Stuck in the Middle! A Case of Repeated Foreign Body Impaction in Oesophagus
P Kiranmayi1, Y Radha Krishna2
1 Assistant Professor, Department of Physiology, GIMSR, Visakhapatnam, Andhra Pradesh, India.
2 Associate Professor, Department of Gastroenterology, GIMSR, Andhra Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Y Radha Krishna, GIMSR, Visakhapatnam, Andhra Pradesh, India.
E-mail: radhayellapu@gmail.com
Oesophageal foreign body impaction is usually seen in children as well as in adults with varying aetiologies. It is an emergency situation requiring proper evaluation and prompt treatment because of the possible complications like oesophageal perforation, mediastinitis and aspiration. Here, the report presented an interesting case of repeated foreign body impaction in the lower oesophagus of an elderly male. A 76-year-old male patient came to the Emergency Department in a Tertiary Care Center with chest pain and obstruction in the passage of food which had begun several hours prior to visit after having a chicken meal. The patient had presented with similar complaints in the past on three different occasions. The clinical examination was normal. As a part of the treatment, urgent upper gastrointestinal endoscopy was performed by using olympus flexible video endoscope under general anaesthesia, which showed meal impaction in distal oesophagus. The impaction was removed successfully with combination of rat tooth forceps and endoscopic snare. Later on after successful retrieval during his subsequent visit in view of his repeated foreign body impaction, further evaluations including High-Resolution Manometry (HRM) were performed which revealed multiple oesophageal spasms during the passage of food, with premature peristalasis and thereby, it was diagnosed as Diffuse Oesophageal Spasm (DES). The patient was given nitrates and kept on calcium channel blockers for long