Comparison of Efficacy of Alginate Filler Dressings with Conventional Saline Dressings for Cavity Wounds in Diabetic Foot Ulcer- A Prospective Cohort Study
Tharun Ganapathy Chitrambalam1, Pradeep Joshua Christopher2, Jeyakumar Sundaraj3, Ramyasree Paladugu4, Sundeep Selvamuthukumaran5
1 Associate Professor, Department of General Surgery, SRM University, Chennai, Tamil Nadu, India.
2 Postgraduate Student, Department of General Surgery, SRM University, Chennai, Tamil Nadu, India.
3 Professor and Head, Department of General Surgery, SRM University, Chennai, Tamil Nadu, India.
4 Postgraduate Student, Department of General Surgery, SRM University, Chennai, Tamil Nadu, India.
5 Postgraduate Student, Department of General Surgery, SRM University, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Pradeep Joshua Christopher, Potheri, SRM Nagar, Kattankulathur, Chennai-603203, Tamil Nadu, India.
E-mail: pdp.joshua@gmail.com
Introduction
Diabetic foot ulcers are associated with 25% of patients with Diabetes Mellitus (DM). These diabetic foot ulcers if not given appropriate care at the right time can lead to amputations and poor quality of life. Alginate dressings are newer and help in faster healing of cavity wounds in diabetic foot ulcer.
Aim
To compare the advantages of alginate dressings over conventional saline dressings in cavity wounds of diabetic foot ulcer patients.
Materials and Methods
A single centre prospective longitudinal cohort study was conducted on 88 patients with diabetic foot ulcers randomising equally into two groups containing 44 patients in each group in a tertiary care hospital. The wounds of all patients included in the study were thoroughly debrided and initial assessment was done using the Pressure Ulcer Scale for Healing (PUSH) scoring system. The patients were started on alginate dressings in one group and saline dressings in other group and were assessed after two and four weeks. The reduction in the surface area of the wound, reduction in the exudate amount, type of the tissue over the ulcer and reduction in the bacterial load (wound cultures) of the ulcers were studied. The statistical analysis were done using Statistical Package for the Social Sciences (SPSS) software version 21. The statistics were done using independent sample tests (Levene’s test for equality of variances and t-test for equality of means), Mann-Whitney test and Wilcoxon test.
Results
The results of wound assessment before dressings, at two weeks and at the end of four weeks are as follows: The mean (SD) reduction in wound surface area was 9.07 (1.634) to 6.89 (1.434) to 4.68 (1.272) for alginate group and 9.25 (2.059) to 8.00 (1.905) to 6.50 (1.650) for saline group. The mean (SD) reduction of the exudate amount was 2.02 (0.505) to 1.09 (0.473) to 0.14 (0.347) for alginate group and 1.98 (0.590) to 1.43 (0.625) to 0.75 (0.615) for the saline group. The mean (SD) for tissue type of cavity wounds assessed via PUSH scoring was reduced from 2.30 (0.701) to 0.16 (0.370) for the alginate group in comparison to 2.32 (0.740) to 0.77 (0.743) for the saline group at the end of four weeks. On evaluation of the wound cultures; 6 out of 44 patients (13.6%) were culture positive in the alginate group while 30 out of 44 patients (68.2%) were culture positive from the saline group at the end of four weeks. All the above results were statistically significant with a p-value of 0.001.
Conclusion
Alginates dressings are superior to saline dressings in terms of reduction in the size of the ulcer and control of microbial activity in diabetic foot. Alginate absorbs large amount of exudates and fill in irregular shaped cavities which are ideal in treating cavity wounds in diabetic foot syndrome.
