Spontaneous Intramural Oesophageal Haematoma (IEH) is a rare oesophageal emergency. This report describes the case of a 70-year-old diabetic male, who presented with chest pain and was started on thrombolysis as Electrocardiography (ECG) showed ST elevation Myocardial Infarction (MI). As the patient developed gum bleeding and neck swelling, thrombolysis was stopped. Computed Tomography (CT) showed a non-enhancing mediastinal mass, causing significant extrinsic compression of the distal trachea and a diagnosis of IEH, possibly secondary to thrombolysis was made. Although IEH generally resolves spontaneously with conservative management, the patient remained poorly ventilated despite intubation and expired due to cardiac arrest following failure of resuscitative efforts, eight days after the initial thrombolysis. Several cases of uncomplicated IEH where complete recovery was achieved with conservative treatment are reported in literature; however, there are fewer reports on the poorer outcomes in patients with multiple co-morbidities and co-existent clinical complications.
Case Report
A 70-year-old male with diabetes mellitus for 15 years on irregular treatment (HbA1c: 8.2%) and ex-smoker (smoked for 20 years, before quitting), presented to a nearby hospital with complaints of right-sided chest pain radiating to the right arm for a few hours, followed by an episode of syncope. Patient was started on intravenous thrombolysis with streptokinase after his ECG showed ST elevation infarction involving the inferior myocardial wall. Approximately, 40 minutes into the thrombolysis, the patient developed gum bleeding (approximately 1 million IU streptokinase had been infused at that point). Hence, thrombolysis was stopped immediately. The vitals remained stable, with blood pressure 120/70 mm Hg and saturation 95% in room air.
The patient was referred to another hospital. Investigations showed low haemoglobin (8.2 g/dL), normal platelet levels (183×103/microL) and normal INR value (1.1). Elevated D-Dimer level (4.5 mg/L), suggestive of an abnormally increased clot formation. The patient was desaturated and subsequently developed cardiac arrest (hypoxia induced). The cardiac rhythm reverted, following cycles of CPR. In view of persistent hypoxia, the patient was intubated and saturation was maintained at 94%. The same day, he was taken up for coronary angiogram, which showed 95% stenosis of proximal Right Coronary Artery (RCA). Subsequently, Percutaneous Transluminal Coronary Angioplasty (PTCA) was done. There were no procedural complications. Since the initial pulmonology opinion was Chronic Obstructive Pulmonary Disease (COPD), bronchodilator therapy was stepped up. The patient’s hypoxia seemed to improve and the patient was extubated. Over 48 hours from the onset of bleeding manifestations, the patient’s haemoglobin dropped from 8.7 to 6.6 g/dL. One unit of packed RBCs was transfused, following which haemoglobin improved to 7.4 g/dL.
The next day, the patient again developed bronchospasm and cardiac arrest. The saturation dropped to 81%. The patient was revived with four cycles of resuscitation and reintubated due to persistent stridor. Chest X-ray showed mediastinal widening. Bronchoscopy revealed extrinsic compression of the distal trachea with edematous inflammation. Bronchial narrowing due to the extrinsic compression prevented advancement of the bronchoscope beyond the distal trachea. As plain CT revealed a mediastinal mass, the patient was referred to us for further management of the mediastinal mass.