term medication. DES is an uncommon cause of dysphagia, for which oesophageal manometry is the gold standard procedure. Presence of synchronous contractions in a minimum of twenty for one hundredth of wet swallows (constituting 20%), alternating with normal motility patterns is a diagnostic criteria for DES on manometry. HRM has been a significant improvement in the accuracy of describing the various motility disorders of oesophagus.
Chest pain, Dysphagia, Manometry, Oesophageal spasm
Case Report
A 76-year-old male presented with dysphagia to both solids and liquids. The patient presented to the emergency services late in the afternoon in July 2018 with difficulty in swallowing for both solids and liquids along with chest pain. Chest pain was sudden in onset, squeezing type of pain without any radiation, and was aggravated by swallowing. The patient was an edentulous, smoker and an alcoholic for thirty years. He was nondiabetic and normotensive. His vitals and clinical examination were normal.
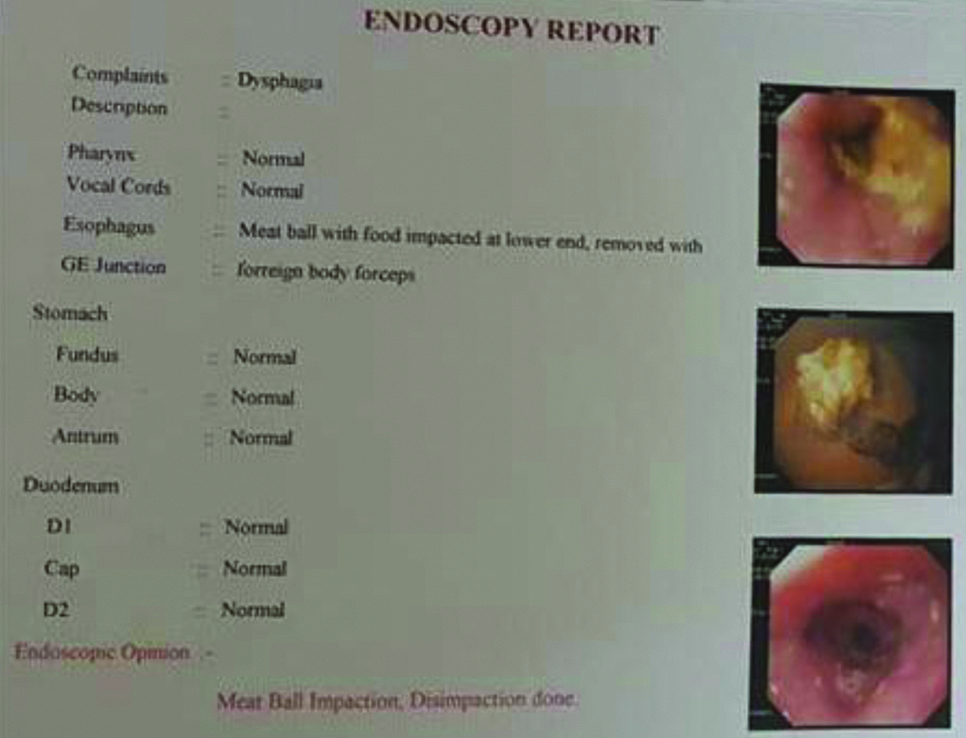
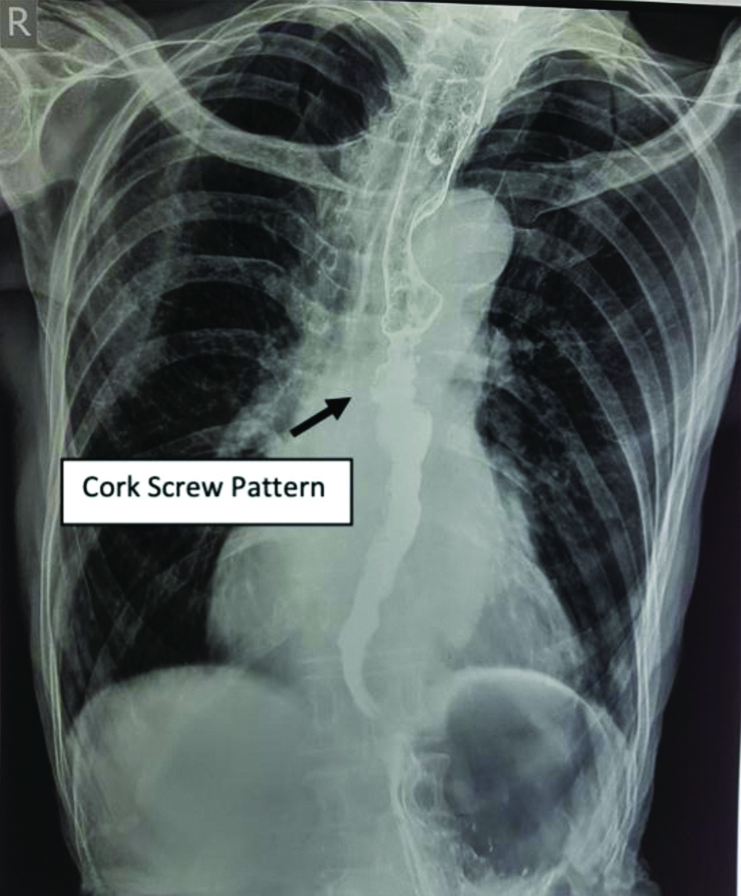
The patient had a past history of similar type of foreign body impaction on three different occasions between Feb 2014 and July 2018. He had meat ball impactions in February 2014, June 2014, February 2017 and during the current visit July 2018. Emergency endoscopy was performed in Feb 2017 which showed that the patient had no other significant endoscopic findings like polyp, growth or features of achalasia cardia [Table/Fig-1]. The patient was given Barium meal and anterio posterior chest x-ray was taken during the current visit which revealed cork screw pattern, suggestive of increased pressurisation in oesophagus, which is indicative of cork screw oesophagus [Table/Fig-2].
Patient Upper GI Endoscopy report showing Meal Impaction (Feb 2017).
Patient’s barium swallow report showing corkscrew pattern.
