Long-Term Stability of Root Coverage of Restored Roots: A 18-Year Follow-up Case Report
Khalid S Al-Hamdan1
1 Associate Professor, Department of Periodontics and Community Dentistry, College of Dentistry, King Saud University, Riyadh, Saudi Arabia.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Khalid S Al-Hamdan, 7669 King Saud University Unite-1, Riyadh, Saudi Arabia.
E-mail: khalidh1@ksu.edu.sa
Tooth sensitivity is a major concern following gingival recession. Stable long-term results are necessary for the management of this condition. Here, we present a case report with the aim of validating the utilisation of a connective tissue graft to replace a restorative material over the root surface for a long term. A 36-year-old female patient presented with the chief complaint of sensitivity in her lower right (#43) and left (#33) canines, which were previously restored with a composite restoration. The recession type defect was Miller’s Class II. The old restoration was removed and replaced with a connective tissue graft, accompanied by a double-papilla flap. The case was followed-up for 18 years, and the results were stable during the follow-up period, with a highly satisfied patient. Based on these results, it can be reported that a connective tissue graft has highly predictable results and can be used for previously restored root surfaces. In addition, the connective tissue graft provides more stable results than does the use of a restorative material over root surfaces.
Connective tissue graft, Gingival recession, Root coverage, Root restoration
Case Report
A 36-year-old female patient presented in to the periodontal clinic in 2002 with a complaint of long teeth and sensitivity in the lower right (#43) and left (#33) canines. The dental history revealed that the patient had a history of using an aggressive brushing technique, which caused generalised abrasion of the cervical region and resulted in the placement of a composite restoration to fill the abrasion area. Subsequently, gingival recession occurred in some areas, and root sensitivity reoccurred because of a leakage of these restorations. Clinical examination revealed the presence of gingival recessions of approximately 3-4 mm on teeth #33 and #43, with the presence of a composite restoration on the root surface [Table/Fig-1]. The recession defect was classified as Miller’s Class II, with 1 mm of a keratinised gingiva and no attached gingiva [1]. The probing depth ranged from 1 to 2 mm. The plaque index was 75%, with bleeding on probing of 55%. Phase I therapy consisted of scaling and root planing, with plaque control measures using a modified Stillman’s brushing technique and interdental flossing at home. The surgical phase consisted of removal of the old restoration and replaced with a new restoration which; was contoured to the crown only then, placement of a connective tissue graft, combined with a double-papilla flap. The patient agreed to the procedure and signed informed consent. Prior to soft tissue grafting, the composite restoration was removed from the root surface and contoured to the tooth crown only, and the root surface was smoothed with a finishing bur [Table/Fig-2]. The right side of the palate was used as a donor site, which was anaesthetised with one ampoule of lidocaine, while each recipient site received two ampoules. Blade #15 was used for incision placement and palatal tissue harvesting. Two oblique incisions of 3 mm long were placed on each side of the tooth, with two vertical incisions extended beyond the mucogingival junction. A partial thickness flap was utilised all the way long [Table/Fig-3]. A connective tissue graft of 13×5 mm, with 2-mm thickness after removal of adipose tissue, was harvested from the palate, and the donor site was secured with a 4-0 vicryl suture [Table/Fig-4]. The graft was divided in half, for teeth #33 and #43, respectively. The graft was then, sutured in place with a 5-0 vicryl suture using a simple interrupted technique; then, a double-papilla rotational flap was secured with 5-0 vicryl [Table/Fig-5]. No periodontal dressing was used. Postsurgical medication consisted of ibuprofen 400 mg/qid for four to seven days and rinsing with normal saline twice daily for seven days. The patient was instructed to eat soft food for seven days. Brushing of the surgical site was deferred for six weeks, and the patient was asked to use a cotton tip with mouthwash to clean the area twice daily. The sutures were removed after two weeks, and the healing was uneventful, with no complications [Table/Fig-6]. Since the patient had mild localised periodontitis, with a history of an aggressive brushing technique, she was placed on a maintenance recall every four months for suppurative periodontal therapy.
