Corona Virus Disease (COVID-19) has resulted in restriction of face-to-face consultations and mechanisms to access health care. Oesteoarthritis (OA) is one of the most common forms of musculoskeletal disease encountered and a leading cause of painful disability in adults and elderly. The assessment of the challenges and strategies encountered in the nonoperative management of OA of knee care during the COVID-19 pandemic was done. A comprehensive review of the literature using suitable keywords such as ‘COVID-19’, ‘OA’, ‘OA knee’, ‘knee joint’ on the search engines of PubMed, SCOPUS, Google Scholar and Research Gate in May 2020 on developments and guidance during the current COVID-19 pandemic. The management of OA has been hampered by COVID-19 pandemic lock down with subsequent suspension of elective surgeries. Nonoperative complementary therapy has been evaluated with National Institute for Health and Care Excellence (NICE) recommendations to guide management. Conservative strategies including judicial use of analgesia as recommended by NICE, supportive orthosis, patient education and advice using remote telecommunication consultations play an important role in the nonoperative management of OA till elective surgery can safely resume.
Introduction
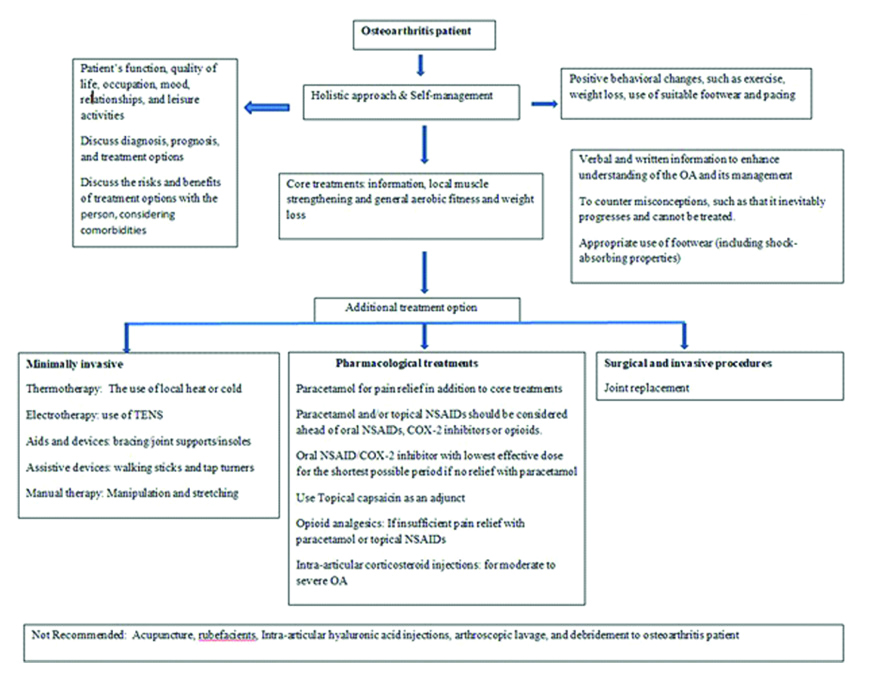
COVID-19 is caused by a novel Coronavirus Severe Acute Respiratory Syndrome-Corona Virus-2 (SARS-CoV-2), predominantly affecting the respiratory system. The mode of transmission for COVID-19 is believed to be through respiratory droplets [1]. The World Health Organisation (WHO) declared the novel Coronavirus outbreak as a pandemic on 11 March, 2020. As the COVID-19 pandemic is spread worldwide, it has became clear that the health care system needs to evolve and develop strategies for COVID-19 as effectively as possible and also provide a continuity of patient care with other medical ailments like knee OA. Lockdown, social distancing and infection prevention strategies have had a significant impact on management of medical and orthopaedic conditions such as OA. All elective orthopaedic surgeries have been suspended. OA is one of the most common form of musculoskeletal disease and a leading cause of pain and disability in adults and elderly. The Indian Orthopaedic Association (IOA), British Orthopaedic Association (BOA) and other organisations have provided guidelines to manage patients with trauma and other emergency orthopaedic conditions during the pandemic [2,3]. However, there are no specific guidelines for coping with chronic painful and disabling musculoskeletal problems like knee OA whilst elective services stand suspended. The emergence of COVID-19 pandemic has significantly impacted orthopaedic surgeons, physicians and their patients worldwide [4]. Consequently, COVID-19 has had a significant impact on pain, joint function, physical function, and physical activity in patients with end-stage hip and knee OA [5]. Conservative strategies to manage OA had to be reinforced to support these patients. NICE has updated some recommendations for management of arthritis during the pandemic [Table/Fig-1] [6].