Treatment
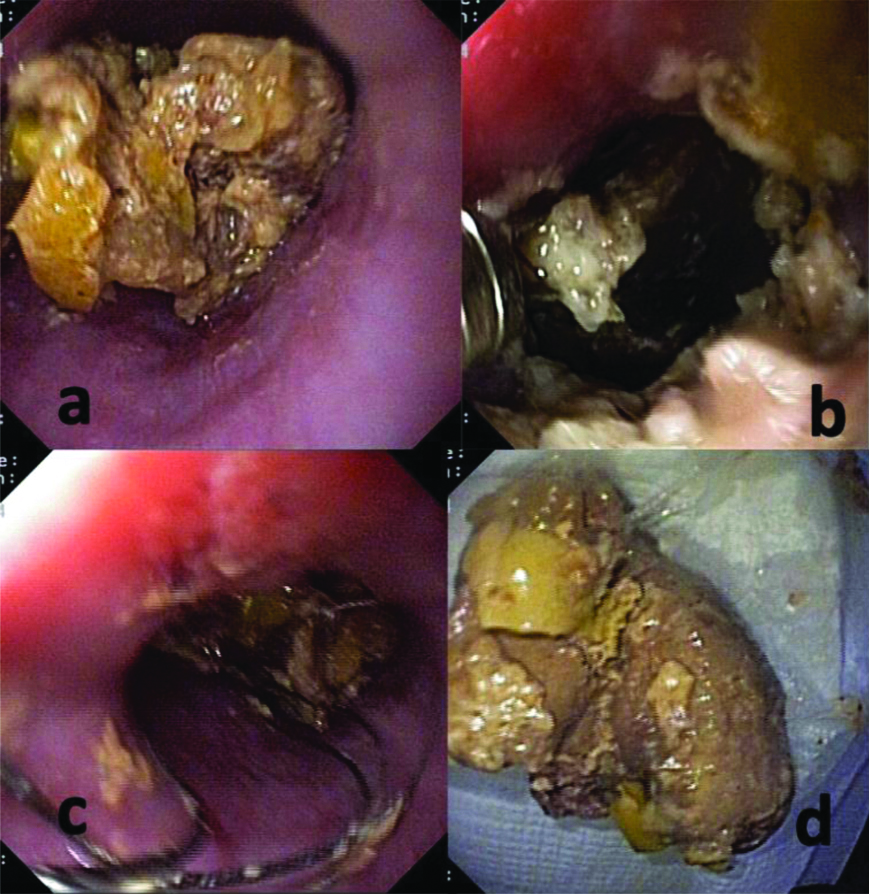
As a part of the treatment, urgent upper gastrointestinal endoscopy was performed by using olympus flexible video endoscope under general anaesthesia showed meal impaction in distal oesophagus which was removed successfully with combination of rat tooth forceps and endoscopic snare [Table/Fig-3]. Informed consent was obtained from the subject for the images used in the case report.