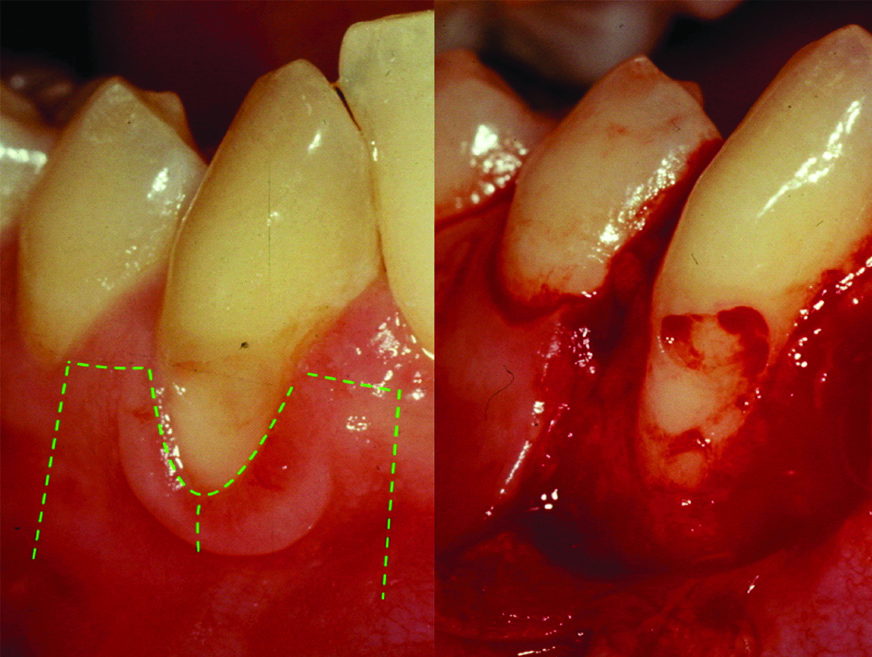
Pre-operative images for teeth #43 and #33 in 2002.

Image after composite removal from teeth #43 and #33 and root surface smoothening.

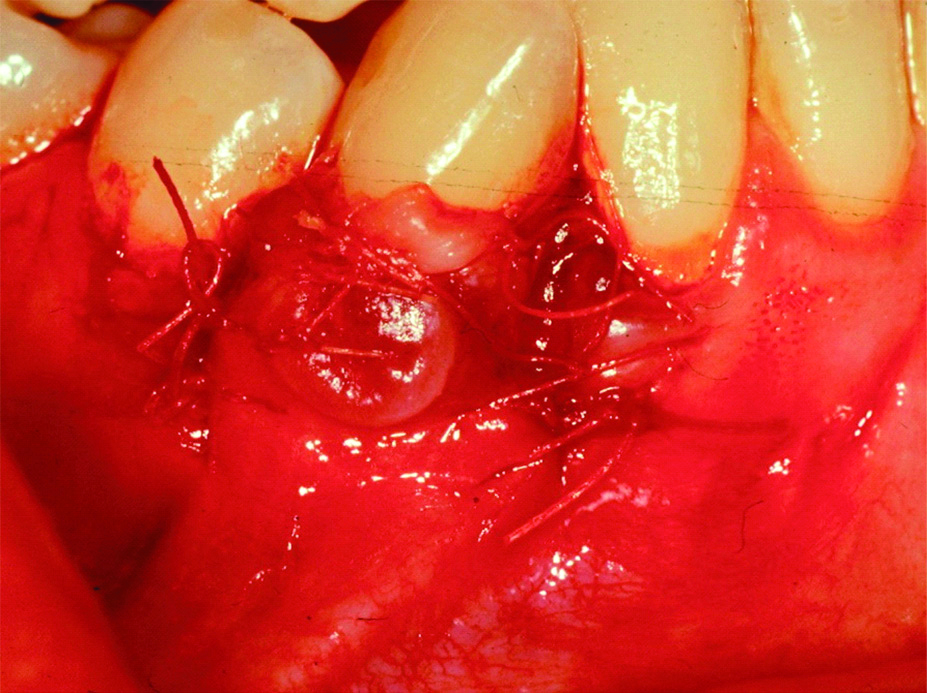
Flap design for a double-papilla flap.
