Displaced Root of 3rd Maxillary Molar Tooth into Infratemporal Fossa- Role of 3D CT Scan
Sanjay M Khaladkar1, B Nagi Reddy2
1 Professor, Department of Radiodiagnosis, Dr. D.Y. Patil Medical College and Research Centre, Dr. D.Y. Patil Vidyapeeth, Pune, Maharashtra, India.
2 Postgraduate Resident, Department of Radiodiagnosis, Dr. D.Y. Patil Medical College and Research Centre, Dr. D.Y. Patil Vidyapeeth, Pune, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: B Nagi Reddy, UG and PG Boys Hostel, Department of Radiodiagnosis, Dr. D.Y. Patil Medical College and Research Institute, Dr. D.Y. Patil Vidyapeeth, Pune, Maharashtra, India.
E-mail: naginov211993@gmail.com
The displaced molar tooth is an unexpected and uncommon intraoperative complication of tooth extraction. Its prompt and early identification and management is crucial, as this may reduce the patient morbidity. Orthopantomogram (OPG) has limitations because of extensive anatomical superimposition of various structures. A 36-year-old female patient was referred for Computed Tomography (CT) of maxillofacial region with 3D CT scan for severe pain and swelling in right cheek region with inability to open mouth for 4 days following the dental intervention in outside dental clinic. CT scan of maxillofacial region showed bony defect in the right 3rd maxillary alveolus with multiple small bony fragments. Small fragment of molar tooth was displaced into the right infratemporal fossa and was impinging on right lateral pterygoid muscle with surrounding ill-defined soft tissue infiltrates in right retroantral fat. CT Face with 3D reconstruction helps in accurate localisation and gives appropriate anatomical detail in case of displaced molar tooth into infratemporal fossa. Thus, a detailed radiological investigation and documenting the relations of the displaced tooth or fragment with adjacent structures provides crucial information for proper surgical planning and avoiding possible complications.
Computed tomography, Intraoperative complications, Oral surgery, Trismus, Wisdom tooth
Case Report