Managing options for Osteoarthritis during COVID-19.
TENS- Transcutaneous electrical nerve stimulation; NSAIDs- Nonsteroidal anti-inflammatory drugs;COX- Cyclooxygenase; OA-Osteoarthritis
Initial studies have shown that there is also significant musculoskeletal dysfunction in some patients with COVID-19 [7]. There can be likely association of both COVID-19 and OA; as they involve elderly patients with common risk factors. Less is known about musculoskeletal disorders in patients with COVID-19. Arthralgia is commonly reported in patients with COVID-19 [7]. The possible mechanism of chondrolysis, arthralgia, and bone mineral loss in COVID-19 has been explained by induction of inflammation in lung and which can excessively release the inflammatory cytokines, especially the up-regulation of interleukins such as interleukin 6, 8, 17 and 1β, the systemic inflammation marker C-X-C motif chemokine ligand 10 (CXCL10), Interferon gamma (IFNγ) and Tumor Necrosis Factor-α (TNFα) affecting bone and joint along with other organs. IL-1β, IL-6, and TNF-α can lead to chondrolysis which could result in arthralgia or progression of OA in some patients [8]. Therefore, in patients with existing OA with COVID-19, the symptoms will be more pronounced due to these inflammatory markers or it may be the first symptom which can confuse orthopaedic surgeon for the diagnosis of OA. The presence of arthralgia may lead to a confusion to the orthopaedic surgeon for diagnosis of pain due to OA and further delay the recognition of COVID-19 [9]. Before COVID-19 pandemic, the demand for Total Knee Arthroplasty (TKA) had risen substantially over the past decade in countries around the world [10]. Many patients underwent TKA due to knee OA. During COVID-19, the elective arthroplasty cases have been postponed at most hospitals across world. The suffering of these patients requiring TKA surgery increased tremendously.
Most of the literature published during this pandemic has focused on the management of COVID-19 confirmed cases or the emergency cases. Therefore, in this review, authors have highlighted the challenges and tried to provide insight in the complementary nonoperative intervention strategies that can be applied to manage chronic orthopaedic conditions such as knee OA during COVID-19 pandemic, till elective services resume.
Challenges in Managing OA of the Knee Nonoperatively during the COVID-19 Pandemic
Pain is the predominant symptom of the OA; others are brief morning stiffness and functional limitations. Clinically, the knee joint is the most common site [11]. The prevalence of knee OA is alarmingly high (about 22% to 39%) in India [12]. Since outpatient services have been deferred due COVID-19 pandemic lockdown, the impact on knee OA patients has been profound. Inability to access services has led to finding solutions for the pain management and providing remote support possibilities. The American Association of Hip and Knee Surgeons (AAHKS) and other associations during COVID-19 outbreak have recommended continued non-surgical treatment for OA [13]. Recently the Osteoarthritis Research Society International (OARSI) has updated and expanded its guidelines by developing patient-focused treatment recommendations for individuals with knee and other joints OA [14].