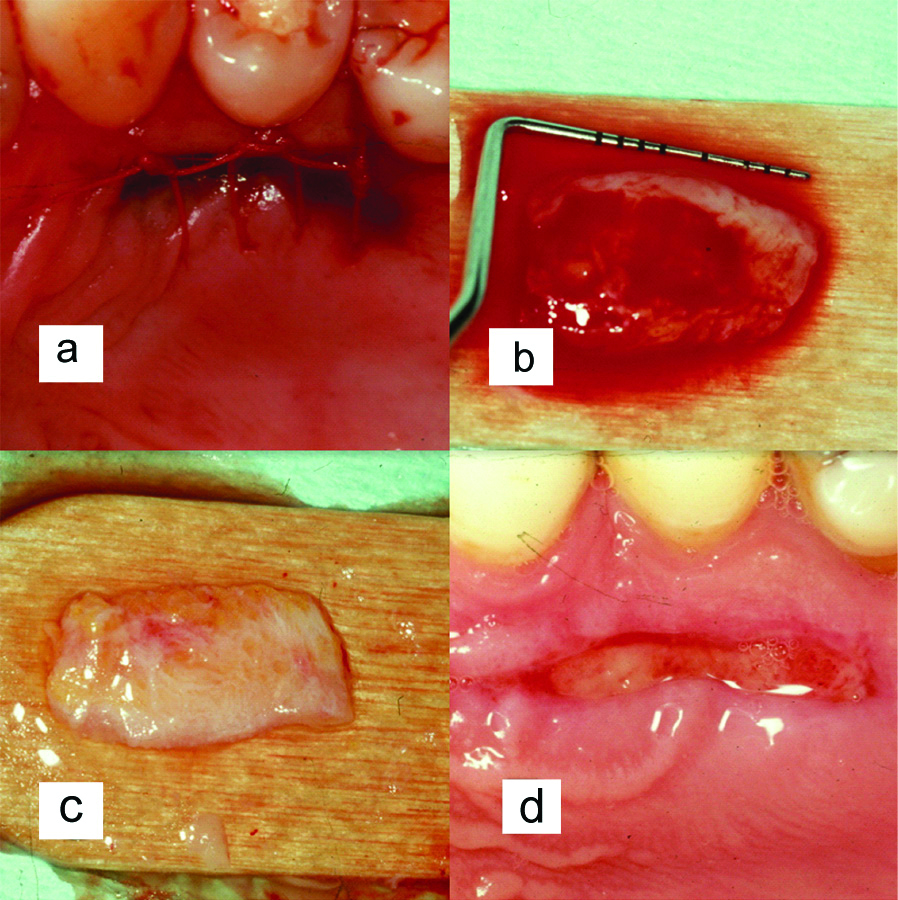
a) Palatal donor site; b) Approximately 13 mm of tissue harvested; c) Palatal tissue after removal of adipose tissue; d) Donor site after two weeks of healing.
Flap suturing for tooth #43.
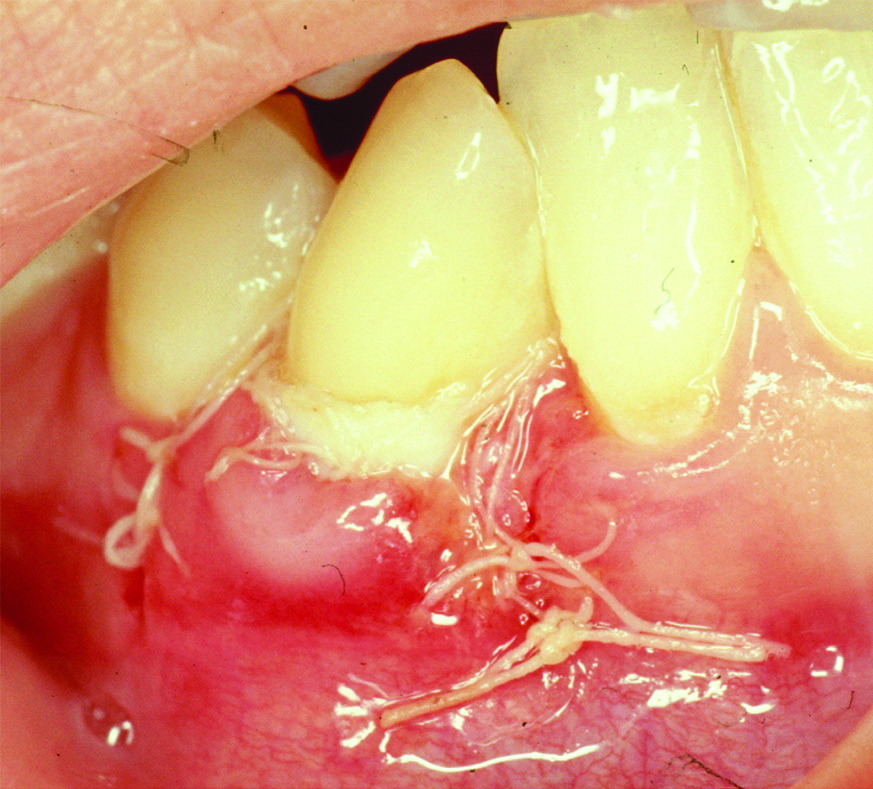
Slight sloughing of the coronal part of the graft on tooth #43 after two weeks of healing.