A 36-year-old female patient was referred for CT of maxillofacial region in the Department of Radiodiagnosis for severe pain, swelling in right cheek region with inability to open mouth for four days following the dental intervention in outside dental clinic. The patient initially had dental (right maxillary 3rd molar) caries with severe pain and swelling for three months for which she took treatment from private dental practitioner on OPD basis. The swelling subsided after antibiotics and anti-inflammatory drugs. The patient was advised root canal procedure. During root canal procedure, there was fracture of tooth. During extraction of fractured tooth, there was displacement of fractured fragment. This was followed by severe throbbing pain and swelling with trismus. Clinically, patient had diffuse swelling with pain over right maxillary region. There was limitation in intraoral examination due to severe trismus. The patient was hence referred to dental department of medical college for further management.
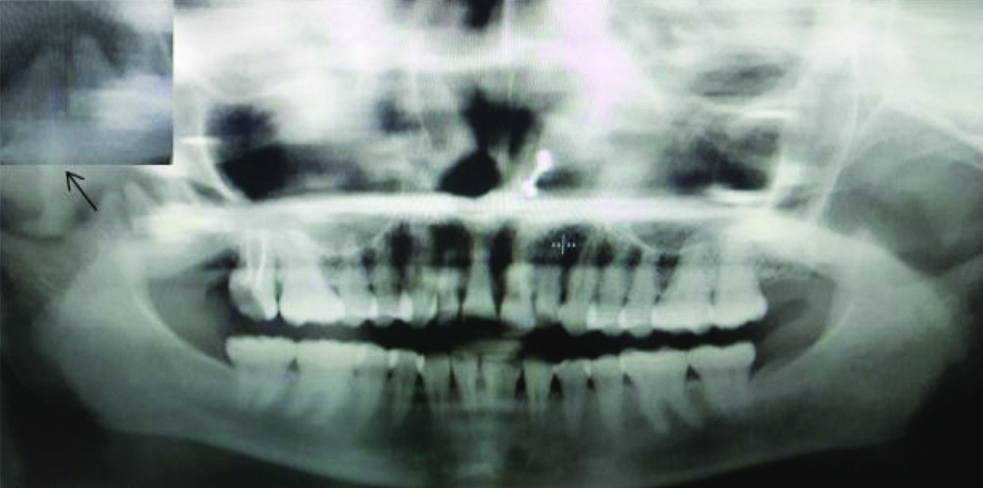
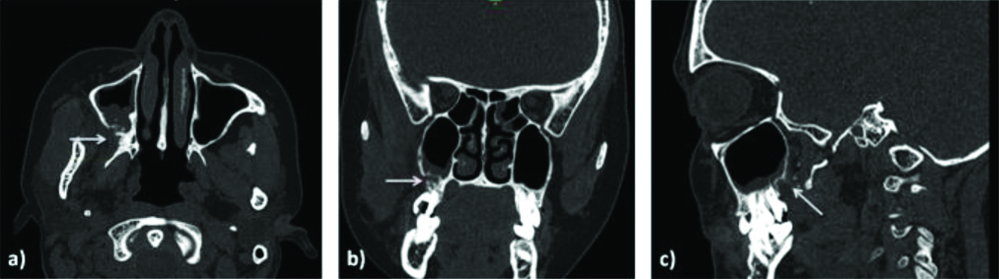
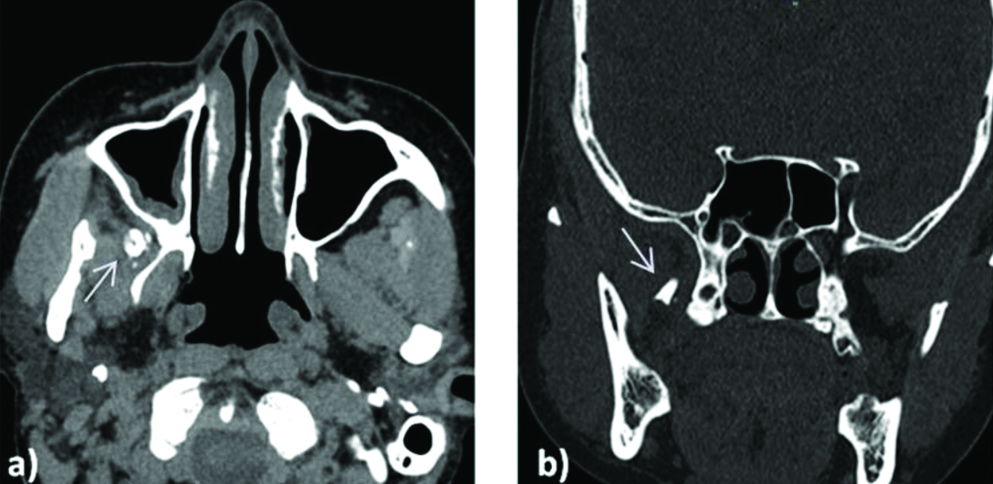
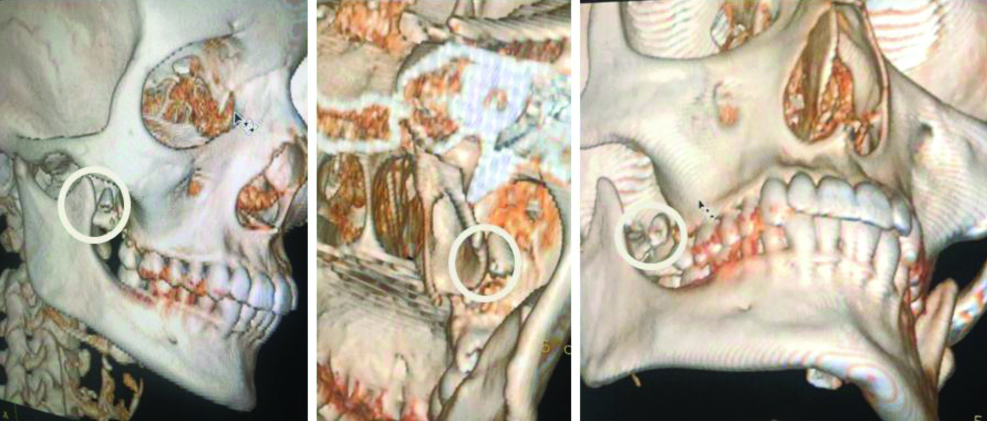
The OPG of patient [Table/Fig-1] showed a vertical root fracture of right maxillary 3rd molar with dislodged fragment of the root in the right infratemporal space. CT scan of maxillofacial region of this patient was done. On multiplanar bone windows [Table/Fig-2], bony defect was seen in the right 3rd maxillary alveolus with multiple small bony fragments. Soft tissue window [Table/Fig-3] gave details of involvement of adjacent muscles and fat planes. In this case, small fragment of molar tooth measuring approx. 6 (anteroposterior)×6 (transverse)×7 (craniocaudal) mm was displaced into the right infratemporal fossa with surrounding ill-defined soft tissue infiltrates in right retroantral fat and the fragment was impinging on right lateral pterygoid muscle. CT face 3D reconstruction [Table/Fig-4] was used for better anatomical assessment of the location of the displaced tooth fragment.