Debridement, Diabetes mellitus, Diabetes mellitus complications
Introduction
DM is a heterogeneous metabolic disorder characterised by the presence of hyperglycaemia due to impairment of insulin secretion, defective insulin action or both [1]. DM is considered a major health problem with a worldwide increase in its prevalence and is the 7th major cause for morality [2]. Diabetic foot ulcers are associated with 25% of patients with DM typically leading to life-threatening amputations and poor quality of life [3]. For every 20th second a lower limb is lost worldwide in diabetics, which is considered to be the most common cause of non-traumatic lower limb amputations [4]. In India, about 45,000 lower limbs are amputated every year out of which most of them can be prevented if managed properly [5]. A cavity wound is defined as any wound that extends beneath the layers of the dermis, extending in potential spaces to involve underlying structures such as fascia, tendons, muscle and bone [6,7]. Various measures have been undertaken in the past for healing of diabetic ulcers starting from normal saline dressings, growth factors like Platelet-Derived Growth Factor β (PDGF-beta), and bioengineered skin substitutes to the use of negative pressure wound therapy [8]. However, considering the affordability of the patients, most of them are out of their reach. One such cost effective yet efficacious material which can be used for managing cavity wounds are Alginate filler wound dressings.
Alginates are found in marine brown algae (pheophycea) with its cell wall constituent in the form of alginic acid, which was first extracted by a British chemist Stanford in 1881. In the past, alginates have been used in food and textile industries. They were reportedly used by sailors to heal wounds and hence called as the ‘mariner’s cure’. In 1947, Blaine used alginates for treating experimentally produced burns. Alginic acid is comprised of both mannuronic acid (M) and guluronic acid (G) [9,10]. They are manufactured based on an ion-exchange reaction; the soluble sodium alginates produced from the purification and extraction of the seaweed is dissolved in water to produce a colloidal solution which is then passed through a bath of calcium ions thereby converting to insoluble calcium or calcium sodium alginates [10]. Based on their ratio of guluronic acid and mannuronic acid, they can absorb 15-20 times its own weight [11]. The major properties of alginates include the absorption of exudates that can prevent maceration of the wound, biodegradability by aiding significant inhibition of Staphylococcus aureus, Streptococcus pyogenes or Bacteroides fragilis and haemostasis [12].
Alginate dressings do not adhere to the wound surface and can be washed off easily with irrigation of saline which reduces the risk of wound infection [11]. The aim of this study was to compare the efficacy of alginate dressings with that of conventional saline dressings in terms of the rate of reduction of the mean surface area of the cavity wounds.
Materials and Methods
A single centre prospective longitudinal cohort study was conducted on 88 patients with diabetic foot ulcers from August 2018 to August 2020 dividing equally 44 patients in each group in a tertiary care hospital. The study was initiated after Institutional Ethical Committee clearance, IEC 1624 dated 27/2/2019. Sample size was calculated based on a study conducted by Donaghue VM et al., on the efficacy and safety of a collagen-alginate topical wound dressing (FIBRACOL Collagen-Alginate Wound Dressing) in the treatment of diabetic foot ulcers was compared with that of regular gauze moistened with normal saline, which showed standard deviation of alginate dressings (s1) and saline dressings (s2) as 6 and 26, respectively while mean of alginate dressings (μ1) and saline dressings (μ2) as 80.6 and 61.1, respectively, which when applied on n=2(zγ+z1-β)2 (s12+s22)/(μ1-μ2)2 gave sample size as 39.30 (40) which when calculated with 10% of dropouts finalised as 44 in each group [13]. Simple randomisation was done. Diabetic foot ulcer patients aged between 12 to 75 years giving consent were included in the study and were explained in their native language about the study in detail. The patients with peripheral vascular diseases, skin malignancies, venous or arterial ulcers, immunocompromised patients or with underlying osteomyelitis were excluded from the study. All the dressings were done by the same group of doctors working in the same surgical unit in order to avoid any discrepancies and were followed-up on a daily basis. The work has been reported in line with the STROCSS criteria [14].
