The Endoscopic Retrograde Cholangiopancreatography (ERCP) is a widely used advanced endoscopic procedure in the management of pancreatobiliary diseases. Selective cannulation of Common Bile Duct (CBD) is the rate limiting and challenging step in ERCP [1]. Atraumatic and quick biliary cannulation is desired for a successful ERCP in biliary interventions. Prolonged attempt at cannulation leads to endoscopist anxiety, unnecessary radiation exposure, increased patient morbidity, failure or aborting of procedure [2]. It also leads to significant adverse events such as perforation and pancreatitis [3,4]. Fatty meal has been proposed to stimulate gall bladder emptying and enhance the bile flow through the ampulla. It has also been proposed to relax the sphincter of Oddi. Studies which have compared non-fatty meal and fatty meal prior to ERCP have shown that oral administration of liquid fatty meal prior to ERCP make the biliary orifice more open with visible bile flow albeit with no difference in successful biliary cannulation rates [5,6].
Common Bile Duct (CBD) cannulation can also be facilitated by inhibition of intestinal motility which can be achieved by using intravenous glucagon [7]. Hyoscine-N-butyl bromide is utilised for this purpose in many centres due to its easy availability and low cost compared to glucagon [7]. It has already been shown that Hyoscine-N-butyl bromide and glucagon are equally effective in decreasing the duodenal motility during endoscopy [8]. Drotaverine hydrochloride is a papaverine analogue which causes smooth muscle relaxation by inhibiting phosphodiesterase IV. It is a non-anticholinergic, antispasmodic agent and hence, adverse effects which are seen with Hyoscine like palpitation, hypotension, nausea and vertigo are milder with Drotaverine. Drotaverine could be used as a suitable alternative to conventionally used hyoscine with similar effects on duodenal motility [9].
No study has been conducted to compare fatty meal with pharmacologic agents in facilitation of CBD cannulation during ERCP. Fatty meal, the action of which is physiological and without adverse effects when compared to potential haemodynamic adverse effects of Hyoscine-N-butyl bromide and Drotaverine hydrochloride, may be a suitable alternative to the widely used anti-motility pharmacologic agents during ERCP [10,11]. The aim of the study was to compare the effect of Fatty meal, Drotaverine hydrochloride and Hyoscine-N-butyl bromide with respect to duodenal anti-motility, cannulation time and haemodynamic adverse effects of the drugs used. The primary outcome measure was duodenal motility grade during the procedure. Duodenal motility was recorded by observing number of duodenal contractions occurring per minute with air insufflation in D2. Secondary outcome measures were cannulation time, percentage of successful selective cannulation and haemodynamic adverse effects.
Materials and Methods
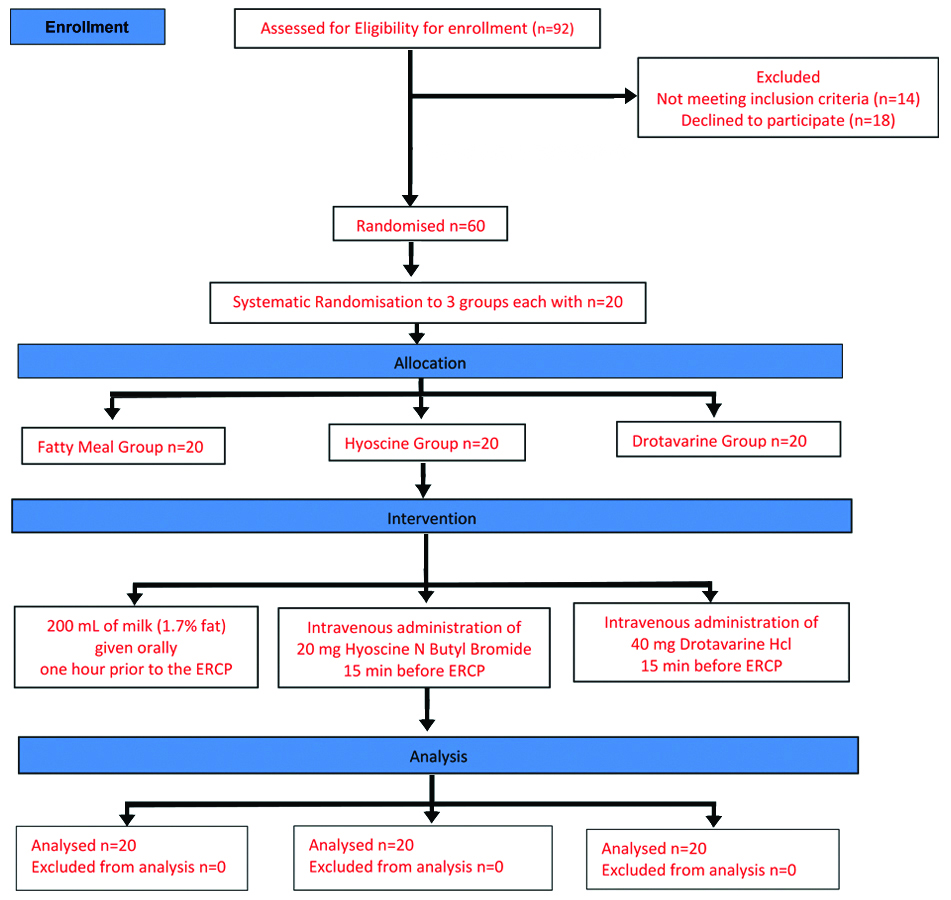
A randomised clinical study between fatty meal, hyoscine-N-butyl bromide and drotaverine was conducted in patients undergoing ERCP at the Department of Medical Gastroenterology, Madras Medical College and Rajiv Gandhi Government General Hospital, Chennai, Tamil Nadu, India, between June 2013 to March 2014. Systematic allocation of consecutive patients was done alternatively to one of the three groups viz., Fatty meal, Hyoscine and Drotaverine group. This study was approved by Institutional Ethics Committee (EC Reg No. ECR/270/Inst./TN/2013).