OPG showing vertical root fracture of a 3rd maxillary molar on the right side with dislodged fragment (arrow) in the right infratemporal space.
Multiplanar CT maxillofacial region at bone windows: a) axial; b) coronal; and c) sagittal images at the level of maxillary sinuses showing a bony defect in the right maxillary alveolus with multiple small bony fragments (arrows) displaced posterolaterally. Also, polypoid mucosal thickening in the right maxillary sinus.
a) CT maxillofacial region at soft tissue window in the axial plane at the level of maxillary sinuses showing ill-defined soft tissue infiltrates in retroantral region and hyperdense bony fragment (arrow) impinging on right lateral pterygoid muscle; b) CT face bone window in the coronal plane at the level of sphenoid sinus showing displaced root fragment (arrow) into right infratemporal fossa. Left infratemporal fossa and retroantral fat appear normal.
CT face 3D reconstructed images showing displaced fragment of tooth in the right infratemporal fossa (ring) and its relation to adjacent bony structures.
The patient underwent Caldwell-Luc Operation for extraction of displaced fragment of molar tooth from infratemporal fossa. Post operatively, the pain and swelling reduced with mild trismus. Patient is being followed-up in dental department. The unique feature of this case report is that part of 3rd molar tooth (root) was displaced in infratemporal fossa rather than entire tooth.
Discussion
Dental interventions like tooth extraction or root canal procedures are associated with a wide range of complications. Venkateshwar GP et al., gave a list of frequently encountered complications in the oral and maxillofacial surgery units like; tooth fracture (20.4%), fracture of cortical plate (16.2%), dry socket (alveolitis) (11.7%), trismus (18%), pain (3.9%), bleeding (1.3%), fracture of maxillary tuberosity (0.5%), infection (0.4%), fracture mandible, luxation of adjacent tooth (0.13%), displacement of tooth into adjacent tissue spaces (0.05%) and displacement of tooth into maxillary sinus (0.04%). Among which tooth root fracture, haemorrhage and trismus are most common, but perforation of maxillary sinus and displacement of tooth or fragments of tooth is very uncommon [1].
Maxillary 3rd molars are very uncommon to be displaced and only few cases of displaced molar tooth due to some surgical intervention have been reported till now in the literature, involving following anatomical spaces: lateral pharyngeal space, infratemporal fossa and pterygo mandibular space. Displacement of maxillary molar tooth can occur due to the application of extreme force, improper use of instruments, judgment error or failure of adequate visualisation prior to removal. Maxillary molar can be displaced through the adjacent periosteum into the infratemporal fossa. It is usually located lateral to lateral pterygoid plate inferior to lateral pterygoid muscle [2,3].
In such a complicated situation, clinical determination of location of displaced tooth is not possible and even basic radiographic investigation like OPG is also of no great use because of extensive anatomical superimposition of various structures which may lead to misdiagnosis. CT is essential for diagnosis and accurate localisation of the displaced tooth in infratemporal fossa [3,4].
Very less literature is available on the role of CT in displaced mandibular and maxillary molar tooth. Using multiplanar, high resolution and 3D reconstruction capabilities of the CT, the authors can easily localise the displaced tooth and adjacent soft tissue structures affected by the displaced fragment ultimately providing a route map for the surgeon for the retrieval of the tooth.
