Umbilical Deposit in Metastatic Breast Cancer
Anju Anna Abraham1, TM Anoop2, P Rona Joseph3, Steffi Chacko4
1 Senior Resident, Department of Medical Oncology, Regional Cancer Centre, Thiruvananthapuram, Kerala, India.
2 Associate Professor, Department of Medical Oncology, Regional Cancer Centre, Thiruvananthapuram, Kerala, India.
3 Assistant Professor, Department of Medical Oncology, Regional Cancer Centre, Thiruvananthapuram, Kerala, India.
4 Senior Resident, Department of Medical Oncology, Regional Cancer Centre, Thiruvananthapuram, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: TM Anoop, Associate Professor, Department of Medical Oncology, Regional Cancer Centre, Thiruvananthapuram, Kerala, India.
E-mail: dranooptm@yahoo.co.in
Mastectomy, Sister Mary Joseph nodule, Umblcal nodule
Sister Mary Joseph nodule or Sister Mary Joseph Sign refers to a palpable umbilical nodule as a result of metastasis from disseminated malignancy. It is a rare finding and is a sign of advanced stage of malignancy. Gastrointestinal malignancies and gynaecologic malignancies account for most cases of umbilical deposit. Here, the authors describe a case of disseminated metastatic breast cancer with umbilical metastasis as Sister Mary Joseph nodule.
A 59-year-old postmenopausal lady presented with progressive abdominal distension and exertional breathlessness of two months duration. The patient had history of triple negative breast cancer treated in December 2017 with neoadjuvant chemotherapy, modified radical mastectomy and adjuvant radiation. Clinical examination revealed enlarged right axillary lymph node, distended abdomen with pelvic mass, ascites and an infected pea sized umbilical lesion clinically suggestive of Sister Mary Joseph nodule [Table/Fig-1].
Clinical Photograph of patient showing distended abdomen with an umbilical nodule.

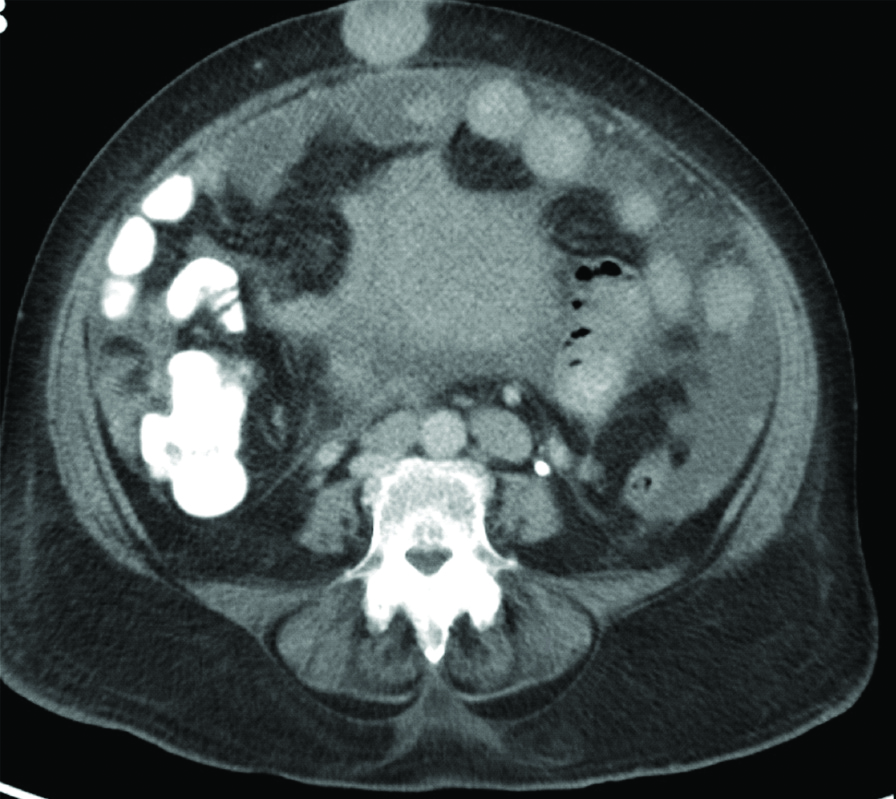
A Computer Tomography (CT) of abdomen and pelvis showed an umbilical deposit with size of 3.4×3.3 cm [Table/Fig-2] along with moderate ascites, multiple peritoneal and omental deposits. A bulky uterus with mass like enhancement in endometrial cavity and Peritoneal and Omental Deposits (POD) were also noted. Metastatic evaluation with CT of chest, abdomen and pelvis also revealed mediastinal lymphadenopathy, lung and liver metastasis. Right axillary lymph node biopsy showed metastatic adenocarcinoma. Immunohistochemistry revealed negative staining for estrogen, progesterone and HER2/Neu receptors. Final diagnosis of disseminated metastatic breast cancer with umbilical deposit was considered.