A total of 88 patients were included in the study, one group was managed using alginate dressings [Table/Fig-1], while the other group using conventional saline dressings [Table/Fig-2]. After bedside debridement of the wound without anaesthesia, initial wound assessment was made using PUSH before starting the patient on dressings [Table/Fig-3] [15]. The patients were started on saline or alginate dressing depending on group code and were monitored at two week and at the end of four weeks. The components of the PUSH score include, length×width in square centimetres (wound area), exudate amount and tissue type. These components are further given a sub score. Wound area is given a score from 0 to 10 based on size of the ulcer in Cm Sq. Based on the amount of exudate from the ulcer, it is sub scored from 0 to 3 as none, mild, moderate and severe. Based on the tissue type, it is sub scored from 0 to 4 with 0 as closed, 1 for epithelial tissue, 2 for granulation tissue, 3 for slough and 4 for necrotic tissue.
Alginate application (Group-1).

Saline dressings (Group-2).

| Length × Width (Cm2) | 0 | 1<0.3 | 20.3-0.6 | 30.7-1.0 | 41.1-2.0 | 52.1-3.0 | Sub-Score |
| | 63.1-4.0 | 74.1-8.0 | 88.1-12.0 | 912.1-24.0 | 10>24.0 | |
| Exudate amount | 0None | 1Mild | 2Moderate | 3Severe | | | Sub-Score |
| Tissue type | 0Closed | 1Epithelial tissue | 2Granulation tissue | 3Slough | 4Necrotic Tissue | | Sub-Score |
| | | | | | | TOTAL SCORE |
Statistical Analysis
The statistical analysis were done using SPSS software version 21. The statistics were done using Levene’s test (for equality of variances and t-test for equality of means), Pearson Chi-square test and Mann-Whitney test and Wilcoxon test.
Results
A total of 88 patients were included in the study out of which 56 were males and 32 were females. In males, 24 patients were included in alginate group and 32 in saline group. In females, 20 patients were included in alginate group and 12 patients were included in saline group.
At two weeks, the mean (SD) of alginate group was reduced from 9.07 (1.634) to 6.89 (1.434) while the mean (SD) of the saline group was reduced from 9.25 (2.059) to 8.00 (1.905). At four weeks, the mean (SD) of alginate group was further reduced to 4.68 (1.272) while the mean (SD) of the saline group was reduced to 6.50 (1.650) [Table/Fig-4].
Reduction in wound area (p-value was calculated using t-test for equality of mean).
| Wound area (cm2) | Group | N | Mean±SD | p-value |
|---|
| On admission | Alginate | 44 | 9.07±1.634 | 0.647 |
| Saline | 44 | 9.25±2.059 |
| Two weeks | Alginate | 44 | 6.89±1.434 | 0.003 |
| Saline | 44 | 8.00±1.905 |
| Four weeks | Alginate | 44 | 4.68±1.272 | 0.001 |
| Saline | 44 | 4.68±1.272 |
p-value less than 0.05 was considered as statistically significant
The mean (SD) of the alginates at two weeks were reduced from 2.02 (0.505) to 1.09 (0.473) in comparison to saline group from 1.98 (0.590) to 1.43 (0.625). The mean (SD) of the alginates at four weeks were further reduced to 0.14 (0.347) in comparison to saline group from 0.75 (0.615) [Table/Fig-5].
Reduction in exudate amount (p-value was calculated using t-test for equality of mean).
| Exudate amount | Group | N | Mean±SD | p-value |
|---|
| On admission | Alginate | 44 | 2.02±0.505 | 0.699 |
| Saline | 44 | 1.98±0.590 |
| Two weeks | Alginate | 44 | 1.09±0.473 | 0.005 |
| Saline | 44 | 1.43±0.625 |
| Four weeks | Alginate | 44 | 0.14±0.347 | 0.001 |
| Saline | 44 | 0.75±0.615 |
p-value less than 0.05 was considered as statistically significant
The mean (SD) was found to be reduced from 2.30 (0.701) to 0.16 (0.370) for the alginate group in comparison to 2.32 (0.740) to 0.77 (0.743) for the saline group at the end of four weeks [Table/Fig-6].