Patient’ Upper GI Endoscopy pictures showing: a) Meat ball impaction; b) Rat tooth forceps application; c) Foreign body snare removal application; d) Extracted meat bolus (July 2018).
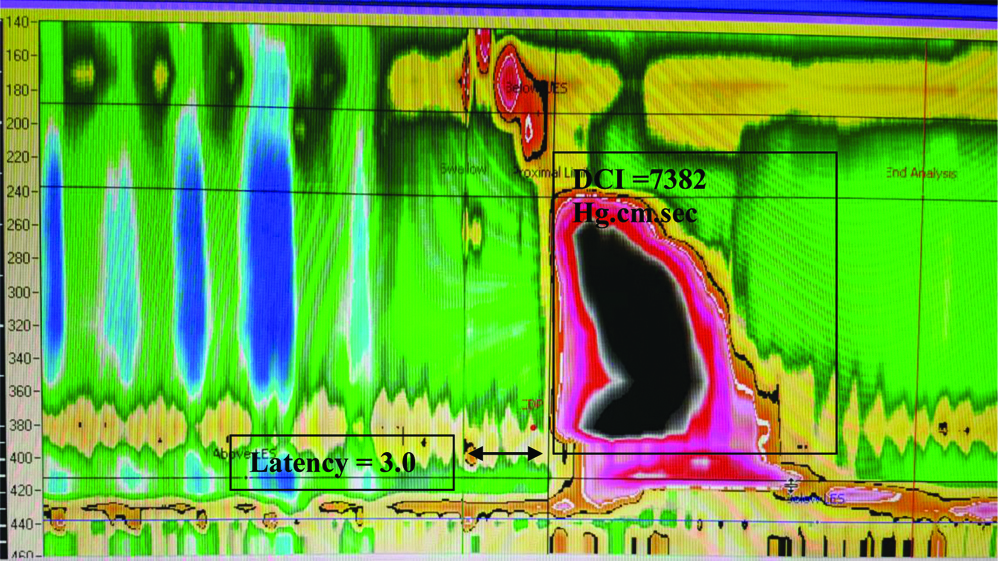
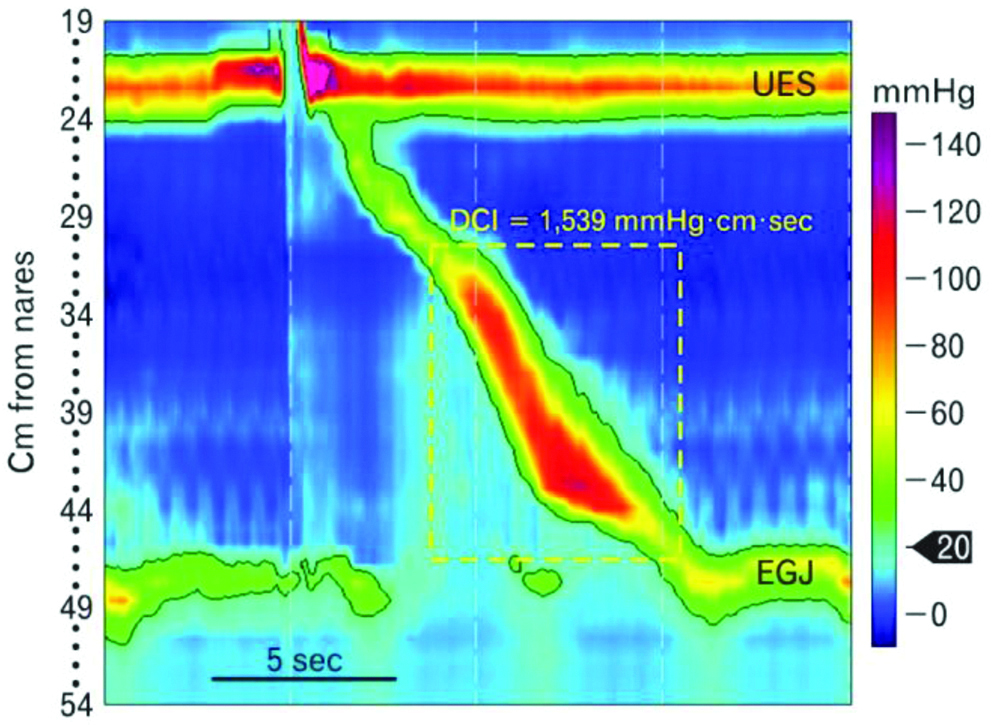
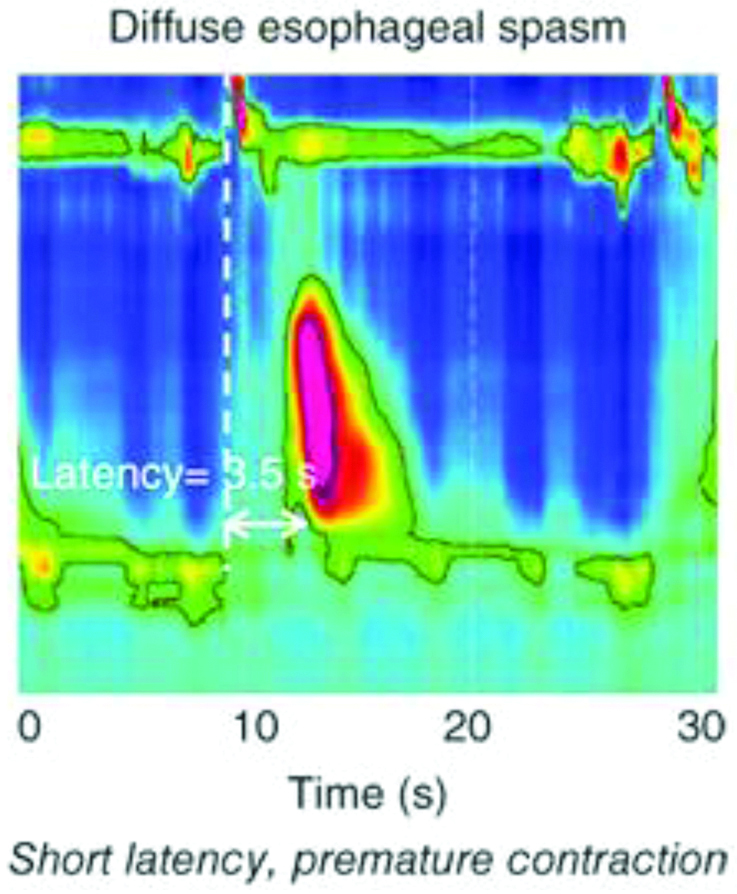
The oesophageal HRM was performed which revealed multiple oesophageal spasms during the passage of food with premature peristalsis and thereby, it was diagnosed as DES [Table/Fig-4].
Patients high resolution Oesophageal Manometry Report showing Diffuse Oesophageal Spasm (DES).