Initial Computer Tomography of Abdomen and pelvis showing multiple peritoneal, omental and umbilical deposits.
Patient received palliative chemotherapy with single agent carboplatin for six cycles. Evaluation done three weeks after sixth cycle of palliative chemotherapy with CT scan showed progressive increase in size of peritoneal deposits, ascites and lung metastasis. Patient opted for follow-up with supportive care thereafter. The first umbilical metastasis was described by Storer in 1864. Sir Hamilton Bailey coined the term “Sister Mary Joseph nodule” as this sign was first identified by Sister Mary Joseph who was a surgical assistant to Dr William James Mayo, in patients being prepared for surgery in 1928 [1].
The nodules are typically firm and irregular, located at dermal, subcutaneous or peritoneal level. They may be sometimes painful, ulcerate or fistulise with a serous, purulent or bloody discharge. Commonly encountered primary tumours associated with umbilical metastasis include stomach, ovary, colorectal and pancreas [2]. The presence of an umbilical metastasis indicates a poor prognosis and is a sign of disseminated malignancy [3]. The differential diagnosis of umbilical nodule is Sister Mary Joseph nodule, umbilical granuloma, umbilical hernia, endometriosis, omphaliths and keloid [4]. Sister Mary Joseph nodule is associated with evidence of disseminated malignancy especially with gastric and genitourinary malignancies [5,6].
Umbilical endometriosis usually occurs in reproductive age group with bleeding from umbilcal nodule during menstruation [7,8]. Omphaliths are formed due to poor personal hygiene which results in accumulation of sebum and exfoliated skin within the umbilicus [9]. Umbilical keloids usually have a history of trauma or umbilical piercing [10]. Umbilical hernia may be congenital or postsurgical in origin.
This article highlights the importance of keeping Sister Mary Joseph nodule in the differential diagnoses for umbilical hernia. Though rare, breast metastasis may present as umbilical hernia.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 18, 2020
Manual Googling: Aug 01, 2020
iThenticate Software: Oct 23, 2020 (21%)
[1]. Dar IH, Kamili MA, Dar SH, Kuchaai FA, Sister Mary Joseph nodule a case report with review of literatureJ Res Med Sci 2009 14(6):385-87. [Google Scholar]
[2]. Larbcharoensub N, Pongtippan A, Pangpunyakulchai D, Phongkitkarun S, Lertsithichai P, Dejthevaporn TS, Sister Mary Joseph nodule caused by metastatic desmoplastic small round cell tumour: A clinicopathological reportMolecular and Clinical Oncology 2016 5(5):557-61.10.3892/mco.2016.100227900084 [Google Scholar] [CrossRef] [PubMed]
[3]. Larentzakis A, Theodorou D, Fili K, Manataki A, Bizimi V, Tibishrani M, Sister Mary Joseph’s nodule: Three case reportsCases Journal 2008 1:18210.1186/1757-1626-1-18218816407 [Google Scholar] [CrossRef] [PubMed]
[4]. Tso S, Brockley J, Recica H, Ilchyshyn A, Sister Mary Joseph’s nodule: An unusual but important physical finding characteristic of widespread internal malignancyBr J Gen Pract 2013 63(615):551-52.10.3399/bjgp13X67390024152477 [Google Scholar] [CrossRef] [PubMed]
[5]. Dubreuil A, Dompmartin A, Barjot P, Louvet S, Leroy D, Umbilical metastasis or Sister Mary Joseph’s noduleInt J Dermatol 1998 37:07-13.10.1046/j.1365-4362.1998.00326.x9522229 [Google Scholar] [CrossRef] [PubMed]
[6]. Gabriele R, Conte M, Egidi Borghese M, Umbilical metastases: Current viewpointWorld J Surg Onc 2015 3:1310.1186/1477-7819-3-1315723695 [Google Scholar] [CrossRef] [PubMed]
[7]. Dadhwal V, Gupta B, Dasgupta C, Shende U, Deka D, Primary umbilical endometriosis: A rare entityArch Gynecol Obstet 2011 283(suppl 1):119-20.10.1007/s00404-010-1809-221170542 [Google Scholar] [CrossRef] [PubMed]
[8]. Von Stemm AMR, Meigel WN, Scheidel P, Gohct A, Umbilical endometriosisJ Eur Acad Dermatol Venereol 1999 12:30-32.10.1016/S0926-9959(98)00099-3 [Google Scholar] [CrossRef]
[9]. Gallouj S, Harmouch T, Amarti A, Fatima Z, Omphalolith: A rare entity but important to recognizeDermatol Online J 2014 20(5):2264110.5070/D320502264124852780 [Google Scholar] [CrossRef] [PubMed]
[10]. Kydd AR, Patel D, Schwarz J, Joseph D, Mitchell G, Thomas S, Umbilical endometriosis mistaken for a keloid in a premenopausal woman of Caribbean descentJAAD Case Rep 2016 2(3):219-21.10.1016/j.jdcr.2016.03.00927294186 [Google Scholar] [CrossRef] [PubMed]