Sample size was calculated using the following formula:
n=Z2×p^ (1-p^)/E2, wheren, is the sample size of 60, Z is the z score at 80% confidence level, p^ is the population proportion derived from meta-analysis showing 85% successful cannulation in virgin papilla [12], E is the margin of error 6%.
Inclusion criteria: Sixty consecutive patients with consent, aged >18 years with normal appearing ampulla undergoing ERCP for the first time (virgin papilla) were included in the study.
Exclusion criteria: Patients with known allergy to milk, with glaucoma, with altered anatomy like Billroth II gastrectomy, obstructive uropathy, hypotension (systolic blood pressure <100 mmHg), impaired renal function (serum creatinine >1.5 mg/dL), second-degree and third-degree atrio-ventricular block, pregnant or breastfeeding women, congestive cardiac failure were excluded.
Ultrasonography of abdomen, Contrast-Enhanced Computed Tomography (CECT), Magnetic Resonance Cholangiopancreatography (MRCP) were done prior to the procedure. All patients planned for ERCP underwent pre-anaesthetic evaluation, baseline investigations like serum creatinine, intra-ocular pressure for glaucoma, electrocardiography, echocardiography and upper gastrointestinal endoscopy were done. Baseline duodenal motility was recorded on the day of ERCP by performing upper gastro-intestinal endoscopy after eight hour fasting and observing the number of duodenal contractions per minute in the second part of duodenum. Baseline heart rate and blood pressure were documented. Patients were consecutively allocated into the three groups. Fatty meal group received 200 mL of semi-skimmed milk (1.7% fat) orally one hour prior to the procedure to allow for gastric emptying. In Hyoscine group and Drotaverine group, Hyoscine-N-butyl bromide 20 mg and Drotaverine hydrochloride 40 mg, respectively, were administered intravenously 15 minutes before the procedure [Table/Fig-1].
The Endoscopic Retrograde Cholangiopancreatography (ERCP) procedure was done under IV sedation of pentazocine 30 mg with promethazine 50 mg administered slowly. All ERCPs were done using Pentax Duodenoscope by the same endoscopist with expertise of performing over 2000 ERCPs. The presence or absence of bile tinge at major papillary orifice prior to cannulation attempt was recorded. Haemodynamic parameters were recorded during the ERCP procedure with recording of heart rate and BP every three minutes. Blood pressure was recorded manually using mercury sphygmomanometer. Duodenal contraction rate was recorded as number of duodenal contractions per minute by observing duodenal motility from the time of scope insertion to time of cannulation of the desired duct. Success of cannulation without performing needle knife sphincterotomy, time taken to achieve successful cannulation into the desired ducts (which is defined as the time interval between the satisfactory positioning of duodenoscope in D2 with proper visualisation) and orientation of ampulla and fluoroscopic confirmation of wire guided cannulation of desired duct, were noted. Haemodynamic adverse effects of drugs if any, were noted. No additional dosage or supplemental drugs were administered to achieve duodenal hypomotility.