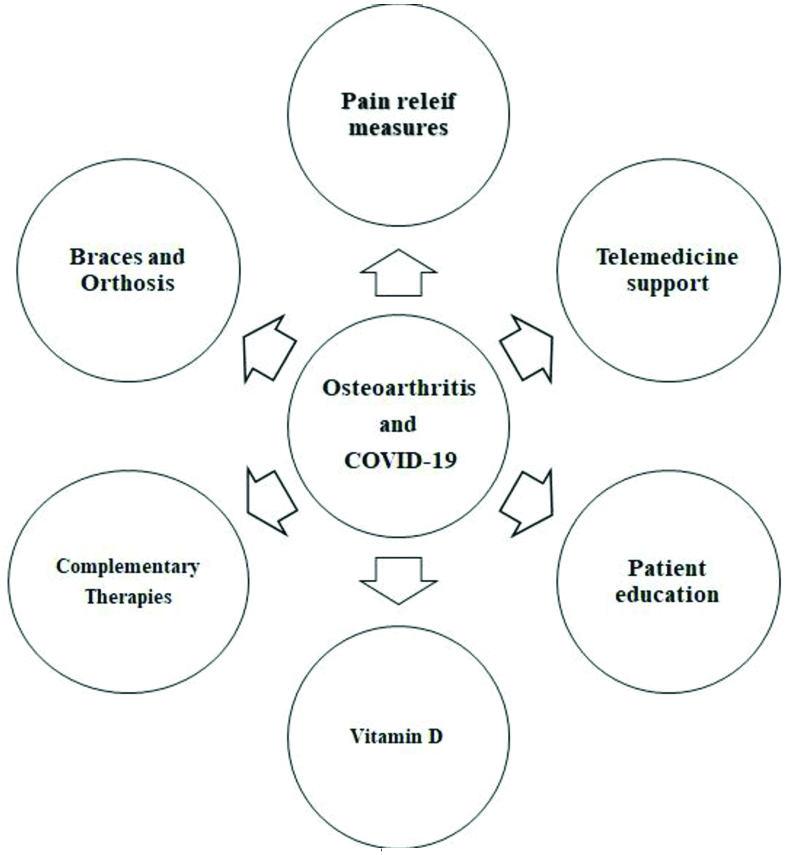
Conservative, Nonoperative Management Strategies for OA during the COVID-19 Pandemic
1. Pain Relief Measures
These include the use of painkillers like Paracetamol (PCM), Tramadol and NonSteroidal Anti-Inflammatory Drugs (NSAIDs), Knee braces, Insoles inside the shoes, Intra-Articular (IA) injections (steroid or hyaluronic acid), stretching, and low-impact knee exercises [Table/Fig-2]. Managing pain in patients with OA is the key issue. Since PCM forms the first rung of the analgesic ladder, some patients may require further supportive medication to manage their pain especially during the current pandemic and lockdown guidelines.
Conservative management options for OA during COVID-19.
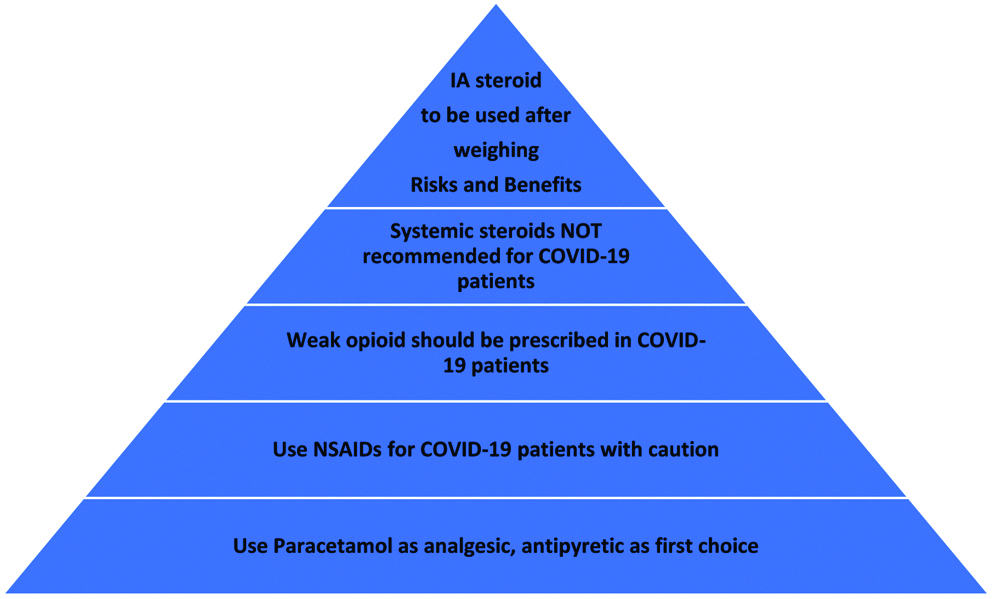
PCM use may affect cardiovascular system, liver and kidney at high doses. As most of the COVID-19 patients died due to renal failure, its use should be carefully monitored in OA patients associated with COVID-19 [15]. The relevance of PCM is its use for the longest duration, usually for more than 20 days per month, due to its safety at correct dose. Although NSAIDs are related to gastrointestinal and renal side effects; increased respiratory infection and bronchoconstriction has been reported. These drugs should be used cautiously in patients with Diabetes Mellitus (DM). Patients should be watched for complications related to diabetic nephropathy. There is controversy regarding the use of second line drugs such as NSAIDs as it may aggravate COVID-19 symptoms. There is no direct correlation between their use and COVID-19 [16]. Currently, there is no evidence for discontinuation of NAIDSs; their use should benefit for patients with weak symptoms. NSAIDs are to be used at the minimum effective dose for the shortest time possible. Recently, authors have recommended the use of acetaminophen for controlling fever and inflammation and to be cautious about using NSAIDs in management of COVID-19 patients until there is enough evidence [17]. Opioids have increased risk for adverse events in OA patients including respiratory depression. The use of opioids could potentially lead to increased susceptibility to COVID-19 complications like pneumonia, but no direct evidences