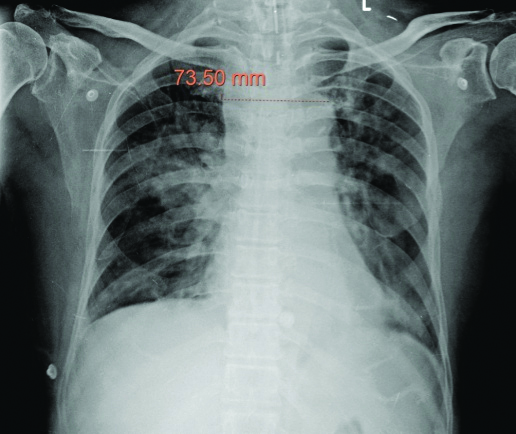
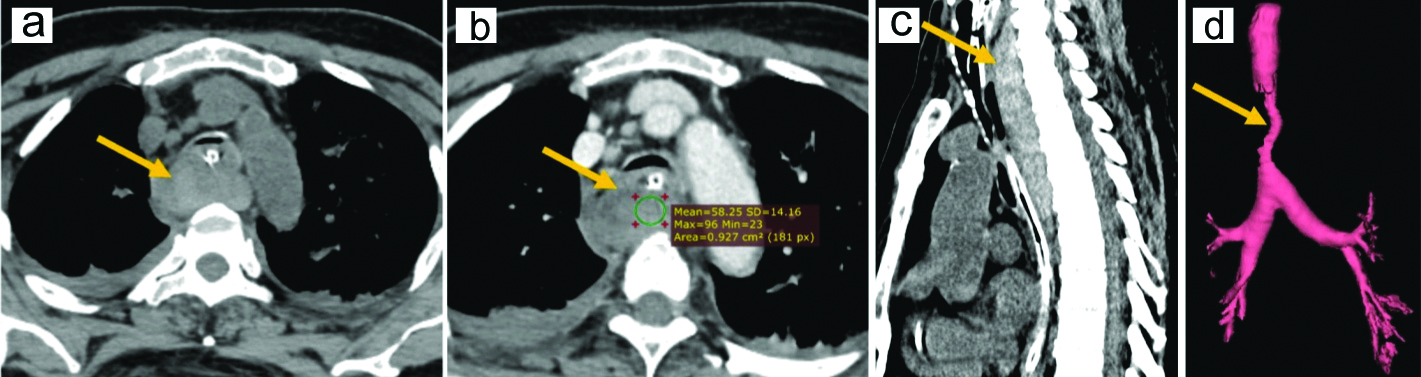
A repeat chest X-ray showed persistent mediastinal widening [Table/Fig-1]. Contrast enhanced computed tomography of the chest showed a hyperdense collection within the oesophageal wall, extending from C5 to T6 vertebral level with no significant wall enhancement on contrast imaging. The mass caused extrinsic compression of the trachea, reducing the distal tracheal lumen to a mere crescent shaped slit. This was also seen on 3-D volumetric analysis [Table/Fig-2]. Multiple scattered consolidations in bilateral lung fields and bilateral pleural effusion were also seen. A diagnosis of IEH probably secondary to thrombolysis was made.
Chest x-ray taken in Posteroanterior view showing mediastinal widening.
(a) Plain CT image in axial section at the level of the trachea shows collection in the oesophageal wall and narrowing of the tracheal lumen to a mere slit. Contrast enhanced CT images of the IEH; (b) Axial section image shows a hyperdense collection within the oesophageal wall, with no significant wall enhancement. Extrinsic compression of the trachea by the mass is noted, reducing the tracheal lumen to a mere crescent shaped slitl; (c) Sagittal section image shows the vertical extent of the IEH; (d) 3-D volumetric analysis showing severe compression (arrow) of the distal trachea and the carina by the IEH.
Despite intubation, the external compression over the distal trachea caused the patient to remain poorly ventilated. The patient was also on continuous ionotropic support. After 8 days of the initial thrombolysis, the patient expired following two episodes of cardiac arrest, with failure of resuscitative efforts.
Discussion
IEH also known as intramural rupture of the oesophagus and oesophageal apoplexy is a bleeding occurring between the mucosa and muscularis propria of the oesophagus. It is described most commonly in the distal oesophagus, where the absence of striated muscle renders it the least supported part of the oesophagus. However, it can occur in the proximal oesophagus and may also be multifocal.
Although cases of IEH have been reported since the 1940s, the first elaborate case series was presented by Kerr WF in 1980 [1]. IEH is a part of the spectrum of oesophageal injuries, along with Mallory-Weiss Tear and Boerhaave syndrome. The differences between these 3 entities are described in [Table/Fig-3]. The predisposing factors for IEH have been traditionally classified into traumatic, emetogenic, abnormal haemostasis-related, aorta-related and spontaneous albeit with some variations.
The position of IEH in the spectrum of oesophageal injuries and the location of bleed.