During the follow-up period, which lasted for 18 years, no adverse significant changes were noted over time. Instead, the root coverage and keratinised tissue increased over time [Table/Fig-7,8,9,10,11 and 12].
Follow-up images of teeth #33 and #43 in 2006.

Follow-up images of teeth #33 and #43 in 2010.

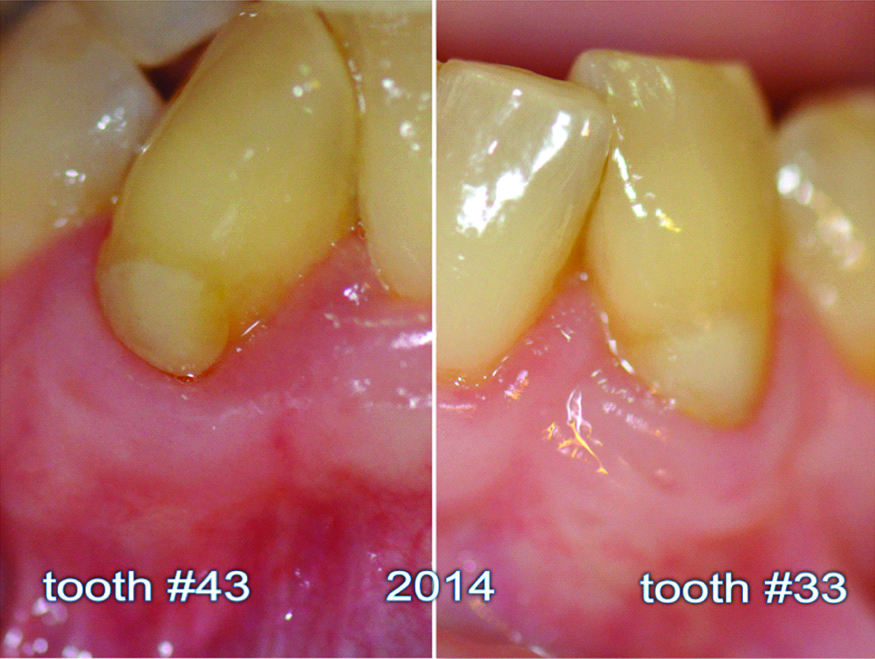
Follow-up images of teeth #33 and #43 in 2014.
Eighteen-year follow-up image of tooth #33.

Eighteen -year follow-up image of tooth #43.

Eighteen -year follow-up images of teeth #33 and #43.

The clinical results showed a 100% complete root coverage with a gain of keratinised tissue of 3-4 mm and a probing depth of 1-2 mm [Table/Fig-13].
Recession and keratinised tissue measurements.
| Recession/Keratinised tissue (mm) | Tooth #33 Recession/Keratiniz Keratinised tissue (mm) | Tooth #43 Recession/Keratiniz Keratinised tissue (mm) |
|---|
| Baseline | 4/1 | 4/1 |
| 1-year follow-up | 1/3 | 1/2 |
| 4-year follow-up | 0/5 | 0/4 |
| 8-year follow-up | 0/5 | 0/4 |
| 12-year follow-up | 0/5 | 0/4 |
| 18-years follow-up | 0/5 | 0/4 |
Informed consent was obtained from the patient for the use of clinical images for the purpose of case presentation and documentation.