have been reported. Whenever the use of opioid is required, a weak opioid with no immunosuppressive activity, as for example tramadol, buprenorphine should be preferred with caution [18]. Use of morphine and fentanyl should be avoided as both are most immunosuppressive. Topical analgesic creams and patches can be used as an adjunct or substitute to the oral medications [19]. In a systematic review, Derry S et al., identified that topical NSAIDs can alleviate pain for chronic musculoskeletal pain in adults [20]. Topical NSAIDs moderately relief pain, with efficacy similar to that of oral NSAIDs. They have a better risk: benefit ratio [21]. Complementary therapies like heat or ice packs to the affected joint may reduce the local inflammation, decreases swelling and help in alleviating symptoms [22].
2. Intra-articular injections for OA
IA corticosteroid injection has been recommended for knee OA for patients who have not responded to oral analgesics. It provides short-term pain relief for up to six weeks; however its use may result in infection, accelerate degradation of the articular cartilage in the knee, and can cause subchondral insufficiency fractures [23]. This further potentiates symptoms of OA. Theoretically, the use of IA steroid injection in COVID-19 patients can cause transient reduction in immunity which could make patients more susceptible to COVID-19, may cause reduction in vaccine efficacy and may cause suppression of hypothalamic-pituitary-adrenal axis but no association with virus clearance and duration of symptoms in COVID-19 has been reported after use of steroid. Consequently, the British Society of Skeletal Radiologists advocates avoiding the use of IA steroid injection whenever possible during the COVID-19 pandemic to reduce the above risks [24]. Further, the use of IA steroid should be avoided in patient with uncontrolled blood sugar levels. IA injection of Hyaluronic Acid (HA) as a visco-supplement and Platelet Rich Plasma (PRP) are other available options for the pain relief in knee OA [6].
A summary of the current literature from an orthopaedic perspective and NICE recommendations is highlighted in [Table/Fig-3] [25].
COVID-19 NICE and recent literature recommendations for analgesic ladder [25].