Statistical Analysis
Statistical analysis was done by Chi-square test and ANOVA test and using SPSS 16.0 version software. The duodenal motility, cannulation success, cannulation time, adverse haemodynamic effects were analysed and compared between the three groups. A p-value <0.05 was considered to be statistically significant.
Results
There was fairly even distribution of cases with respect to age and sex across all 3 groups [Table/Fig-2].
| Age (years) | Number of cases (N, %) | Sex | Number of cases (N, %) |
|---|
| Hyoscine group | Drotaverine group | Fatty meal group | Chi-square test p-value | | Hyoscine group | Drotaverine group | Fatty meal group | Chi-square p-value |
|---|
| 20-30 | 3 (15%) | 3 (15%) | 4 (20%) | 0.84 | Male | 12 (60%) | 13 (65%) | 15 (75%) | 1 |
| 31-40 | 4 (20%) | 4 (20%) | 5 (25%) |
| 41-50 | 5 (25%) | 7 (35%) | 3 (15%) |
| 51-60 | 4 (20%) | 3 (15%) | 6 (30%) | Female | 8 (40%) | 7 (35%) | 5 (25%) | 1 |
| 61-70 | 3 (15%) | 2 (10%) | 2 (10%) |
| >70 | 1 (5%) | 1 (5%) | 0 |
Visualisation of bile stain at papillary orifice and thus facilitation of identification of the papillary orifice was seen more frequently in fatty meal group when compared to the other two groups [Table/Fig-3].
Bile stain at major papillary orifice.
| Groups | Bile tinge present | Bile tinge absent | Chi-squarep-value |
|---|
| Overall | Fatty meal vs. Hyoscine | Fatty meal vs. Drotaverine | Drotaverine vs. Hyoscine |
|---|
| Fatty meal group | 16 | 04 | 0.029 | 0.09 | 0.04 | 0.52 |
| Hyoscine group | 8 | 12 |
| Drotaverine group | 10 | 10 |
Lower cannulation success was seen in patients with CBD stricture in all the groups. At p<0.05, there is no statistically significant difference in successful cannulation rates between the three groups. Comparison among any two groups also did not show statistical significance in cannulation success [Table/Fig-4].
Diagnosis and outcome of cannulation attempt.
| Diagnosis and Cannulation Success | | Group |
|---|
| Hyoscine | Drotaverine | Fatty meal |
|---|
| Number of cases/Successful cannulation (%) | CBD stone and sequelae | 7/5 (71.4%) | 9/6 (66.6%) | 9/7 (77.7%) |
| CBD stricture | 4/2 (50%) | 3/2 (66.6%) | 2/1 (50%) |
| Bile leak | 1/1 (100%) | 1/1 (100%) | 1/1 (100%) |
| Cholangio carcinoma | 4/2 (50%) | 3/3 (100%) | 2/1 (50%) |
| Pancreatic Duct Leak | 1/1 (100%) | 0/0 | 2/2 (100%) |
| Carcinoma pancreas | 0/0 | 2/2 (100%) | 0/0 |
| Chronic pancreatitis and sequelae | 3/3 (100%) | 2/2 (100%) | 4/2 (50%) |
| Overall cannulation successNumber of cases/Successful cannulation (%) | | 20/14 (70%) | 20/16 (80%) | 20/14 (70%) |
| Overall cannulation success analysisChi-square statistics (p-value) | | 0.681 (p=0.711) |
| Cannulation success analysis between groupsChi-square statistic (p-value) | | Fattymeal vs. Hyoscine | Fattymeal vs. Drotaverine | Drotaverine vs. Hyoscine |
| | 0 (p=1)* | 0.53 (p 0.46)** | 0.53 (p 0.46)** |
*The Chi-square statistics with Yates correction is 0.119. The p-value is 0.73007. Not significant as p<0.05
**The Chi-square statistics with Yates correction is 0.1333. The p-value is 0.715001. Not significant as p<0.05
The baseline duodenal motility reduced drastically in all three groups after intervention. The p-value is 0.567, showing that there was no statistically significant difference in mean reduction of duodenal motility after intervention between the 3 groups at p<0.05. However, at p<0.05 the change in heart rate and BP variability was statistically significant for Hyoscine group. Between Drotaverine and Fatty meal group there was no significant difference in variation of haemodynamic parameter [Table/Fig-5].