Discussion
The objectives of periodontal treatment include the establishment and maintenance of the gingival health and tooth-supporting structures, in addition to providing an acceptable aesthetic appearance to the natural teeth [2].
An epidemiological study by Susin C et al., showed that more than half of the subjects in the population studied presented gingival recession, the extent of gingival recession was more in males than females [3].
Recession at the buccal surfaces of the teeth can be seen in individuals even with good standards of oral hygiene maintenance whereas other surfaces may be involved in individuals with poor oral health conditions [4-7].
Certain types of gingival recession defects can be treated utilising different procedures such as Coronally Advanced Flaps (CAF) with or without mucosal grafts, Subepithelial Connective Tissue (SECT) grafts, Acellular Dermal Matrix (ADM) and guided tissue regeneration procedures [8-10].
A double-papilla flap was used in this case because of the wide papillae on each side of the operated site, which guaranteed more blood supply to the grafted tissue as well as to avoid a muscle pull from the vestibular area, which occurs if a coronal flap is utilised [11].
This case report with a long term follow-up showed that a long-term stability can be attained with a root coverage procedure using a connective tissue graft over previously restored noncarious cervical lesions. Present findings are in agreement with those of Goldstein M et al., who previously reported a long-term stability after a six-year follow-up for 27 teeth with carious roots (restored and unrestored), which were treated with SECT grafts [12,13]. In their study, the authors reported 92% root coverage for previously carious roots and 97% for intact roots. In addition, they reported complete root coverage in 44/60 patients. Furthermore, Santamaria MP et al., reported predictable results of using SECT grafts for gingival recessions associated with noncarious cervical lesions [14,15].
In a similar case report, Corsair reported a 100% root coverage after a seven-year follow-up of a previously restored root with class V composite restoration [16]. It was also noted that the zone of the attached gingiva increased. The 18-year follow-up photographs in the current report show more root coverage over time, which is known as a “creeping attachment” phenomenon [17].
A recent systematic review by Rovai ES et al., reported no significant influence of restoration on the root coverage procedure, which was also noted in this study as previously restored roots did not affect the end results [18].
Conclusion(s)
To our knowledge, this case report has the most extended follow-up period for the described procedure. This study showed that the placement of a SECT graft on previously restored root surfaces provided highly predictable and stable results.
Clinical Significance
Restoring a lost root structure with a SECT graft should provide long-lasting aesthetic results and stable marginal tissue.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 18, 2020
Manual Googling: Sep 18, 2020
iThenticate Software: Oct 28, 2020 (7%)
[1]. Miller PD Jr, A classification of marginal tissue recessionInt J Periodontics Restorative Dent 1985 5(2):08-13. [Google Scholar]
[2]. Newman MG, Takie HH, Klokkevold PR, Carranza FA, Carranza’s Clinical Periodontology 2012 Ed 11St. LouisSaunders Elsevier:608 [Google Scholar]
[3]. Susin C, Haas AN, Oppermann RV, Haugejorden O, Albandar JM, Gingival recession: Epidemiology and risk indicators in a representative urban Brazilian populationJ. Periodontol 2004 75(10):1377-86.10.1902/jop.2004.75.10.137715562916 [Google Scholar] [CrossRef] [PubMed]