National Institute for Health and care Excellence (NICE): Coronavirus (COVID-19). Arthritis: Available from: https://www.nice.org.uk/guidance/conditions-and-diseases/musculoskeletal-conditions/arthritis
IA: Intra-articular; NICE: National institute for health and care excellence; NSAID: Nonsteroidal anti-inflammatory drug
3. Role of Bracing and Orthosis
Bracing for knee OA is a non-invasive option which provides biomechanical stability and significantly reduces pain and improve function. Bracing may provide more time to those patients who want to undergo TKA during COVID-19 pandemic.
Since many patients waiting for TKA must have deformities; and the use of an off-loader knee brace (e.g., valgus knee brace for knee OA with varus deformity) gives good support to the knee and helps these patients in pain relief and walking [26]. A walking stick or a cane is extremely helpful in offloading the arthritic joint and relieving pain. A lateral wedge insole inside the shoe helps in offloading the medical compartment of the knee, which is mostly affected in knee OA.
4. Role of remote strategies in managing OA during current pandemic
The core treatments for OA knee include lifestyle changes, low-impact land-based exercise with or without dietary weight management in patients with obesity [27]. Control of blood sugar in DM patients is important to halt progress of OA. A recent randomised trial showed that patients with OA of the knee who underwent physical therapy suffer less pain and functional disability than patients who received an IA glucocorticoid injection [28]. Physical therapy and remote counselling can play an important role during the current pandemic situation. With the aim to reduce ‘face-to-face’ consultation, social distancing and shielding guidelines, remote technologies like telephone or video technologies are increasingly being used to support and manage chronic orthopaedic conditions [29-31]. Physical therapy can be advised and monitored via web-based technologies available on social media to patients staying at home during lockdown for their relief of symptoms, functional improvement, and a decreased need for pain killers.
5. Yogasana
To improve proprioception and joint function in OA patients, balance exercises and yoga can be advised to the patients. A systematic review and meta-analysis found that yoga is beneficial for OA of the knee with regard to pain intensity, physical function, and stiffness [32]. Yoga involves gentle exercises and stretches combined with deep breathing [33]; which will reduce stress related to pain and COVID-19. Yoga improves microcirculation and leg muscle strength supporting knee joint which in turn will decrease joint load. A daily practice of yogasana, pranayama, and meditation for at least 30 minutes as advised by Ministry of AYUSH should be encouraged [34].
6. Role of mental health counselling
There is an increased risk of depression due to disease progression of knee OA, especially during the COVID-19 lockdown phase, due to social distancing, and self-isolation strategies. Duloxetine, an antidepressant can also be used to treat OA pain and depression associated with COVID-19 disease [35]. Telemedicine psychiatric counselling may also help these patients with chronic disorders like knee OA.
7. Patient education and role of Vitamin D
OA patients must be encouraged to eat healthy diet with proper nutrients to avoid weight gain and boost their immunity during the COVID-19 lockdown phase [36]. As deficiency in vitamin D is associated with progression of knee OA, its supplementation in OA patients should also be recommended if the dietary intake is poor or have vitamin D deficiency [37]. It is recommended that people at risk consider taking 10,000 IU/d of vitamin D3 for a few weeks, followed by 5000 IU/d. The goal should be to raise 25(OH) D concentrations above 40-60 ng/mL (100-150 nmol/L) [38].
Patient education about the OA is also an important component for management. The education of surgeons to educate patients about how to self-manage during the COVID-19 pandemic is an essential thought process [39]. Clinicians should be encouraged to learn to provide continuity of care with new referrals and follow-up patients, thus, establishing a new way of professional relationship with their patients [40].
Conclusion(s)
Patients with OA knee are recommended to use conservative options such as minimal use of analgesics, orthosis and modification of activities of daily living during the COVID-19 pandemic. The nonoperative management is important for OA patients till the hospitals resume elective surgery. A physician’s advice via telecommunication will help reduce face-to-face consultation and therefore, prevent spread of infection to patient and health care provider.
