Rise in Road Traffic Accidents (RTAs) are a major cause of increasing human mortality and morbidity in the current era. One of the injuries seen in such cases is the fracture of distal tibia. These fractures are known to be notorious and are difficult to treat even with advancement in the field. Another notable factor predisposing to distal tibia fractures is osteoporosis posing a higher risk to the elderly population. With the increasing life expectancy number of aged in the society has increased and so has the incidence of distal tibia fractures [1,2]. As these fractures are adjacent to the ankle joint, regaining full ankle movements after fracture union is a challenge. Soft-tissue damage, comminution and fractures extension into the ankle joint leads for disappointing results irrespective of the treatment modality used. Comprehensive understanding of injury patterns, availability of superior implant, the concept of surgical fixation and early postoperative mobilisation of joint have enormously improved the functional outcome of the patient [3,4]. There are several challenges which are encountered during the treatment of distal tibial fracture. These are high energy fractures, associated with extensively damaged soft tissues, poor vascularity, higher incidence of compound injuries, complications pertaining to skin following the surgery and comminution of the metaphysis and articular surface. Such daunting factors make anatomical reduction difficult. Around this area the fracture fixation is less satisfactory due to the quality of bone, and lack of soft tissue cover resulting in early loosening of the implant. Achieving rigid fixation in comminuted fractures is hard due to poor screw purchase, and hence the fixation is less optimal to allow weight bearing, or even early mobilisation. Proximity of the fracture to the ankle joint, displacement, comminution and injury to the soft tissue largely influence the selection of treatment modality [1]. Most fractures at this site need to be fixed because non-operative treatment results in loss of reduction and malunion. Diverse options are available for the treatment of these fractures which include Intramedullary Interlocking (IMIL) nail, conventional plating with dynamic compression plate, ankle spanning external fixator for soft tissue management and LCP using minimally invasive plate osteosynthesis [2-4].
Each of these techniques has its own advantages and demerits. IMIL nailing has been reported to have higher rate of malunion. This is because stable fixation is difficult to achieve due to inadequate distal locking screws. With conventional plate osteosynthesis wound infection, skin breakdown and delayed union or non-union are common complications which ultimately require secondary procedures like bone grafting. Likewise, osteomyelitis resulting from pin tract infection, pin loosening, malunion and non-union, is another potential complication of external fixators and hence it is not preferred as definitive fixation technique [5,6]. Recently emerged technique of closed reduction and MIPPO with LCP, provides alternative treatment option for distal tibia fracture. A mechanically stable osteosynthesis can be obtained with minimum dissection, time and surgical insult by this technique. This technique utilises indirect reduction and internal fixation with LCP bridging the fracture site [7-9]. LCP does not endanger periosteal blood supply; fracture haematoma remains undisturbed and provides biomechanically a stable construct. MIPPO provides firm fixation which helps in early mobilisation of the patients, minimum postoperative complications and greater rate of union [10-12].
With this background the current study was taken up to assess the functional and radiological outcomes of distal tibial fractures managed by MIPPO using LCP.
Materials and Methods
This was a cross-sectional study conducted on 25 patients with distal tibia fracture reported within the study duration i.e., between November 2015 to July 2019 after taking informed consent. Institutional Ethical Committee (IEC) approval was obtained (SDMIEC 0352). Patients more than 18 years with distal tibia and Gustilo and Anderson type I [4] fractures were included while Type II and Type III were excluded from the study. Patients with pathological fractures, fractures associated with compartment syndrome and ipsilateral fractures in proximal tibia or femur were excluded from the study. A detailed history was taken from patients and their attenders, followed by a clinical examination to evaluate the skin condition, wound and neurovascular status. Following that they were assessed radiologically with X-rays and blood investigations. The fractures were then classified according to Orthopaedic Trauma Association/AO foundation classification [4].