| Mallory weiss syndrome | IEH | Boerhaave’s syndrome |
|---|
| Sudden increase in intra-abdominal pressure causes gastric cardia to move into thoracic cavity via hiatus↓Oesophageal mucosal laceration (shear injury) [2]↓Bleed from superficial mucosal vessels into oesophageal lumen↓Presents as haematemesis | Traumatic/nontraumatic factors (discussed in [Table/Fig-2]) predispose to bleeding tendency↓Intramural bleed & haematoma formation↓Bleed limited by mucosal and muscularis propria layers of oesophagus↓Causes dysphagia and chest pain↓With increase in size of haematoma, it may tear into the lumen causing haematemesis | Sudden increase in intra-oesophageal pressure due to forceful retching or vomiting↓Full thickness oesophageal wall perforation↓Bleed into oesophageal lumen and internally into thoracic cavity↓Presents as haematemesis |
IEH: Intramural oesophageal haematoma
Some authors use the term “spontaneous” only when no known risk factor is present whereas some authors use the term “spontaneous” despite the presence of a known coagulopathy to connote the absence of direct oesophageal trauma. This leads to confusion over the implication of term “spontaneous.” In this article, the author have consolidated these risk factors in [Table/Fig-4] to emphasise that IEH can be
“Spontaneous/idiopathic,” in the absence of trauma and underlying risk factors
Facilitated by an indirect underlying factor in the absence of known trauma/trigger
Precipitated by direct identifiable/known trauma in the recent past.
| Aetiological class | Spontaneous/Idiopathic [3] | Underlying risk factor present, but no direct oesophageal injury | Secondary to direct oesophageal injury (Traumatic) |
|---|
| Causes | no known predisposing factor | Sub-optimal haemostasis [2]→ Coagulopathies→ Anticoagulant→ Anti-platelets→ ThrombolysisVessel wall fragility [2]CirrhosisHaemodialysisHypertension [4] | Procedure related→ NG tube insertion [5]→ Endoscopic procedures[6]→ Oesophageal band ligation/sclerotherapy/dilatation→ Injury during CVC insertion [6]Chest traumaEmetogenic/BarotraumaForeign bodyFood abrasion- e.g., Fish bone [6,7]Pill induced oesophagitis [3]Aorto-oesophageal fistula due to [7]→ rupture of thoracic aortic aneurysm/intramural aortic haematoma/postaortic surgery→ penetrating ulcer→ corrosive oesophagitis→ oesophageal malignancies |
IEH: Intramural oesophageal haematoma
The chief symptoms of IEH include chest pain, dysphagia/odynophagia and haematemesis. Most sources describe two of the three symptoms to be present in up to 80% of patients, with the triad occurring in approximately 35% of patients. There is a female preponderance. It is seen mainly in the middle- aged and elderly population [2,6] although, it has also been reported in younger patients [7].
Based on the extent of disease progression and effects, four stages of IEH are recognised [4,8].
Stage I: Isolated haematoma.
Stage II: Haematoma surrounded by tissue oedema.
Stage III: Haematoma with oedema compresses and narrows the oesophageal lumen.
Stage IV: Haematoma, oedema and clot formation obliterate the oesophageal lumen.
IEH can be eccentric or concentric, depending on the extent of circumferential involvement. IEH can be imaged using chest X-ray (may show mediastinal widening), barium swallow (may show double barrel sign of oesophagus/mucosal stripe sign) and upper Gastrointestinal (GI) endoscopy (may show mucosal bulge with or without discoloration of mucosa with luminal narrowing, with or without intraluminal bleed). However, contrast enhanced CT scan remains the gold standard investigation as it is noninvasive, causes minimal patient discomfort, and is useful in excluding other diagnosis, while allowing assessment of the exact extent of the lesion. CT usually demonstrates a high attenuating non-enhancing mass (except, if caused by aorto-oesophageal fistula) within the oesophageal wall, causing concentric or eccentric thickening of the oesophageal wall, with resultant compression or complete obliteration of the lumen.
The patient presented with gum bleeding during thrombolysis. A mediastinal widening was incidentally picked up on Chest Xray and was further evaluated. However, in all the other case reports [2-6,8], dysphagia was the presenting complaint. It was associated with chest pain in some cases [4,5,8] and with haemoptysis [2] and blood straked vomitus [5] in one instance each. Of the six cases, two patients were on anticoagulants [2,8], two were treated with aspirin [5,6], one patient had idiopathic thrombocytopenic purpura [4], while another patient was hypertensive but did not have any other predisposing factor [3]. In all cases, there was uneventful recovery with conservative management but in one case, poor outcome was noted in one patient as reported by Hong M et al., a hypertensive with previous history of Peripheral Vascular Disease (PVD). The patient was reported to have presented for Deep Vein Thrombosis (DVT) and Pulmonary Thromboembolism (PTE), but developed IEH as a complication of the anticoagulation of the DVT and PTE. Although the IEH started to resolve, it recurred and was removed endoscopically using Roth net. The patient however, died subsequently due to a second episode of PTE [8].