Tissue type (p-value was calculated using t-test for equality of mean).
| Tissue type | Group | N | Mean±SD | p-value |
|---|
| On admission | Alginate | 44 | 2.30±0.701 | 0.883 |
| Saline | 44 | 2.32±0.740 |
| Two weeks | Alginate | 44 | 1.16±0.608 | 0.027 |
| Saline | 44 | 1.45±0.627 |
| Four weeks | Alginate | 44 | 0.16±0.370 | 0.001 |
| Saline | 44 | 0.77±0.743 |
p-value less than 0.05 was considered as statistically significant
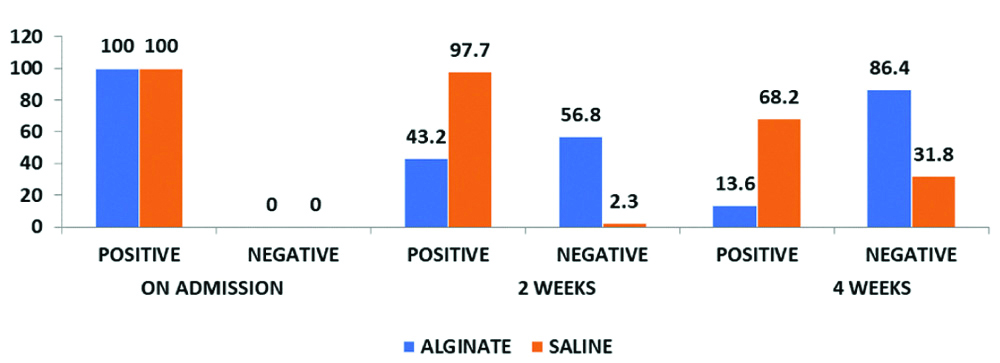
On evaluation of the wound cultures 19 out of 44 patients (43.2%) were culture positive in the alginate group while 43 out of 44 patients (97.7%) were culture positive from the saline group at two weeks. At the end of four weeks; 6 out of 44 patients (13.6%) were culture positive in the alginate group while 30 out of 44 patients (68.2%) were culture positive from the saline group [Table/Fig-7].
Wound culture (p-value 0.001, calculated using Pearson Chi-square test).
In overall comparison among the groups, the PUSH score on admission for both saline and alginate group was 13.57 and 13.45, respectively, which after four weeks were found to be reduced to 8.02 and 4.98 respectively. On further statistical evaluation with Mann-Whitney and Wilcoxon tests, alginate dressing group were found to be statistically significant [Table/Fig-8].
Overall comparison with statistical significance- Results of Mann-Whitney and Wilcoxon tests.
| PUSH Score | Group | N | Mean±SD | | Wilcoxon W | Z | p-value |
|---|
| On admission | Alginate | 44 | 13.45±1.873 | 937.500 | 1927.500 | 0.258 | 0.797 |
| Saline | 44 | 13.57±2.193 |
| On discharge | Alginate | 44 | 4.98±1.320 | 186.500 | 1176.500 | -6.593 | 0.001 |
| Saline | 44 | 8.02±1.798 |
p-value less than 0.05 was considered as statistically significant
Discussion
The treatment of diabetic foot ulcers in highly exuding cavity wounds is a challenge. The treatment in such wounds includes debridement of the wound, managing the infection, revascularisation procedures if needed and off-loading of the ulcers [16]. There are several dressing modalities available at present that aids not only in protecting the wound but also promote faster wound healing. An ideal dressing material must be able to remove exudates and toxic components, should maintain a moist environment at wound-dressing interface, should be impermeable to micro-organisms, allowing gaseous exchange, should be removed easily and most importantly should be cost-effective [17]. The use of alginate dressings for cavity wounds was found to be efficacious in many aspects. In terms of wound surface area, in this study, there was marked reduction in the size of the wound in patients who were subjected to alginate dressings when compared to that of saline dressings which was statistically significant. Donaghue VM et al., in evaluating the efficacy and safety of collagen-alginate topical wound dressing (FIBRACOL Collagen Alginate wound dressing) in the treatment of diabetic foot ulcers found the reduction in wound surface area was statistically significant (p=0.0049) with alginate dressings and concluded that collagen-alginate dressings is more effective than the conventionally used saline dressings [13].