Treatment of DES remains challenging. The patient was advised to take calcium channel blockers and nitrates (Nifedipine 5 mg three times a day). Hellers Myotomy and Peroral Endoscopic Myotomy (POEM) are alternative treatment modalities in refractory cases. In view of repeated problems, the patient was advised to undergo POEM. On last follow-up in December 2019, the patient had no recurrence of previous complaints and was continuing calcium channel blockers (Nifedipine 5 mg three times a day). The patient was reluctant for aggressive therapy (POEM or surgery). The patient also changed his dietary pattern and was consuming predominantly mashed foods/semi soft diet.
Discussion
In general, majority of cases oesophageal foreign bodies can be resolved without any intervention and so they go unnoticed. Dysphagia is a common clinical problem, for which motor disorders like Achalasia Cardia and DES are uncommon aetiologies [1]. Diagnosis of these disorders is only possible with detailed evaluation. Here, an unusual case of repeated foreign body impaction due to DES was reported. Spasm of the oesophagus is common explanation for unexplained chest pain and dysphagia which can be confirmed by dedicated motility studies like Manometry [2]. Recently, HRM with graphical displays [Table/Fig-5,6] has yielded new views and insights in studying the musculature and motor functions of oesophagus [3,4].
Normal oesophageal manometry with a swallow.
UES: Upper oesophageal sphincter; EGJ: Oesophagogastric junction
High resolution oesophageal manometry with DES.
The simultaneous relaxation of upper and lower oesophageal sphincters with a swallow can be seen. Here, Heberts water-perfusion oesophageal manometry of 16 channels was used [1]. This procedure is done in outpatient setting without any sedation. HRM helps to differentiate true muscular spasm from speedy elevation of the intra-bolus pressure and also to diagnose focal dysmotility or obstruction [4].
The report also did multiple rapid swallow test in this case, it involves administering five swallows of 2-5 mL liquid at 2-3 second intervals, according to the standard HRM protocol. The physiologic responses of profound deglutitive inhibition of the LES, deglutitive inhibition of oesophageal body contractions, and then, after rapid swallows, the augmented contractile response follows in normal oesophagus [5]. In this case, relaxation in LES during rapid swallow test was observed, there by, ruling out achalasia cardia but instead of deglutitive inhibition of oesophageal body contractions, there were intense contractions suggestive of DES [6]. Severe Gastroesophageal reflux disease also causes spasms in oesophagus without rise in Distal Contractile Integral (DCI), which can be diagnosed by 24 hour pH metry [7]. Other motility disorders similar to DES are nutcracker or jackhammer or hyper contractile oesophagus [7].
The Chicago classification proposed that the defining criteria for DES using HRM should be the presence of at least two premature contractions (distal latency <4.5 sec) in context of normal oesophagogastric junction relaxation [Table/Fig-5] [6]. Distal latency is a parameter which measures peristaltic velocity from the beginning of the swallow to the end. It helps in differentiating the normal peristaltic wave from premature peristaltic contractions. Here, another parameter in HRM was also used for diagnosing DES called DCI, which is the measure of pressure in distal part of oesophagus during swallow, in which the normal value ranges between 500 to 3000 mm [8]. For DES, the DCI value ranges between 3000-8000 mm and more than 8000 mm Hg comes under hypercontractile oesophagus. Thus, HRM helps in distinguishing DES from hypercontractile oesophagus where DCI would be more than 8000 mm Hg [9,10]. DES is defined manometrically by premature contractions in a minimum of 20% of all swallows [11]. Radiographically in x-ray, diffuse oesophageal spasm is characterised by a “corkscrew pattern” with multiple coincidental contractions that obliterate the lumen [12,13]. Routine upper gastrointestinal endoscopy cannot diagnose these disorders. Barium swallow and HRM are more sensitive in diagnosing these motor disorders [14]. The aetiology of DES links nitric oxide deficiency as one of the culprits resulting in spasmodic oesophageal contractions due to disordered neural inhibition [15].