Myocardial Infarction (MI) is a clinical mimic for IEH- both present as emergencies with chest pain. However, in cases where chest pain is associated with dysphagia or in patients on anticoagulation, haematemesis or haemoptysis, a high index of suspicion for IEH must be maintained. This is because both have diametrically opposite treatment- the initial loading dose of anticoagulation used for treatment of MI can cause catastrophic deterioration in a patient with stable or resolving IEH. Apart from this, it must be kept in mind that IEH can develop as a complication of treatment for MI also; hence, a second episode of chest pain in a patient recently thrombolysed for MI should raise the suspicion for IEH [8].
On imaging, IEH can appear similar to oesophageal duplication cyst, oesophageal malignancy and Boerhaave’s syndrome. Oesophageal duplication cysts appear as thick-walled homogenous, smooth, round or elliptic mass adjacent to or within the oesophageal wall. They may compress on the oesophagus and produce dysphagia. Boerhaaves syndrome appears similar but is differentiated by the presence of contrast leak due to perforation and may show air pockets adjacent to the oesophagus. Oesophageal malignancies usually enhance on intravenous contrast administration and are associated with constitutional symptoms. Except IEH caused due to aorto-oesophageal fistula (requires surgical intervention), other causes warrant only conservative management. Prognosis is generally excellent with spontaneous resolution of the haematoma, generally within three weeks. However, as seen in this report and in that by Hong M et al., higher mortality rates are encountered when associated with other concurrent life-threatening disease processes [8].
Conclusion(s)
IEH is a well-established, albeit rare oesophageal emergency. Unlike other oesophageal emergencies, it usually resolves spontaneously with supportive measures and rarely requires the surgical intervention. It is also important to distinguish it from other mimics like Boerhaave syndrome and myocardial infarction which require an active, immediate and different line of management. This case demonstrates the diagnostic difficulties encountered in the evaluation and management of such patients. IEH should be kept in mind as a potential cause for acute chest pain and dysphagia, and also as a rare complication of thrombolysis.
IEH: Intramural oesophageal haematoma
IEH: Intramural oesophageal haematoma
[1]. Kerr WF, Spontaneous intramural rupture and intramural haematoma of the oesophagusThorax 1980 35:890-97.10.1136/thx.35.12.8906973833 [Google Scholar] [CrossRef] [PubMed]
[2]. Trip J, Hamer P, Flint R, Intramural oesophageal haematoma-A rare complication of dabigatranN Z Med J 2017 130(1456):80-82. [Google Scholar]
[3]. Lee SW, Yeh HZ, Chang CS, Ko CW, Lee TY, Endoscopic ultrasound images of esophageal intramural hematomaJ Med Ultrasound 2010 18(4):161-63.10.1016/j.jmu.2010.06.001 [Google Scholar] [CrossRef]
[4]. Sharma K, Wang Y, Submucosal esophageal hematoma precipitated by chronic idiopathic thrombocytopenic purpuraJ Radiol Case Rep 2017 12(2):278-80.10.1016/j.radcr.2017.01.02228491169 [Google Scholar] [CrossRef] [PubMed]
[5]. Silva MJ, Saiote J, Salvado V, Nunes AP, Durate P, Intramural hematoma of the esophagus after thrombolysis for ischemic strokeAm J Emerg Med 2015 33(3):481.e1-481.e2.10.1016/j.ajem.2014.08.06925239697 [Google Scholar] [CrossRef] [PubMed]
[6]. Seneviratne S, Kumara D, Drahaman A, Spontaneous intramural oesophageal haematoma: A case reportMed J Malaysia 2012 67:536-37. [Google Scholar]
[7]. Restrepo CS, Lemos DF, Ocazionez D, Moncada R, Gimenez CR, Intramural hematoma of the esophagus: A pictorial essayEmerg Radiol 2007 15(1):13-22.10.1007/s10140-007-0675-017952475 [Google Scholar] [CrossRef] [PubMed]
[8]. Hong M, Warum D, Karamanian A, Spontaneous intramural esophageal hematoma (IEH) secondary to anticoagulation and/or thrombolysis therapy in the setting of a pulmonary embolism: A case reportJ Radiol Case Rep 2013 7(2)10.3941/jrcr.v7i2.121023705034 [Google Scholar] [CrossRef] [PubMed]