[1]. Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, China novel coronavirus investigating and research team. A novel coronavirus from patients with pneumonia in China, 2019N Engl J Med 2020 382(8):e727-33.Epub 2020 Jan 2410.1056/NEJMoa200101731978945 [Google Scholar] [CrossRef] [PubMed]
[2]. Indian Orthopaedic Association. COVID-19 IOA guidelines. New Delhi: Indian Orthopaedic Association, 2020. Available at: https://www.ioaindia.org/COVID-19IOAguidelines.pdf [Google Scholar]
[3]. British Orthopaedic Association. Management of patients with urgent Orthopaedic conditions and trauma during the coronavirus pandemic. 2020. Available at https://www.boa.ac.uk/resources/covid-19-boasts-combined.html [Google Scholar]
[4]. Jain VK, Vaishya R, COVID-19 and orthopaedic surgeons: The Indian scenario [published online ahead of print, 2020 Apr 21]Trop Doct 2020 :4947552092161610.1177/004947552092161632316857 [Google Scholar] [CrossRef] [PubMed]
[5]. Endstrasser F, Braito M, Linser M, Spicher A, Wagner M, Brunner A, The negative impact of the COVID-19 lockdown on pain and physical function in patients with end-stage hip or knee osteoarthritisKnee Surg Sports Traumatol Arthrosc 2020 28(8):2435-43.10.1007/s00167-020-06104-332556438 [Google Scholar] [CrossRef] [PubMed]
[6]. National Institute for Health and care Excellence (NICE): Coronavirus (COVID-19). Arthritis: Available from: https://www.nice.org.uk/guidance/conditions-and-diseases/musculoskeletal-conditions/arthritis (Accessed 20 August 2020) [Google Scholar]
[7]. Disser NP, De Micheli AJ, Schonk MM, Konnaris MA, Piacentini AN, Edon DL, Musculoskeletal consequences of COVID-19J Bone Joint Surg Am 2020 102(14):1197-204.10.2106/JBJS.20.0084732675661 [Google Scholar] [CrossRef] [PubMed]
[8]. Aizawa T, Kon T, Einhorn TA, Gerstenfeld LC, Induction of apoptosis in chondrocytes by tumour necrosis factor-alphaJ Orthop Res 2001 19(5):785-96.10.1016/S0736-0266(00)00078-4 [Google Scholar] [CrossRef]
[9]. Joob B, Wiwanitkit V, Arthralgia as an initial presentation of COVID-19: ObservationRheumatol Int 2020 40(5):82310.1007/s00296-020-04561-032222804 [Google Scholar] [CrossRef] [PubMed]
[10]. Kurtz S, Ong K, Lau E, Mowat F, Halpern M, Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030J Bone Joint Surg Am 2007 89(4):780-85.10.2106/JBJS.F.0022217403800 [Google Scholar] [CrossRef] [PubMed]
[11]. Hunter DJ, Bierma-Zeinstra S, OsteoarthritisLancet 2019 393(10182):1745-59.10.1016/S0140-6736(19)30417-9 [Google Scholar] [CrossRef]
[12]. Pal CP, Singh P, Chaturvedi S, Pruthi KK, Vij A, Epidemiology of knee osteoarthritis in India and related factorsIndian J Orthop 2016 50(5):518-22.10.4103/0019-5413.18960827746495 [Google Scholar] [CrossRef] [PubMed]
[13]. The American Association of Hip and Knee Surgeons (AAHKS) http://www.aahks.org/covid-19/. (Accessed on June 26, 2020) [Google Scholar]
[14]. Bannuru RR, Osani MC, Vaysbrot EE, Arden NK, Bennell K, Bierma-Zeinstra SMA, OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritisOsteoarthritis Cartilage 2019 27(11):1578-89.10.1016/j.joca.2019.06.01131278997 [Google Scholar] [CrossRef] [PubMed]
