Case Report
A 24-year-old male reported to Department of Prosthodontics and Crown & Bridge, Faculty of Dentistry, Jamia Millia Islamia, New Delhi missing lower front teeth, causing him mental despair due to poor aesthetics. He presented with the history of Road Traffic Accident (RTA) 1-1.5 years ago, which led to multiple injuries and loss of the concerned teeth. Following the RTA, the patient was unconscious and under intensive care for approximately 1.5 months. The patient was a non-smoker and had no other associated relevant medical history or any associated maxillofacial fractures. At the time of reporting to us, the patient was using removable partial denture (RPD) at a different dental setup but was dissatisfied with aesthetics and comfort. The patient was subjected to clinical and radiographic evaluations to formulate an appropriate treatment plan. Clinical evaluation showed missing mandibular incisors along with canine and first premolar on right side. The patient did not have his previous medical records thus, nothing could be commented about the presence of maxillofacial fractures. However, clinical examination did not elucidate presence of step deformity. Patient gave no previous history of missing teeth prior to RTA. Thus, nothing conclusively could be said about it. It is possible that the teeth lost can be due to orotracheal intubation that the patient was subjected to during treatment of RTA associated injuries. Reduced labial bone width of 2 to 3 mm with high labial frenum attachment (gingival attachment) was recorded in central incisor region [Table/Fig-1]. Bone width was estimated by making measurements in the recorded diagnostic casts. The cast was cut in cross-section and measurements were made by giving due consideration to overlying soft tissue thickness. At this clinical examination, sufficient vestibular depth with 3-4 mm of attached gingiva was present in the edentulous area corresponding to right mandibular central incisor to right mandibular first premolar.
a) Preoperative clinical, intraoral findings; b) Orthopantogram findings, c) Preoperative mandibular occlusal view.

Orthopantogram revealed impacted mandibular right first premolar with presence of insufficient vertical bone measurements in mandibular right central incisor to canine region (3.4 to 3.8 mm with respect to root apex of adjacent teeth) [Table/Fig-1]. It was speculated that the impacted mandibular right first premolar could have been due to the impact of the experienced RTA. Measurements were done by superimposing the radiograph on a grid. Cone Beam Computed Tomography (CBCT) was originally planned to make accurate measurements but was not done due to patient’s inhibition for the recording procedure. Owing to these attributes, the case was discussed with an oral surgeon and periodontist associated with the institute, for a multidisciplinary approach. Planned treatment consisted of transalveolar removal of impacted tooth, deficit alveolar ridge augmentation followed by implant-based rehabilitation, labial frenectomy and vestibuloplasty (if required as the initial clinical examination presented adequate dimensions of 4 to 6 mm). The patient was informed about the treatment in detail and written informed consent was obtained.
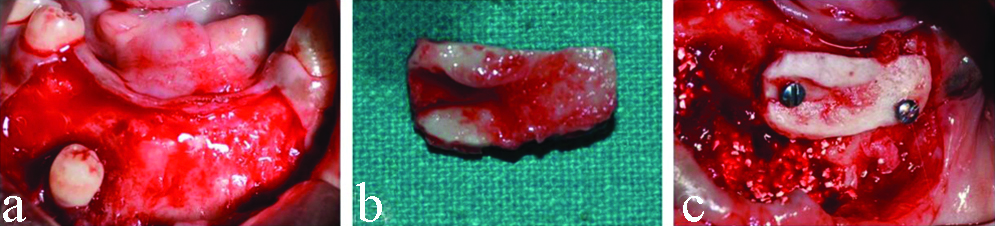
In first surgical intervention, impacted tooth was removed along with edentulous ridge augmentation. Surgery was conducted under local anaesthesia using 2% lidocaine with 1:80,000 adrenaline (Lignox® 2% A, Indoco Remedies Ltd., Gujarat, India). Amoxicillin 500 mg was given orally one hour before the procedure. First incision was made on edentulous alveolar crest, reflecting a mucoperiosteal flap till the level of impacted tooth to facilitate its extraction [Table/Fig-2a]. Vertical releasing incision was also given to avoid prospective complications of wound dehiscence. Hydroxyapatite crystals were densely packed in the extraction socket to facilitate bone formation. Bone dimensions of the residual ridge in the anterior region were measured directly using william’s graduated probe to confirm the estimations made on the radiograph. Simultaneously, symphyseal autogenous bone block (dimensions of 29*13*4 mm) was harvested for ridge augmentation and donor site, present in the symphysis region, was filled with hydroxyapatite granules (Ostofom Bone Graft, Sark Healthcare Pvt., Ltd.,). While obtaining the graft care was taken to keep a minimum distance of 5 mm from the inferior border of mandible, 5 mm from the mental foramen and 5 mm from apices of the present teeth in the region. This was ensured by using bone wax as a surgical template. Bone wax was softened and adapted over the ridge area that required augmentation. Following its adaptation, the bone wax was hardened by placing it in cold water to be used as a template. 