Dislodgement of maxillary molar in infratemporal fossa may lead to dangerous complications as this area consists of vital neurovascular structures like; branches of the mandibular nerve, chorda tympani, maxillary artery and pterygoid plexus of veins. Complications include: neurological injury, chronic trismus and postoperative bleeding and parapharyngeal space infection, submasseteric abscess, cervico-facial infections and life threatening ludwig’s angina [2,5].
Various surgical approaches are available for retrieval of the displaced molar tooth, but almost all of them are associated with some extent of patient morbidity in the postoperative period. These interventions may vary depending on the anatomical space into which the tooth is displaced. For infratemporal space: a) Caldwell-Luc approach; b) Gilles approach; c) long incision in the buccal sulcus are used. Molar tooth displaced into pterygopalatine fossa are usually managed conservatively by intraoral approach to prevent further displacement [4].
These surgical techniques are associated with postoperative complications like- trismus and injury to the otic ganglion. Prevention of infratemporal tooth displacement can be achieved by balanced application of force during tooth extraction and on the expertise of the surgeon [6].
Previous cases reported in the literature showed displacement of entire 3rd molar into the infratemporal fossa [Table/Fig-5] [4,7-22]. In this case, part of 3rd molar tooth (root) was displaced in infratemporal fossa rather than the entire tooth.
Tabulated form of comprehensive review of literature about cases of displaced 3rd maxillary molar tooth into infratemporal fossa and associated clinical symptoms [4,7-22].
| S. No. | Authors | Year | Age (years) | Sex | Symptoms and signs | Part of 3rd maxillary molar displaced |
|---|
| 1. | Oberman M et al., [7] | 1986 | 26 | Female | Not reported | Entire tooth |
| 2. | Dawson K et al., [8] | 1993 | 18 | Female | None | Entire tooth |
| 3. | Patel M and Down K [9] | 1994 | 19 | Female | Not reported | Entire tooth |
| 4. | Orr DL [10] | 1999 | 16 | Male | Not reported | Entire tooth |
| 5. | Sverzut CE et al., [11] | 2009 | 22 | Male | Limited mouth opening, pain during mandibular movements | Entire tooth |
| 6. | Campbell A and Costello BJ [12] | 2010 | 18 | Female | Diplopia on upward eye movement | Entire tooth |
| 7. | Gómez-Oliveira G et al., [13] | 2010 | 23 | Female | None | Entire tooth |
| 8. | Borgonovo A et al., [14] | 2010 | 35 | Female | Presented with displaced tooth | Entire tooth |
| 9. | Selvi F et al., [15] | 2011 | 35 | Male | None | Entire tooth |
| 10. | Baig MH et al., [16] | 2012 | 24 | Male | Pain, oedema | Entire tooth |
| 11. | Bodner L et al., [17] | 2012 | 34 | Male | Presented with displaced tooth | Entire tooth |
| 12. | Condal CD et al., [18] | 2012 | 42 | Female | Limited mouth opening, pain | Entire tooth |
| 13. | Corega C et al., [19] | 2013 | 24 | Male | Limited mouth opening, pain | Entire tooth |
| 14. | Özer N et al., [4] | 2013 | 23 | Female | Oedema, limited mouth opening | Entire tooth |
| 15. | Primo BT et al., [20] | 2014 | 14 | Female | None | Entire tooth |
| 16. | Roshanghias K et al., [21] | 2016 | 14 | Not mentioned | Presented with displaced tooth | Entire tooth |
| 17. | Lutz JC et al., [22] | 2019 | 17 | Female | Presented with displaced tooth | Entire tooth |
| 18 | Present study | 2020 | 36 | Female | Trismus, swelling | Root |
Conclusion(s)