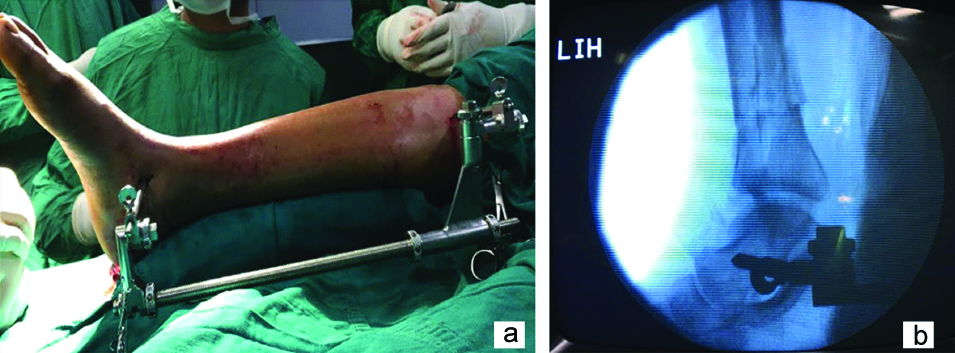
The patient was positioned supine on a radiolucent table with pneumatic tourniquet applied after the spinal/epidural anaesthesia. Medial and lateral malleolus were marked. Lateral malleoli or distal fibula fracture was fixed first which led to indirect reduction of the tibia as it helped to maintain the length and alignment. Persisting angular deformity in coronal or sagittal plane were corrected by using k-wire or Schanz pin as a joystick under image intensifier. In some cases, indirect reduction was done by the AO distractor which is a very easy way of getting the desired reduction [Table/Fig-1]. After correction of deformity, around 2-3 cm incision was made starting at level of the tip of the medial malleoli and extending proximally along medial surface of tibia. A subcutaneous tunnel was created along medial aspect of tibia by blunt dissection. The plate was placed on anteromedial aspect of distal tibia. A small incision was made at proximal end of plate proximal to the fracture site and plate was held in place with k-wires [Table/Fig-2]. The plate position was confirmed by image intensifier in anteroposterior and lateral views. The tip of the distal end of plate was at the level of tibial plafond and proximal end extended at least four screw holes beyond the proximal extent of fracture and fixed with locking screws of appropriate sizes as per the requirement of the fracture configuration [2].
a) Reduction of fracture indirectly with AO distractor; b) Fluroscopy image of fracture reduction after applying AO distractor.
Proximal and distal incision site with plate temporarily held with k wires.

Postoperatively, limb was kept elevated on Bohler Braun splint to prevent swelling with below knee slab immobilisation. Intravenous antibiotics and analgesics were given for two days postoperatively. On second postoperative day wound inspection and dressing was done. Postoperative X-rays were done in anteroposterior and lateral views. Static quadriceps exercise and toe movements were started from postoperative day 1. Postoperative day 5-7 walking with the aid of a walker without weight bearing on the operated limb was started, postoperative day 10-12 sutures were removed and patients were instructed to continue walking non-weight bearing with walker support. All patients were followed-up at 3 weeks, 6-8 weeks, 10-12 weeks, 6 months and 1 year with radiographs [Table/Fig-3,4 and 5]. At three weeks active ankle mobilisation was started and at 6-8 weeks partial weight bearing was allowed. At 10-12 weeks depending on the radiological and clinical evidence of fracture union patients were allowed full weight bearing on the operated limb. Functional evaluation was done on each follow-up and was looked for complications. Functional outcome was evaluated using AOFAS. Radiological outcome was evaluated using RUST score to assess union and misalignment [2-4]. The RUST score is a novel tool for the fracture assessment that was developed to standardise the radiological assessment of the fracture healing in tibia. The score takes into account the presence of callus and visibility of the fracture line in each cortex of the tibia (anterior, posterior, medial and lateral). The minimum score is 4 when there is no callus and the fracture line is visible on each cortex, whereas, maximum score is 12 when the callus is evident with invisible fracture line in all four cortices indicating complete healing [13].
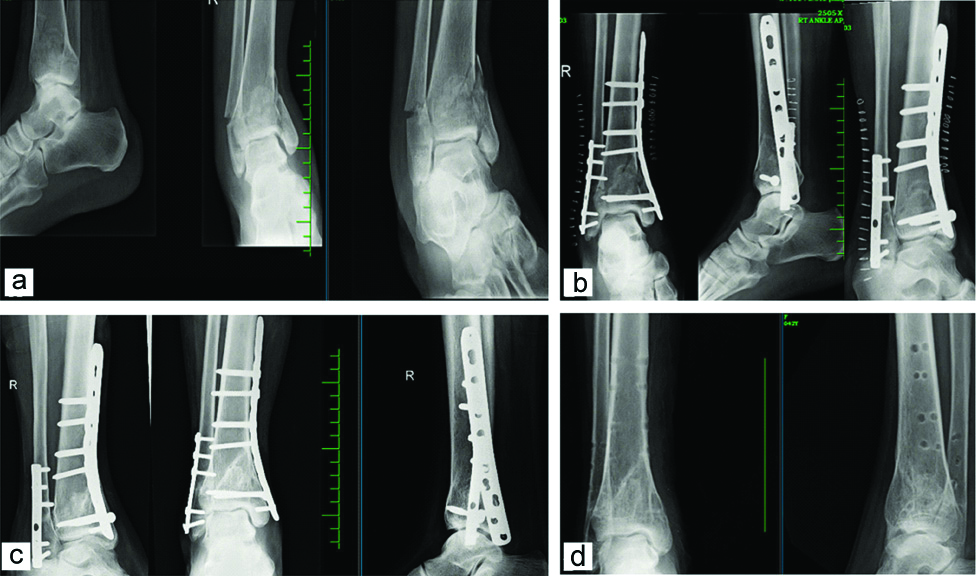
a) X-ray showing type B2 fracture with lateral malleoli fracture; b) Immediate postoperative X-ray; c) Follow-up x-ray at 6 months showing radiological union; d) implants removed at 2 years postoperatively.