1 mm diameter round rotary bur (SS White Dental, USA) was used in a straight hand piece under copious irrigation to obtain the graft. The recipient site was prepared by decorticating the recipient surface and making a few bleeding points at the site. Inducing bleeding also ensured bone graft uptake at the site. The graft was then contoured and anchored to recipient site using two titanium screws of 1.5×6 mm in dimensions (Tita. Mini Bone Screws, Ortho Max Mfg. Co. Pvt., Ltd.,) [Table/Fig-2b,c]. Any voids present between the graft bone and donor site were filled using the bone chips obtained by decorticating of the recipient bone surface and hydroxyapatite crystals. No additional membrane for graft stabilisation was placed. The flap was re-approximated and sutured by interrupted sutures, using nonresorbable 3-0 silk suture (Mersilk, Ethicon US). Patient was prescribed an antibiotic (Augmentin, GlaxoSmithKline) and an analgesic (Ibuprofen) for five days postoperatively. Patient was recalled after five days for suture removal and to check for inflammation and any associated discomfort. Follow-up visits were scheduled every two weeks for the first month and once a month thereafter for clinical and radiographic evaluation of soft tissue healing and graft integration of the used autologous onlay graft.
a) Raising the surgical flap to expose impacted mandibular first premolar; b) Harvested bone graft from symphysis; c) Fixing of the obtained bone graft at the recipient site with titanium screws.
Five months following ridge augmentation, a second surgery was performed for implant placement in grafted site. Site re-entry was done following incision line of first surgery. Fixation screws were removed after assessing block stability. Four implants (Osstem Implant System; two of 11.5×3.5 mm, one each of 11.5×4.0 mm and 11.5×4.5 mm) were placed in planned positions using manufacturer specified drilling protocol [Table/Fig-3]. The planned positions of the four dental implants in the mandible were: left central incisor region, right lateral incisor region, right canine region and right first premolar region. All drills and implant measurement equipment used were of Osstem Implant System. All drillings were performed at insertion torque between 25-35N. Initially, a punch cut was made using pilot drill at 1,500 rpm to determine the fixture position. This was followed by use of 2.0 mm diameter twist drill at a speed to 1,500 rpm which was extended till the desired length of the planned implant (right central and lateral incisor, canine and first premolar regions). Achieved depth was confirmed using a depth gauge. Subsequently, larger diameter drills were used at speeds of 800 rpm to 1,200 rpm till the desired diameter was achieved. All drillings were done under copious irrigation. Orientation of two adjacent implant holes was confirmed using parallel pins before proceeding with implant insertion. Provisional prosthesis was given three months after implant placement to improve patient’s aesthetics [Table/Fig-3]. Postsurgically the patient was asked not to consume hard and hot food, not to use straw for consuming liquid, to avoid forceful spitting by creating negative suction pressure, not to evert the lip to see the surgical site in the mirror, not to poke the surgical area with tongue or any other aid such as toothpick and not to brush in the area. Patient was asked to do ice pack application in the area and switch to warm saline rinses after 24 hours.
a) Dental implants in place; b) Temporary prosthesis in place with high frenal attachment (gingival attachment) and low vestibular depth, c) Orthopantogram showing dental implants in place.

As anticipated during initial planning, patients’ high frenal attachment caused tension over gingival margin around implants [Table/Fig-3] which was clinically confirmed by performing tension test. At clinical examination done one month after implant placement and temporary prosthesis delivery, non adherent gingival tissue was observed around dental implant placed in left lateral incisor position with complete absence of attached gingiva (0 mm). This was corrected using diode laser assisted periodontal surgery. Laser was used in pulsed mode (DenLase 940 nm wavelength, 3.0W power output) with intermittent laser tip application, directed at 10°-15° to the tissue.