[15]. Ronco C, Reis T, Husain-Syed F, Management of acute kidney injury in patients with COVID-19 [published online ahead of print, 2020 May 14]Lancet Respir Med 2020 :S2213-2600(20)30229-010.1016/S2213-2600(20)30229-0 [Google Scholar] [CrossRef]
[16]. Brufen concern in COVID-19 reference-https://www.who.int/news-room/commentaries/detail/the-use-of-non-steroidal-anti-inflammatory-drugs-(nsaids)-in-patients-with-covid-19 [Google Scholar]
[17]. Yousefifard M, Zali A, Zarghi A, Madani Neishaboori A, Hosseini M, Safari S, Non-steroidal anti-inflammatory drugs in management of COVID-19; A systematic review on current evidence [published online ahead of print, 2020 May 27]Int J Clin Pract 2020 :e1355710.1111/ijcp.13557PMC7267090 [Google Scholar] [CrossRef] [PubMed]
[18]. de Girolamo L, Peretti GM, Maffulli N, Brini AT, Covid-19-The real role of NSAIDs in ItalyJ Orthop Surg Res 2020 15(1):165Published 2020 May 410.1186/s13018-020-01682-x32366317 [Google Scholar] [CrossRef] [PubMed]
[19]. Ragni E, Mangiavini L, Viganò M, Brini AT, Peretti GM, Banfi G, Management of osteoarthritis during COVID-19 pandemic [published online ahead of print, 2020 May 21]Clin Pharmacol Ther 2020 :10.1002/cpt.191010.1002/cpt.191032438454 [Google Scholar] [CrossRef] [PubMed]
[20]. Derry S, Conaghan P, Da Silva JA, Wiffen PJ, Moore RA, Topical NSAIDs for chronic musculoskeletal pain in adultsCochrane Database Syst Rev 2016 4(4):CD00740010.1002/14651858 [Google Scholar] [CrossRef]
[21]. Rannou F, Pelletier JP, Martel-Pelletier J, Efficacy and safety of topical NSAIDs in the management of osteoarthritis: Evidence from real-life setting trials and surveysSemin Arthritis Rheum 2016 45(4 Suppl):S18-21.10.1016/j.semarthrit.2015.11.00726806189 [Google Scholar] [CrossRef] [PubMed]
[22]. Brosseau L, Yonge KA, Robinson V, Marchand S, Judd M, Wells G, Thermotherapy for treatment of osteoarthritisCochrane Database Syst Rev 2003 (4):CD00452210.1002/14651858.CD00452214584019 [Google Scholar] [CrossRef] [PubMed]
[23]. Kompel AJ, Roemer FW, Murakami AM, Diaz LE, Crema MD, Guermazi A, Intra-articular Corticosteroid injections in the hip and knee: Perhaps not as safe as we thought?Radiology 2019 293(3):656-63.10.1148/radiol.201919034131617798 [Google Scholar] [CrossRef] [PubMed]
[24]. The British Society of Skeletal Radiologists. 19 March 2020. https://www.bssr.org.uk/static/uploads/forum/Musculoskeletal_Radiology_during_the_COVID-19_Global_Pandemic.pdf [Google Scholar]
[25]. Tan SHS, Hong CC, Saha S, Murphy D, Hui JH, Medications in COVID-19 patients: Summarizing the current literature from an orthopaedic perspective [published online ahead of print, 2020 May 22]Int Orthop 2020 :01-05.10.1007/s00264-020-04643-532445030 [Google Scholar] [CrossRef] [PubMed]
[26]. Parween R, Shriram D, Mohan RE, Lee YHD, Subburaj K, Methods for evaluating effects of unloader knee braces on joint health: A reviewBiomed Eng Lett 2019 9(2):153-68.10.1007/s13534-019-00094-z31168421 [Google Scholar] [CrossRef] [PubMed]