Primary and secondary outcome of intervention.
| Parameters | Hyoscine group Mean±SD | Drotaverine group Mean±SD | Fatty meal group Mean±SD | ANOVA testp-value |
|---|
| Overall | Fatty meal vs. Hyoscine | Fatty meal vs. Drotaverine | Drotaverine vs. Hyoscine |
|---|
| Duodenal motility/min (Baseline) | 14.1±2.118 | 13.75±1.996 | 13.95±1.532 | 0.843 | 0.79 | 0.72 | 0.59 |
| Duodenal motility/min (During procedure) | 0.4±0.860 | 0.7±1.144 | 0.35±0.909 | 0.478 | 0.85 | 0.29 | 0.35 |
| Duodenal anti-motility/min | 13.7±2.319 | 13.05±2.188 | 13.6±1.635 | 0.567 | 0.87 | 0.37 | 0.36 |
| Cannulation time (mins) | 4±1.764 | 4.6±2.769 | 5±1.651 | 0.464 | 0.13 | 0.64 | 0.50 |
| Heart rate variation/min | 51.5±12.874 | 24.2±8.433 | 24.4±8.834 | <0.05 | <0.05 | 0.94 | <0.05 |
| Blood pressure difference systolic mm/Hg | 18.3±7.713 | 9.00±5.712 | 10.4±4.661 | <0.05 | <0.05 | 0.40 | <0.05 |
| Blood pressure difference diastolic mm/Hg | 15.7±9.091 | 8.70±5.630 | 8.6±3.315 | 0.001 | 0.002 | 0.94 | 0.006 |
Discussion
The present randomised trial might be the first study to compare the effect of fatty meal with Drotaverine hydrochloride and Hyoscine-N-butyl bromide in facilitation of cannulation during ERCP. The duodenal contraction rates, time taken for cannulation, cannulation success, and the haemodynamic changes during ERCP were studied. Exposure of small intestine to dietary fat has been shown to stimulate the release of a number of gastrointestinal hormones, including CCK (Cholecystokinin) [13] which stimulate gallbladder contraction, decrease sphincter of Oddi baseline pressure [14], and aid in emptying of bile into duodenum [13]. Hence, in the present study, the papillary orifice was easily identifiable with fatty meal due to bile flow and staining of the mucosa at the site. Barrie M et al., showed that the orifice of the CBD/pancreatic duct was much more easily identified in the group which ingested fatty meal compared to non-fatty meal group, which served as control. The fatty meal group had a shorter mean and median deep CBD cannulation time. There was no complication, including aspiration with the liquid meals given shortly before the ERCP procedure [5]. The mean deep cannulation time was 8 minutes, compared to the slightly shorter cannulation time of 5 minutes in the fatty meal group of this study. We did not find any significant difference in the cannulation time or cannulation success between the three groups in this study.
Heddle R et al., has shown that the dietary fat interacts with receptors in small intestine and inhibit gastric emptying and duodenal contractility [15]. Similarly, in the current study there was a significant decrement of duodenal motility in the fatty meal group. This was comparable to the anti-motility effects of pharmacologic agents Hyoscine and Drotaverine in the other two groups. Though the duodenal anti-motility effect, cannulation time, cannulation success rates were comparable between the three groups, the haemodynamics was adversely affected in the Hyoscine group which caused higher incidence of tachycardia and variation in blood pressure compared to the Drotaverine and fatty meal group. This finding was similar to the study by Salmanroghani H et al., in which they compared the efficacy and safety of low dose (5 mg) versus usual dose (10 mg) of Hyoscine during ERCP and showed higher incidence of tachycardia with the use of usual dose (10 mg) hyoscine compared to low dose (5 mg) during ERCP [16]. Several other studies have shown use of dose of 20 mg [17] and 40 mg [18] of Hyoscine in gastrointestinal endoscopy, however, significant haemodynamic instability with p<0.001 was noted by Mui LM et al., with use of higher dose of 40 mg of intravenous Hyoscine [18]. In the current study, 20 mg of Hyoscine-N-Butyl bromide was administered intravenously once 15 minutes prior to beginning of the procedure. No further administration of antispasmodics was done.