Conclusion(s)
In a patient with repeated dysphagia, the authors have to evaluate thoroughly, and the motility disorders should be suspected. These disorders can’t be diagnosed by routine investigations like endoscopy. They need dedicated tests like barium swallow and manometry. Recent technology of high-resolution manometry helps us better characterise these motility disorders and guide to appropriate treatment.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Apr 22, 2020
Manual Googling: Sep 18, 2020
iThenticate Software: Oct 24, 2020 (10%)
[1]. Pandolfino JE, Kahrilas PJ, New technologies in the gastrointestinal clinic and research: Impedance and high-resolution manometryWorld J Gastroenterol 2009 15(2):131-38.10.3748/wjg.15.13119132761 [Google Scholar] [CrossRef] [PubMed]
[2]. Per P, Rebecca A, Magni G, Alex d Leon, Stefan L, Detailed measurements of oesophageal pressure during mechanical ventilation with an advanced high-resolution manometry catheterCrit Care 2019 23(1):21710.1186/s13054-019-2484-831196203 [Google Scholar] [CrossRef] [PubMed]
[3]. Grubel C, Borovicka J, Schwizer W, Fox M, Hebbard G, Diffuse esophageal spasmAm J Gastroenterol 2008 103(2):450-57.10.1111/j.1572-0241.2007.01632.x18005367 [Google Scholar] [CrossRef] [PubMed]
[4]. Soudagar Sd, Sayuk GS, Prakash GC, Learners favour high resolution oesophageal manometry with better diagnostic accuracy over conventional line tracingsGut 2012 61(6):798-803.10.1136/gutjnl-2011-30114521997554 [Google Scholar] [CrossRef] [PubMed]
[5]. Boland K, Abdul-Hussein M, Tutuian R, Castell DO, Characteristics of consecutive esophageal motility diagnoses after a decade of changeJ Clin Gastroenterol 2016 50(4):301-06.10.1097/MCG.000000000000040226422715 [Google Scholar] [CrossRef] [PubMed]
[6]. Bredenoord AJ, Fox M, Kahrilas PJ, Pandolfino E John, Werner S, Smout AJPM, Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topographyNeurogastroenterol Motil 2012 24(1):57-65.10.1111/j.1365-2982.2011.01834.x22248109 [Google Scholar] [CrossRef] [PubMed]
[7]. Trudgill NJ, Daniel S, Rami S, Mark F, Kumar B, McCord M, British Society of Gastroenterology guideline for oesophageal manometry and oesophageal reflux monitoringGut 2019 68(10):1731-50.10.1136/gutjnl-2018-31811531366456 [Google Scholar] [CrossRef] [PubMed]
[8]. Prakash GC, Kahrilas PJ, Edoardo S, Frank Z, Mion F, Smout AJPM, Vaezi M, Modern diagnosis of GERD: The Lyon ConsensusGut 2018 67(7):1351-62.10.1136/gutjnl-2017-31472229437910 [Google Scholar] [CrossRef] [PubMed]
[9]. Konturek T, Lembo A, Spasm, nuckcracker, and IEM: Real or manometry findings?J Clin Gastroenterol 2008 42(5):647-51.10.1097/MCG.0b013e3181646d1918364582 [Google Scholar] [CrossRef] [PubMed]
[10]. Pandolfino JE, Ghosh SK, Rice J, Clarke JO, Kwiatek MA, Kahrilas PJ, Classifying esophageal motility by pressure topography characteristics: A study of 400 patients and 75 controlsAm J Gastroenterol 2008 103(1):27-37.10.1111/j.1572-0241.2007.01532.x17900331 [Google Scholar] [CrossRef] [PubMed]
[11]. Fox MR, Bredenoord AJ, Oesophageal high-resolution manometry: Moving form research and into clinical practiceGut 2008 57(3):405-23.10.1136/gut.2007.12799317895358 [Google Scholar] [CrossRef] [PubMed]
[12]. Lacy BE, Weiser K, Esophageal motility disorders: Medical therapyJ Clin Gastroenterol 2008 42(5):652-58.10.1097/MCG.0b013e31815bd22318364589 [Google Scholar] [CrossRef] [PubMed]
[13]. Sifrim D, Fornari F, Non-achalasic motor disorders of the esophagusBest Pract Res Clin Gastroenterol 2007 21(4):575-93.10.1016/j.bpg.2007.03.00917643902 [Google Scholar] [CrossRef] [PubMed]
[14]. Dogan I, Mittal RK, Esophageal motor disorders: Recent advancesCurr Opin Gastroenterol 2006 22(4):417-22.10.1097/01.mog.0000231818.64138.8a16760760 [Google Scholar] [CrossRef] [PubMed]
[15]. Triadafilopoulos G, Tsang HP, Segall GM, Hot water swallows improve symptoms and accelerate esophageal clearance in esophageal motility disordersJ Clin Gastroenterol 1998 26(4):239-44.10.1097/00004836-199806000-000039649001 [Google Scholar] [CrossRef] [PubMed]