Periosteum strip was removed at the level of mucogingival junction, causing periosteal fenestration and exposing bone, thus achieving the desired vestibular depth. The operated site was covered with eugenol-free periodontal dressing (Coe-PakTM, GC America Inc.). Patient was educated concerning postoperative precautions which were similar to those given after implant placement surgery and was advised to take previously prescribed analgesic on a need basis but not to take more than two tablets per day at less than 12 hours gap. Additionally, 0.12% chlorhexidine mouth wash was prescribed to aid in plaque control. No significant bleeding was encountered during or immediately after the procedure. As previously mentioned, this periodontal procedure was done one month after implant placement and delivery of temporary prosthesis. Although the patient did not present with any complaint, the conducted clinical assessment presented excessive tension at the implant margin which necessitated the need for sulcus deepening. The tension on implants was assessed by lightly pulling the lower lip in an outward direction. This led to movement of the marginal gingival tissue in relation to the dental implant placed in right lateral incisor position. This indicated that the gingival tissue was not adherent to the underlying bone which necessitated undertaking of periodontal surgery to improve prognosis of the dental implant. Literature has shown that use of laser assisted periodontal surgery helps in avoiding relapse [1]. Thus, by their previous experience and available literature, the periodontist did not feel the need for using graft material.
Clinical examination conducted one month following periodontal surgery showed satisfactory labial vestibule healing without complications. After six months of dental implant placement, the implant was clinically and radiographically assessed for mobility and probing depths. Implant mobility was clinically tested by surgeon’s perception and absence of radiolucency between the implant surface and bone on the recorded radiograph. All implants had universal probing depths of 1-1.5 mm on all surfaces. Following assessment, a definitive porcelain-fused-to-metal prosthesis was cemented [Table/Fig-4]. At this time, 3-4 mm of nonmovable keratinised tissue in the periodontally operated area was recorded, thereby leading to successful vestibular deepening and frenectomy procedures. As is evident in the radiograph, the root of mandibular left canine was distally inclined. Thus, the implant could not be placed any more distally than its current position else it would have jeopardised the functionality of the present canine. However, the space present for crown placement was adequate to replace all the missing permanent teeth. A bridge could have been given using present canine as support, but the patient was not willing for intentional sacrifice of natural tooth structure. Preoperative and postoperative extraoral pictures show the outcome of the treatment [Table/Fig-5].
a) Increased vestibular depth following laser assisted periodontal surgery recorded 1 month after periodontal intervention; b) Final prosthesis in place (mandibular occlusion); c) Final occlusion with prosthesis (frontal view).

a) Preoperative frontal view of the patient; b) Postoperative frontal view of the patient.

Discussion
The following case report is a multidisciplinary approach for rehabilitating posttraumatic loss of permanent mandibular anterior teeth [8], using dental implants in resorbed alveolar ridge which has been presented in accordance with CARE guidelines [2].
Traumatic Dental Injuries (TDI) ranges from small defects like enamel infraction, crown fractures to severe dento-alveolar fractures, with resultant loss of tooth and supporting structures. This leaves patients with compromised aesthetics and functioning. Loss of permanent anterior teeth is a common sequela following facial injuries like falls, road accidents, contact sports injuries etc. Global annual incidence of TDI is estimated to be 4.5% with approximately, one-third of adult population affected by it [3,4]. Maxillary central incisors are the most commonly involved teeth with less frequent involvement of mandibular central incisors and maxillary lateral incisors [4,5].
Treatment planning for such patients depends on combination of medical, clinical and radiographic findings. Different rehabilitation options include RPD, Fixed Partial Denture (FPD) and Dental Implants. RPD, though universally feasible does not meet patient’s comfort and aesthetic expectations and is thus, reserved only as last resort [6]. FPDs provide better aesthetics but often lead to damage of adjacent healthy hard and soft tissue to derive adequate support [7]. Dental implants are considered as viable treatment alternative, catering to patient’s biomechanical, functional and aesthetic needs. It overcomes drawbacks posed by conventional prosthesis, providing holistic rehabilitation. There are various rehabilitation options for lost maxillary anterior teeth; from RPD to immediate root form implants. Expected complications and long-term outcomes of replaced maxillary anterior teeth have been widely reported. However, literature lacks detail concerning rehabilitation of traumatically lost mandibular anterior teeth.