[4]. Sangnes G, Gjermo P, Prevalence of oral soft and hard tissue lesions related to mechanical tooth cleansing proceduresCommunity Dent Oral Epidemiol 1976 4(2):77-83.10.1111/j.1600-0528.1976.tb01607.x1062255 [Google Scholar] [CrossRef] [PubMed]
[5]. Santarelli GA, Ciancaglini R, Campanari SG, Wennstrom JL, Lindhe J, Eneroth L, The prevalence and distribution of gingival recession in subjects with a high standard of oral hygieneJ Clin Periodontol 1994 21(1):57-63.10.1111/j.1600-051X.1994.tb00278.x8126246 [Google Scholar] [CrossRef] [PubMed]
[6]. Neely AL, Holford TR, Loe H, Anerud A, Boysen H, The natural history of periodontal disease in humans: Risk factors for tooth loss in caries-free subjects receiving no oral health careJ Clin Periodontol 2005 32(9):984-93.10.1111/j.1600-051X.2005.00797.x16104963 [Google Scholar] [CrossRef] [PubMed]
[7]. Baelum V, Fejerskov O, Karring T, Oral hygiene, gingivitis and periodontal breakdown in adult TanzaniansJ Periodontal Res 1986 21(3):221-32.10.1111/j.1600-0765.1986.tb01454.x2941555 [Google Scholar] [CrossRef] [PubMed]
[8]. Alghamdi H, Babay N, Sukumaran A, Surgical management of gingival recession: A clinical updateSaudi Dental J 2009 21(2):83-94.10.1016/j.sdentj.2009.07.00623960465 [Google Scholar] [CrossRef] [PubMed]
[9]. Sameera S, Nagasri M, Kumar PA, Indeevar P, Raviraj K, Musalaiah S, Comparison of two surgical techniques in the treatment of multiple gingival recessions sandwiched with a combination of A-PRF and L-PRFSaudi Dent J 2018 30(3):183-89.10.1016/j.sdentj.2018.03.00229942101 [Google Scholar] [CrossRef] [PubMed]
[10]. Al-Hamdan K, Long-term predictability of allogenic dermal matrix for root coverage: Three years observation period on 15 consecutive casesSaudi Dental J 2020 Available online 16 January 202010.1016/j.sdentj.2020.01.00133551623 [Google Scholar] [CrossRef] [PubMed]
[11]. Grupe HE, Warren RF Jr, Repair of gingival defects by a sliding flap operationJ Periodontol 1956 27(2):92-95.10.1902/jop.1956.27.2.92 [Google Scholar] [CrossRef]
[12]. Goldstein M, Naskatzky E, Goultschin J, Boyan B, Schwartz Z, Coverage of carious roots by a subepithelial connective tissue graftAm J Dent 2002 15(3):143-48. [Google Scholar]
[13]. Goldstein M, Naskatzky E, Goultschin J, Boyan BD, Schwartz Z, Coverage of previously carious roots is as predictable a procedure as coverage of intact rootsJ Periodontol 2002 73(12):1419-26.10.1902/jop.2002.73.12.141912546091 [Google Scholar] [CrossRef] [PubMed]
[14]. Santamaria MP, Feitosa D dS, Nociti FH Jr, Casati MZ, Sallum AW, Sallum EA, Cervical restoration and the amount of soft tissue coverage achieved by CAF: A 2-year follow-up randomized-controlled clinical trialJ Clin Periodontol 2009 36(5):434-41.10.1111/j.1600-051X.2009.01389.x19419445 [Google Scholar] [CrossRef] [PubMed]
[15]. Santamaria MP AG, Casati MZ, Nociti Júnior FH, Sallum AW, Sallum EA, Connective tissue graft plus resin-modified glass ionomer restoration for the treatment of gingival recession associated with non-carious cervical lesion: A randomized-controlled clinical trialJ Clin Periodontol 2009 36(9):791-98.10.1111/j.1600-051X.2009.01441.x19594663 [Google Scholar] [CrossRef] [PubMed]
[16]. Corsair A, Root coverage of a previously restored tooth. A case report with a 7-year follow-upClin Cosmet Investig Dent 2009 1:35-38.10.2147/CCIDE.S5856 [Google Scholar] [CrossRef]
[17]. Matter J, Free gingival graft and coronally repositioned flap. A 2-year follow-up reportJ Clin Periodontol 1979 6:437-42.10.1111/j.1600-051X.1979.tb01942.x295291 [Google Scholar] [CrossRef] [PubMed]
[18]. Rovai ES, Ambrosio LM, Morillo CM, Villar CC, Holzhausen M, Santamaria MP, Root coverage procedures in noncarious cervical lesions with and without restoration: A systematic review and meta-analysisInt J Periodontics Restorative Dent 2020 40(3):e127-35.10.11607/prd.428432233197 [Google Scholar] [CrossRef] [PubMed]