a) X-rays showing type A3 fracture with lateral malleoli fracture; b) immediate postoperative X-rays; c) Follow-up X-rays at 6 months showing radiological union; d) Clinical pictures at 6 months.
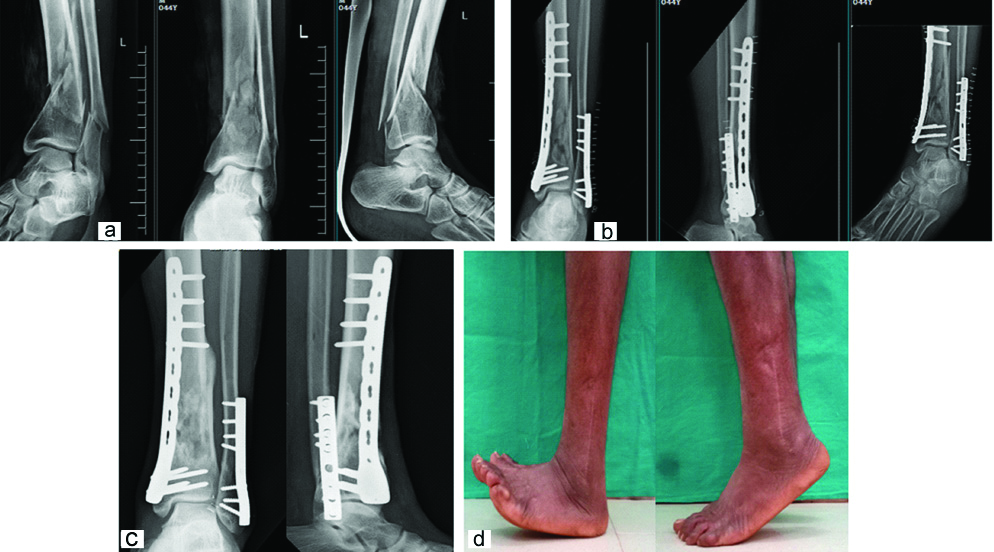
a) X-rays showing type A1 fracture with lateral malleoli fracture; b) Immediate postoperative X-rays; c) Follow-up X-rays at 12 months showing radiological union; d) Clinical pictures at 12 months.

Statistical Analysis
The data collected was subjected to statistical analysis using SPSS version 21. Suitable statistical methods (SD, Paired t-test, p-value) were employed for the analysis of the data. Paired t-test was used for comparison of AOFAS and RUST scores at three months, six months and 12 months of postoperative follow-up.
Results
Out of 25 patients analysed, 64% (16) of them were male and 36% (9) were female. Age distribution showed that 16% of the patients were of the age group between 30-39 and 40-49 each and the mean age was 51.83 (SD 11.28). Majority (60%) of the injuries occurred due to RTA which was most common mode of injury. AO type A3 (48%) was the most common fracture pattern and type B3 and C1 being least common with only one patient affected. Eighteen cases (72%) underwent fibula fixation [Table/Fig-6].
Observations of the demographic variables.
| Variable | Number of patients (%) (n=25) |
|---|
| Gender |
| Male | 16 (64%) |
| Female | 09 (36%) |
| Age groups (in years) |
| 30-39 | 04 (16%) |
| 40-49 | 04 (16%) |
| 50-59 | 10 (40%) |
| 60-65 | 07 (28%) |
| Mode of injury |
| RTA | 15 (60%) |
| Slip and fall | 9 (36%) |
| Fall of heavy object | 01 (4%) |
| Fracture pattern (AO types) |
| A1 | 03 (12%) |
| A3 | 12 (48%) |
| B2 | 04 (16%) |
| B3 | 01 (4%) |
| C1 | 01 (4%) |
| C2 | 04 (16%) |
| Fracture type |
| Open (Compound) | 03 (12%) |
| Closed (Simple) | 22 (88%) |
| Fixation of fibula |
| Yes | 18 (72%) |
| No | 04 (16%) |
| Not applicable | 03 (12%) |
RTA: Road traffic accident
The average fracture union time was 20 weeks. The mean RUST score at the three months was 7.83 and at one year were 11.58 showing increased union rates which was statistically significant [Table/Fig-7]. The mean AOFAS score at three months was 39.71 and at the one year it was 88.83 indicating positive functional outcome which was statistically significant [Table/Fig-8]. One patient had superficial infection, one patient reported plate impingement and one had implant failure.