Rehabilitation of lost mandibular anterior teeth not only facilitates patient’s psychological, functional and aesthetic well-being, but also plays an important role during anterior guidance of the jaw, preventing undue forces on posterior teeth during lateral excursive movements [9]. They also act as a functional landmark for tongue, help in pronunciation of sounds, like ‘s’ and ‘z.’ Mandibular anterior teeth along with tongue and lips modify the airflow for proper articulation of consonants [10].
Maximum bone loss is seen in first year following loss of teeth, with almost a 25% decrease in crestal bone width which increases to up to 40% in three years [11]. Dental implant rehabilitation in such cases thus, require grafting to obtain adequate bone height. Treatment for the current patient was done with an aim of prosthetically-driven rehabilitation wherein, prosthetic considerations were a key factor in treatment planning. Reconstruction and modification of the existing anatomy was considered to provide an ideal environment for optimal implant placement. Although invasive compared to advanced modalities available today, autologous symphysial graft was preferred in our case because of impacted premolar in the region which required extraction. This helped in reducing surgical time and avoided two separate surgical sites and procedures. Symphysial graft provides rich quality bone wherein the cortical layer prevents or reduces bone resorption and the cancellous part helps in fastened bone regeneration [12]. Also, symphyseal graft provide extremely favourable and predictable results with proposed mean gains of 2.1-2.9 mm in buccolingual and apico-coronal directions, six months postoperatively [13,14]. Onlay ridge augmentation in our patient showed successful graft osseointegration with existing alveolar bone without complications. Implant-supported dental prosthesis provided increased functional efficiency to the patient compared to his conventional dentures. Functional bone graft stimulation by implants also ensured reduced future rate of bone resorption [15]. Placement of dental implants without performing ridge augmentation would have compromised the implant length along with an apical positioning of abutment-crown junction ultimately leading to poor aesthetics [16]. In a case report Bäumer D et al., showed successful implant-based rehabilitation of missing mandibular central incisors, lost due to mechanical trauma sustained due to an accident. Because of compromised hard and soft tissue structures in the area, the patient was subjected to ridge augmentation and soft tissue augmentation procedures [8]. Aby J et al., have also shown clinically satisfactory results for autologous symphyseal bone graft combined with implant placement for treatment of missing mandibular central incisor [15].
Diode laser for periodontal surgery offer improved haemostasis, lower oedema, disinfection of target tissue due to local heating and production of eschar layer, reduced postoperative pain and less scar tissue formation. Previously conducted studies have shown that laser assisted frenectomy procedure leads to less postoperative pain as compared to scalpel assisted surgical intervention [8,17]. As expected, the patient reported minimal postoperative pain with no need for taking analgesics. Also, the healing was satisfactory in follow-up visit and was observed to be at a faster rate compared to the periodontist’s previous experience. Uncomplicated healing can be attributed to the fact that lasers provide added advantage of acting as disinfection and detoxification agent thereby, ensuring good healing [18].
Patient Prospective
The patient reported minimal discomfort following either of the two surgical procedures with no need for taking medicines other than those prescribed. The patient was very satisfied with treatment outcomes and expressed increased aesthetic and functional adaptability compared to his previous prosthesis.
Conclusion(s)
The standard of care regarding tooth loss replacement is evolving towards the use of dental implants as removable and fixed prosthesis often cause hard and soft tissue trauma over prolonged use. Use of implants often necessitates reconstruction and modification of proposed site for a successful treatment outcome. Lack of literature towards rehabilitation of edentulous anterior mandible facilitates that more clinicians be encouraged to report the adopted treatment strategies during such cases, spreading knowledge about possible treatment complications and prognosis.