In promoting the wound healing by reducing the exudate amount or by increasing the absorption of the exudate, alginates showed marked improvement with reduction in mean of 2.02 to 0.14 within a span of four weeks when compared to that of a reduction from 1.98 to 0.75 in case of saline dressings. In a study conducted by Jones V concluded that alginates are considered to be a comfortable and cost-effective alternative dressing to other dressings especially in cases of moderate to heavily exuding wounds. The ability of the alginates to absorb large amounts (15-20 times its weight) of exudate and fill irregularly shaped cavity wounds was emphasised in this study [11]. In contrast to the above mentioned study, Dumville JC et al., in his research paper stated no significant research evidence to prove alginate dressing to be more efficacious than other dressings, yet they concluded that decision makers may wish to consider certain aspects such as dressing cost and wound management properties like exudate management in alginate dressings [18].
Another important entity that has been compared as per PUSH scaling system is the improvement in the tissue type. In this study, several ulcers which were initially covered with necrotic tissues or slough were either resurfaced completely or healed with epithelial tissues after application of alginate dressings over a period of four weeks. The patients with saline dressings were still granulating over a 4-week period without epithelisation. This was confirmed on PUSH score with reduction in mean from 2.30 to 0.16 for alginate dressings and 2.32 to 0.77 for saline dressings. In addition to these three attributes of PUSH scale, the 4th entity that has been compared in this study is the reduction or nullification of the bacterial load. The wound swabs taken at the time of admission of 88 patients forming the study population were positive with growth of a variety of organisms. On follow-up wound swabs at two weeks, only 43% of the patients in alginate group were positive while 97% in saline group were still positive for organisms. After four weeks about 13.6% (6) patients in alginate group were culture positive in comparison to 68.2% (30) patients culture positivity in saline dressing group. In a study conducted by Naik BM et al., comparing the efficacy between alginate dressings and povidone iodine dressings, wound culture swabs were compared but there was no statistical significance between the groups [19].
The strength of the study is the sample size with statistically significant results and all the dressings were done by the team of doctors working in the same surgical unit. Alginates are capable of absorbing 15-20 times of its own weight and are useful in highly exuding cavity wounds. We recommend the routine use of alginate dressings in non-healing highly exuding cavity wounds.
Limitation(s)
The limitations of the study was, firstly alginate dressings were compared with conventional saline dressings and not with proven advanced biological substitutes or negative pressure wound therapy and secondly cost-analysis was not done.
Conclusion(s)
Alginates dressings are superior to saline dressings in terms of reduction in the size of the ulcer and control of microbial activity in diabetic foot. Alginates absorb large amounts of exudates and fill in irregular shaped cavities which are ideal in treating cavity wounds in diabetic foot syndrome.
p-value less than 0.05 was considered as statistically significant
p-value less than 0.05 was considered as statistically significant
p-value less than 0.05 was considered as statistically significant
p-value less than 0.05 was considered as statistically significant
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Aug 27, 2020
Manual Googling: Sep 28, 2020
iThenticate Software: Oct 27, 2020 (5%)
