primary investigator were not blinded. Furthermore, there was no standard control group in this trial.
Conclusion(s)
Ethyl chloride spray and ice pack application have no significance difference in reducing pain intensity due to radial AP. However, ethyl chloride spray was significantly more effective in prevention of early haematoma formation at radial AP site. Therefore, ethyl chloride spray is recommended to be used at radial artery planned puncture site for three seconds just before to the procedure.
*p-value <0.05 is statistically significant; n: Number of participants; %: Percentage; SD: Standard deviation
Chi-square test applied
p-value <0.05 is statistically significant
Mann-Whitney U test applied
*p-value <0.05 is statistically significant; %: Percentage
Fisher’s-exact test applied