[1]. Kacarska M, Dimtrovski O, Monevska DP, Preprosthetic laser assisted mandibular vestibuloplastyBalk J Dent Med 2016 20:182-85.10.1515/bjdm-2016-0030 [Google Scholar] [CrossRef]
[2]. Riley DS, Barber MS, Kienle GS, Aronson JK, Schoen-Angerer T, Tugwell P, care guidelines for case reports: Explanation and elaboration documentJ Clin Epidemiol 2017 89:218-35.10.1016/j.jclinepi.2017.04.02628529185 [Google Scholar] [CrossRef] [PubMed]
[3]. Lam R, Epidemiology and outcomes of traumatic dental injuries: A review of the literatureAust Dent J 2016 61(Suppl 1):04-20.10.1111/adj.1239526923445 [Google Scholar] [CrossRef] [PubMed]
[4]. Andersen JO, Andersen FM, Andersen L, Textbook and Color Atlas of Traumatic Injuries to the Teeth 2019 5th edUSAWiley BlackwellChapter 11: Classification, Epidemiology and Etiology; pp. 252-94 [Google Scholar]
[5]. Zaleckiene V, Peciuliene V, Brukiene V, Drukteinis S, Traumatic dental injuries: Etiology, prevalence and possible outcomesStomatologija 2014 16(1):07-14. [Google Scholar]
[6]. Abouelkomsan AM, Butt AM, Dall AQ, Removable partial dentures: Patient satisfaction with associated demographic and biomechanical factorsPakistan Oral and Dental Journal 2012 32(3):564-68. [Google Scholar]
[7]. Tan K, Li AZJL, Chan ESY, Patient satisfaction with fixed partial dentures: A 5-year retrospective studySingapore Dent J 2005 27(1):23-29. [Google Scholar]
[8]. Bäumer D, Zuhr O, Hürzeler M, Replacement of mandibular central incisors with implant-supported crowns: A case reportInt J Esthet Dent 2016 11(2):204-18. [Google Scholar]
[9]. Pawah S, Gupta A, Shukla P, Madan B, Rehabilitation of mandibular anterior teeth: Need of adequate incisal guidanceIndian J Oral Sci 2013 4:44-47.10.4103/0976-6944.118544 [Google Scholar] [CrossRef]
[10]. Hyde AC, Moriarty L, Morgan AG, Elsharkasi LM, Deery C, Speech and the dental interfaceDental Update 2018 45(9):795-803.10.12968/denu.2018.45.9.795 [Google Scholar] [CrossRef]
[11]. Mittal Y, Jindal G, Garg S, Bone manipulation procedures in dental implantsIndian J Dent 2016 7(2):86-94.10.4103/0975-962X.18465027433052 [Google Scholar] [CrossRef] [PubMed]
[12]. Desai AJ, Thomas R, Tarun Kumar AB, Mehta DS, Current concepts and guidelines in chin graft harvesting: A literature reviewInt J Oral Health Sci 2013 3:16-25.10.4103/2231-6027.122094 [Google Scholar] [CrossRef]
[13]. Misch CM, Ridge augmentation using mandibular ramus bone grafts for the placement of dental implants: Presentation of a techniquePract Periodontics Aesthet Dent 1996 8(2):127-35.quiz 138 [Google Scholar]
[14]. Puri S, Ridge Augmentation with autogenous bone graft in anterior region: A case seriesJ Adv Med Dent Scie Res 2019 7(8):37-41. [Google Scholar]
[15]. Tamrkar AK, Rathee M, Mallick R, Murali G, Singh B, Rehabilitation of patients with fixed implant supported prostheses: A revisit to the moderate shortened dental arch conceptAnnals of Dental Speciality 2016 4(3):70-72. [Google Scholar]
[16]. Aby J, Salim SP, Sunny NA, Ridge augmentation using mandibular symphyseal bone graft for the placement of dental implant-A case reportWorld Journal of Pharmaceutical and Medical Research 2020 6(2):97-102. [Google Scholar]
[17]. Patil P, Kabbur KJ, Madaiah H, Satyanarayana S, Diode laser frenectomy: A case report with review of literatureJ Dent Lasers 2019 13:19-22.10.4103/jdl.jdl_1_19 [Google Scholar] [CrossRef]
[18]. Yadav RK, Verma UP, Sajjanhar I, Tiwari R, Frenectomy with conventional scalpel and Nd:YAG laser technique: A comparative evaluationJ Indian Soc Periodontol 2019 23:48-52.10.4103/jisp.jisp_352_1830692743 [Google Scholar] [CrossRef] [PubMed]
[19]. Aoki A, Mizutani K, Schwarz F, Sculean A, Yukna RA, Takasaki AA, Periodontal and peri-implant wound healing following laser therapyPeriodontol 2000 2015 68:217-69.10.1111/prd.1208025867988 [Google Scholar] [CrossRef] [PubMed]