Unlike, Salmanroghani H et al., observation of hypotension in their study cohort of older patients, this study did not show any incidence of hypotension and only had rise in BP from baseline in Hyoscine group [16]. The rise in BP was significant at p<0.05 in Hyoscine group compared to Fatty meal and Drotaverine group. Intraprocedural hypotension to hyoscine was not seen in this study probably due to careful exclusion of patients with heart failure, and majority of patients were younger <61 years (80%). The rise in BP during ERCP has also been shown in other studies. Study on cardiovascular complications of ERCP by Fisher L et al., showed significant haemodynamic change with rise in heart rate and BP during ERCP, majority of patients in their study received IV Hyoscine-N-Butyl bromide for duodenal anti-motility [19]. Similarly, in this study, the mean increase in heart rate from baseline was higher at 51.5/minute in Hyoscine group as compared to 24.2/minute and 24.4/minute in Drotaverine and Fatty meal group respectively. The mean intraprocedural variation in BP was also higher in Hyoscine group at 18.3 mmHg systolic and 15.7 mmHg diastolic as compared to 9 mmHg systolic/8.7 mmHg diastolic for Drotaverine and 10.4 mmHg systolic/8.6 mmHg diastolic in fatty meal group. Apart from pharmacologic agents used, haemodynamic changes can also occur during ERCP due to several other factors including advanced age and pre-existing cardiovascular disease [19]. Tønnesen H et al., showed that endoscopy caused significant increase in norepinephrine and cortisol levels along with a significant peak in heart rate (76 to 90/min) and rise in mean arterial blood pressure (97 to 111 mmHg) and attributed this change to endocrine stress response [20]. This explains the variation in heart rate and BP seen in all three groups in this study, however, the adverse haemodynamic change was more pronounced in Hyoscine group. This finding re-emphasises that the GI endoscopist should be aware of the potential harmful effects of Hyoscine which is known to cause tachycardia and BP variation through its anti-cholinergic effects especially in older individuals [11,20]. Anaphylactic reactions have also been reported to IV Hyoscine [12]. The tachycardia, hypotension or anaphylaxis can be more serious in patients with underlying cardiac disease such as heart failure, coronary artery disease, cardiac dysrhythmia or hypertension [21]. It is therefore advisable to avoid the use of Hyoscine during endoscopic procedures in patients who have significant cardiac co-morbidity. Drotaverine, a non-anticholinergic antispasmodic, has been showed to cause minor adverse effects such as hypotension, vertigo, nausea, and vomiting [13]. However, no adverse effects were seen in this study in Drotaverine group.
Limitation(s)
Being a time bound study in the setting of academic trial, convenient sampling was done where patients meeting study criteria within the limited study duration presenting to the institution for ERCP and willing to give consent for enrollment in the study were included, hence the sample size in this study is small with lower confidence level.
Conclusion(s)
Fatty meal is not inferior to the conventionally used Hyoscine or its alternate Drotaverine for its anti-motility effect on the duodenum during ERCP. The cannulation time is no different within the groups. The identification of ampulla was easier with the fatty meal group. There is a possibility of higher variability in pulse rate and BP in patients with the use of hyoscine-N-butyl bromide which may be detrimental in patients with ischemic heart disease. Hence, fatty meal can be a safe regular dietary measure to aid in ERCP cannulation without usage of antispasmodic pharmacologic agents, thereby avoiding possible adverse effects of drugs.
Further larger randomised trials are required to confirm the efficacy of fatty meal as a safe alternative to pharmacologic agents in performing ERCP.
*The Chi-square statistics with Yates correction is 0.119. The p-value is 0.73007. Not significant as p<0.05
**The Chi-square statistics with Yates correction is 0.1333. The p-value is 0.715001. Not significant as p<0.05