[1]. Diabetes Canada Clinical Practice Guidelines Expert CommitteePunthakee Z, Goldenberg R, Katz P, Definition, Classification and Diagnosis of Diabetes, Prediabetes and Metabolic SyndromeCan J Diabetes 2018 42(Suppl 1):S10-S15.10.1016/j.jcjd.2017.10.00329650080 [Google Scholar] [CrossRef] [PubMed]
[2]. WHO. Top 10 causes of death. World Health Organisation 2017. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death [Google Scholar]
[3]. Singh N, Armstrong DG, Lipsky BA, Preventing foot ulcers in patients with diabetesJAMA 2005 293(2):217-28.10.1001/jama.293.2.21715644549 [Google Scholar] [CrossRef] [PubMed]
[4]. The International Working Group on the Diabetic Foot. IWGDF Guidance on the diagnosis and management of foot infections in persons with diabetes 2017. http://iwgdf.org/ Accessed 10 Sept 2017 [Google Scholar]
[5]. Jain AKC, Vishwanath S, Studying major amputations in a developing country using Amit Jain’s typing and scoring system for diabetic foot complications- Time for standardization of diabetic foot practiceInt Surg J 2015 2:26-30.10.5455/2349-2902.isj20150205 [Google Scholar] [CrossRef]
[6]. Timmons J, Cooper P, How to systematically assess a patient with a cavity woundWounds UK 2008 4(2):04-10. [Google Scholar]
[7]. Williams C, Treatment of cavity woundsPractice Nursing 1997 8:31-33.10.12968/pnur.1997.8.13.31 [Google Scholar] [CrossRef]
[8]. Alexiadou K, Doupis J, Management of diabetic foot ulcersDiabetes Ther 2012 3(1):410.1007/s13300-012-0004-922529027 [Google Scholar] [CrossRef] [PubMed]
[9]. Harding KG, The future of wound healing. In: Leaper DJ, Harding KJ, editorsWounds: Biology and management 1998 OxfordOxford University Press:191 [Google Scholar]
[10]. Yorke M, Spruce P, An update on the use of alginate dressings in the diabetic footThe Diabetic Foot Journal 2015 18:96-100. [Google Scholar]
[11]. Jones V, Alginate dressings and diabetic foot lesionsThe Diabetic Foot Journal 1999 2:08-14. [Google Scholar]
[12]. Cazzaniga AL, Marshall DA, Mertz PM, The effect of calcium alginate dressing on the multiplication of bacterial pathogens in vitroProceedings of the 5th annual symposium on Advanced Wound Care (NewOrleans) 1992 :139 [Google Scholar]
[13]. Donaghue VM, Chrzan JS, Rosenblum BI, Giurini JM, Habershaw GM, Veves A, Evaluation of a collagen-alginate wound dressing in the management of diabetic foot ulcersAdv Wound Care 1998 11(3):114-19.PMID: 9729942 [Google Scholar]
[14]. Agha RA, Borrelli MR, Vella-Baldacchino M, Thavayogan R, Orgill DP, STROCSS GroupThe STROCSS statement: Strengthening the Reporting of Cohort Studies in SurgeryInt J Surg 2017 46:198-202.doi: 10.1016/j.ijsu.2017.08.586. Epub 2017 Sep 7. PMID: 28890409; PMCID: PMC6040889 [Google Scholar]
[15]. George-Saintilus E, Tommasulo B, Cal CE, Hussain R, Mathew N, Dlugacz Y, Pressure ulcer PUSH score and traditional nursing assessment in nursing home residents: Do they correlate?J Am Med Dir Assoc 2009 10(2):141-44.10.1016/j.jamda.2008.10.01419187884 [Google Scholar] [CrossRef] [PubMed]
[16]. Doupis J, Veves A, Classification, diagnosis, and treatment of diabetic foot ulcersWounds 2008 20(5):117-26.PMID: 25942412 [Google Scholar]
[17]. Harding KG, Jones V, Price P, Topical treatment: which dressing to chooseDiabetes Metab Res Rev 2000 16(Suppl 1):S47-50.10.1002/1520-7560(200009/10)16:1+<::AID-DMRR133>3.0.CO;2-Q [Google Scholar] [CrossRef]
[18]. Dumville JC, O’Meara S, Deshpande S, Speak K, Alginate dressings for healing diabetic foot ulcersCochrane Database Syst Rev 2013 2013(6):CD00911010.1002/14651858.CD009110.pub323799857 [Google Scholar] [CrossRef] [PubMed]
[19]. Naik BM, Kulkarni SV, Narayana S, Prabusankar P, A comparative study between efficacy of silver & calcium alginate wound dressing vs in povidone: Odoine wound dressings in chronic non-healing ulcersJournal of Evolution of Medical and Dental Sciences 2013 2(23):4173-76.10.14260/jemds/818 [Google Scholar] [CrossRef]