Comparison of 3 months, 6 months, and 12 months time points with RUST scores by dependent t-test.
| Time points | Mean | Std. Dv. | Mean Diff. | SD Diff. | % of effect | Paired t | p-value |
|---|
| 3 months | 7.83 | 1.34 | -2.08 | 1.14 | -26.60 | -8.9614 | 0.0001* |
| 6 months | 9.92 | 1.02 |
| 3 months | 7.83 | 1.34 | -3.75 | 1.39 | -47.87 | -13.207 | 0.0001* |
| 12 months | 11.58 | 0.72 |
| 6 months | 9.92 | 1.02 | -1.67 | 0.76 | -16.81 | -10.723 | 0.0001* |
| 12 months | 11.58 | 0.72 |
*p<0.05
Comparison of 3 months, 6 months and 12 months time points with AOFAS scores by dependent t-test.
| Time points | Mean | Std.Dv. | Mean Diff. | SD Diff. | % of effect | Paired t | p-value |
|---|
| 3 months | 39.71 | 8.21 | -26.42 | 8.21 | -66.53 | -15.7 | 0.0001* |
| 6 months | 66.13 | 6.89 |
| 3 months | 39.71 | 8.21 | -49.13 | 6.21 | -123.71 | -38.7 | 0.0001* |
| 12 months | 88.83 | 5.65 |
| 6 months | 66.13 | 6.89 | -22.71 | 5.81 | -34.34 | -19.1 | 0.0001* |
| 12 months | 88.83 | 5.65 |
*p<0.05
Discussion
Distal tibial fractures are renowned therapeutic challenges for orthopaedic traumatologists. Although conservative management of these fractures has been described, it has been largely replaced by operative techniques. Reudi T et al., achieved 74% good results following open reduction for distal tibia fractures thus changing the entire outlook of distal tibia fractures management in the early 20th century [14]. However, it was later recognised that all their cases were of low velocity injuries and similar results couldn’t be obtained in high velocity injuries. Therefore, procedures like MIPPO which protects the soft tissue around the distal tibia evolved.
The main aim of the operative procedure is to achieve optimal anatomical alignment and stability with minimal devascularisation of both bone and soft tissue as well as lesser treatment complications. In percutaneous plating, locked plate designs act as fixed angle devices, having axial and angular stability at the screw- plate interface as against interlocking nail which relies on the frictional force between the plate and bone. Thus, preserving the periosteal blood supply around the fracture site [15,16]. The biological fixation techniques are currently the procedures of choice for distal tibia fractures. Minimally invasive percutaneous plating, a well established procedure now, reduces the iatrogenic soft tissue injury and lessens the damage to vascularity of the bone. It is based on principles of limited exposure, indirect reduction (bridging osteosynthesis) and a limited contact between bone and implant [17,18]. The age of the patients ranged from 30-65 years with mean age of 51.83 years (SD 11.28). Range of 50-59 years had highest patients (40%). In present study, seven patients were above the age of 60 years with three patients having controlled diabetes. All were treated with MIPPO technique using LCP and none of them had any wound complications. Guo JJ et al., on the other hand included patients with ages 23-70 years with good number of elderly patients aged >60 years in his study. Most of those elderly patients had associated comorbidities such as diabetes, osteoporosis and vasculitis. In these patients, they stated that fixation around the ankle as per their co-morbidities and skin condition is a must while elderly with no co-morbidities could be treated with same principles as that of the young patients [19].
Of the 25 patients in this study, 16 (64%) were males and 9 (36%) were females. This could be attributed to the fact that more outdoor activities and heavier labour is undertaken by males as compared to females in this conservative regional set up. This was in concordant with the findings of Collinge C et al., and Grosse A et al., [3,20]. The most common cause for these fractures was RTA followed by slip and fall. Present study results were comparable to their studies which also showed that RTA is the most common mode of injury. Present study had a reduced infection rate which could be because of the fact that there were only 12% open injuries. Sixty percent of cases in present study were extraarticular, 20% partial intraarticular and 20% intraarticular fractures. Functional outcome of present study was comparable to findings reported by Vallier HA et al., However, they have not included type C2 fractures [21]. Present study had an average fracture union time of 20 weeks which was similar to other studies using locked compression plating in which the average time for union was 16-28 weeks [3,22]. The union rates with MIPPO were reported to be 100% in a study by Helfet DL et al., [23] and was found to be comparable with present study. Union rates were 90% and 97% in study by Hazarika S et al., and Zelle BA et al., [22,24]. High union rate and increased need for secondary surgery were reported with open reduction and internal fixation, whereas MIPPO showed better results.