[27]. DeRogatis M, Anis HK, Sodhi N, Ehiorobo JO, Chughtai M, Bhave A, Nonoperative treatment options for knee osteoarthritisAnn Transl Med 2019 7(Suppl 7):S24510.21037/atm.2019.06.6831728369 [Google Scholar] [CrossRef] [PubMed]
[28]. Deyle GD, Allen CS, Allison SC, Gill NW, Hando BR, Petersen EJ, Physical therapy versus glucocorticoid injection for osteoarthritis of the KneeN Engl J Med 2020 382(15):1420-29.10.1056/NEJMoa190587732268027 [Google Scholar] [CrossRef] [PubMed]
[29]. Greenhalgh T, Wherton J, Shaw S, Morrison C, Video consultations for covid-19BMJ 2020 368:m998Published 2020 Mar 1210.1136/bmj.m99832165352 [Google Scholar] [CrossRef] [PubMed]
[30]. van Galen LS, Car J, Telephone consultationsBMJ 2018 360:k104710.1136/bmj.k104729599197 [Google Scholar] [CrossRef] [PubMed]
[31]. Iyengar K, El-Nahas W, A brief guide to telephone medical consultationBritish Journal of Healthcare Management 2020 10.12968/bjhc.2020.0032 [Google Scholar] [CrossRef]
[32]. Lauche R, Hunter DJ, Adams J, Cramer H, Yoga for osteoarthritis: A systematic review and meta-analysisCurr Rheumatol Rep 2019 21(9):47Published 2019 Jul 2310.1007/s11926-019-0846-531338685 [Google Scholar] [CrossRef] [PubMed]
[33]. Tillu G, Chaturvedi S, Chopra A, Patwardhan B, Public health approach of ayurveda and yoga for COVID-19 ProphylaxisJ Altern Complement Med 2020 Apr 20 10.1089/acm.2020.012932310670 [Google Scholar] [CrossRef] [PubMed]
[34]. Ministry of AYUSH. Ayurveda’s immunity boosting measures for self-care during COVID 19 crisis. https://www.ayush.gov.in/docs/123.pdf (Accessed 20 August 2020) [Google Scholar]
[35]. Enomoto H, Fujikoshi S, Ogawa K, Tsuji T, Tanaka S, Relationship between pain reduction and improvement in health-related quality of life in patients with knee pain due to osteoarthritis receiving duloxetine: Exploratory post hoc analysis of Japanese phase 3 randomised studyJ Pain Res 2020 13:181-91.10.2147/JPR.S21107232021407 [Google Scholar] [CrossRef] [PubMed]
[36]. Fuggle NR, Cooper C, Oreffo ROC, Price AJ, Kaux JF, Maheu E, Alternative and complementary therapies in osteoarthritis and cartilage repairAging Clin Exp Res 2020 32(4):547-60.10.1007/s40520-020-01515-132170710 [Google Scholar] [CrossRef] [PubMed]
[37]. Yu Y, Liu D, Feng D, Zhao J, Association between Vitamin D and knee osteoarthritis: A PRISMA-compliant meta-analysisZ Orthop Unfall 2020 Mar 9 10.1055/a-1098-881532150754 [Google Scholar] [CrossRef] [PubMed]
[38]. Grant WB, Lahore H, McDonnell SL, Baggerly CA, French CB, Aliano JL, Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deathsNutrients 2020 12(4):988Published 2020 Apr 210.3390/nu1204098832252338 [Google Scholar] [CrossRef] [PubMed]
[39]. Saxena A, Bullock M, Danoff JR, Rodd DS, Fischer SJ, Stronach BM, Educating surgeons to educate patients about the COVID-19 pandemicJ Arthroplasty 2020 Apr 18 :PiiS0883-5403(20)30424-1. doi: 10.1016/j.arth.2020.04.037. [Epub ahead of print] [Google Scholar]
[40]. Stahel PF, How to risk-stratify elective surgery during the COVID-19 pandemic?Patient Saf Surg 2020 14:8Published 2020 Mar 3110.1186/s13037-020-00235-932288785 [Google Scholar] [CrossRef] [PubMed]