Function assessment was done based on AOFAS scoring system at regular intervals and for present study mean AOFAS was 88.83 which was comparable with other studies. Mudgal A et al., reported a mean AOFAS score of 90 [25]. Gao H et al., studied poly-axial locking system in management of 32 cases of distal tibia fractures with short metaphyseal fragments. It showed a mean AOFAS of 87.3 offering more fixation versatility and also a smaller number of cases with palpable implants [26]. Ozkaya U and Parmaksizoglu AS in their study treated distal third tibia fractures with LCP using MIPPO technique and found good results (mean AOFAS = 81) [27]. Dhakar A et al., had 94% excellent to good results with this technique [7]. The RUST score is a novel tool for the fracture assessment that was developed to standardise the radiological assessment of the fracture healing in tibia. In present study, the mean RUST score at the end of one year follow-up was 11.58.
Tibial fractures are often associated with fibular fractures which affect the treatment modality and results. The decision regarding its fixation varies amongst surgeons. According to Francois J et al., it is important to restore the original length and rotation of the fibula. Majority of the people believe that fibular fractures are associated ankle instability and hence must be stabilised otherwise they yield poor functional outcome [28]. Shrestha D et al., in their study did not fix fibula routinely unless it involved syndesmosis [29]. Numerous studies have hypothesised that fibula fixation may facilitate anatomic reduction of the tibia by reducing the strain [28,30]. In present study, out of 25 cases, 22 were associated with fibular fractures. In 18 (72%) cases fibular fractures were fixed. These cases with fibula fixation had isolated mean AOFAS score of 89. In rest 7 (28%) cases fibular fixation was not done and their isolated mean AOFAS score was 86. It appears in both the groups functional results were nearly same which was in comparison to a study done by Vasanad GH et al., [31]. However, statistical comparison was not done because standard protocol was not defined for fibula fixation. As per surgeon’s preference fibula was fixed with either semi-tubular plate or with pre-contoured fibular locking plate.
The infection rate MIPPO technique was found to be 15% in a study by Lau TW et al., 14.6% according to Guo JJ et al., and 14.3% as per Borg T et al. Guo JJ et al., reported a wound complication rate of 14.6%. This was attributed to the precarious blood supply of medial aspect of distal tibia and also the senile atrophy of the skin making it more prone for infection [19,32,33]. In a study by Mudgal A et al., wound complication of about 14.8% superficial infection and 4.76% deep infection was found. They postulated that initial high velocity injury could lead to soft tissue injury at the fracture site which could later complicate the postsurgical wound [25]. In present study however infection rate was much lower (4%) which was well managed with antibiotics and regular dressings. Low infection rate could be because of a greater number of closed fractures in present study and lower number of compound fractures. Implant failure was reported to be 2.4% by Bahari S et al., and 5% by Hazarika S et al., [10,22]. In present study, we had one implant failure accounting for 4%. This was due to early uncontrolled weight bearing. It was managed with cast immobilisation and later it went on to unite. Bedi A et al., and Gun IM et al., treated distal tibial fractures with intramedullary nail and found that failure to control distal fragment led to significant misalignment and deformity. On the other hand, none of patients in present study had varus or valgus malalignments [1,34].
Every technique comes with advantages as well as disadvantages. One drawback of MIPPO is that does not allow direct visualisation of the fracture site and therefore the surgeon solely depends upon intraoperative c-arm pictures to confirm the reduction, plate placement, and locking screw position thereby increasing exposure to radiation. However, data analysis of the present study helps in understanding that fixation of distal tibia fracture with LCP using MIPPO technique gives good results with minimal complications.
Limitation(s)
Limitations of present study was smaller sample size, classification of the soft tissue status preoperatively was not done, subjective method for fibular fixation and individual choice of implant was not done.
Conclusion(s)
The MIPPO technique is a simple, rapid, reliable, and straight forward fixation approach for comminuted distal tibia fractures involving mainly the metaphyseal area preserving osseous vascularity and fracture haematoma and thus providing a more natural fracture healing. Good functional outcomes (mean AOFAS 88.83) obtained in present study further emphasise the effectiveness of minimally invasive plate osteosynthesis.
RTA: Road traffic accident
*p<0.05
*p<0.05