The maxillary tuberosity is vulnerable to fractures due to trabecular pattern with resultant risk of displacement into adjacent anatomical sites. CT Face with 3D reconstruction helps in the diagnosis and accurate localisation of the displaced molar tooth into infratemporal fossa. This helps in proper surgical planning and avoiding possible complications.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 10, 2020
Manual Googling: Sep 16, 2020
iThenticate Software: Oct 20, 2020 (3%)
[1]. Venkateshwar GP, Padhye MN, Khosla AR, Kakkar ST, Complications of exodontia: A retrospective studyIndian Journal of Dental Research 2011 22(5):63310.4103/0970-9290.9344722406704 [Google Scholar] [CrossRef] [PubMed]
[2]. Bansal P, Rohatgi S, Sheokand N, Skillful management of exodontia complication to prevent dreadful sequelaeJ Clin Exp Dent 2011 3(4):e340-42.10.4317/jced.3.e340 [Google Scholar] [CrossRef]
[3]. Kocaelli H, Balcioglu HA, Erdem TL, Displacement of a maxillary third molar into the buccal space: Anatomical implications apropos of a caseInternational Journal of Oral and Maxillofacial Surgery 2011 40(6):650-53.10.1016/j.ijom.2010.11.02121211942 [Google Scholar] [CrossRef] [PubMed]
[4]. Özer N, Üçem F, Saruhanoğlu A, Yilmaz S, Tanyeri H, Removal of a maxillary third molar displaced into pterygopalatine fossa via intraoral approachCase Reports in Dentistry 2013 2013:39214810.1155/2013/39214823476814 [Google Scholar] [CrossRef] [PubMed]
[5]. Di Nardo D, Mazzucchi G, Lollobrigida M, Passariello C, Guarnieri R, Galli M, Immediate or delayed retrieval of the displaced third molar: A reviewJournal of Clinical and Experimental Dentistry 2019 11(1):e5510.4317/jced.5537930697395 [Google Scholar] [CrossRef] [PubMed]
[6]. Kim JH, Lim SU, Jin KS, Lee H, Han YS, The postoperative trismus, nerve injury and secondary angle formation after partial masseter muscle resection combined with mandibular angle reduction: A case reportJournal of the Korean Association of Oral and Maxillofacial Surgeons 2017 43(1):46-48.10.5125/jkaoms.2017.43.1.4628280710 [Google Scholar] [CrossRef] [PubMed]
[7]. Oberman M, Horowitz I, Ramon Y, Accidental displacement of impacted maxillary third molarsInternational Journal of Oral and Maxillofacial Surgery 1986 15(6):756-58.10.1016/S0300-9785(86)80118-1 [Google Scholar] [CrossRef]
[8]. Dawson K, MacMillan A, Wiesenfeld D, Removal of a maxillary third molar from the infratemporal fossa by a temporal approach and the aid of image-intensifying cineradiographyJournal of Oral and Maxillofacial Surgery 1993 51(12):1395-97.10.1016/S0278-2391(10)80149-1 [Google Scholar] [CrossRef]
[9]. Patel M, Down K, Accidental displacement of impacted maxillary third molarsBritish Dental Journal 1994 177(2):57-59.10.1038/sj.bdj.48085078060710 [Google Scholar] [CrossRef] [PubMed]
[10]. Orr DL, A technique for recovery of a third molar from the infratemporal fossa: Case reportJournal of Oral and Maxillofacial Surgery 1999 57(12):1459-61.10.1016/S0278-2391(99)90733-4 [Google Scholar] [CrossRef]
[11]. Sverzut CE, Trivellato AE, Sverzut AT, de Matos FP, Kato RB, Removal of a maxillary third molar accidentally displaced into the infratemporal fossa via intraoral approach under local anesthesia: Report of a caseJournal of Oral and Maxillofacial Surgery 2009 67(6):1316-20.10.1016/j.joms.2008.09.01819446223 [Google Scholar] [CrossRef] [PubMed]
[12]. Campbell A, Costello BJ, Retrieval of a displaced third molar using navigation and active image guidanceJournal of Oral and Maxillofacial Surgery 2010 68(2):480-85.10.1016/j.joms.2009.06.03220116728 [Google Scholar] [CrossRef] [PubMed]
[13]. Gómez-Oliveira G, Arribas-García I, Álvarez-Flores M, Gregoire-Ferriol J, Martínez-Gimeno C, Delayed removal of a maxillary third molar from the infratemporal fossaMed Oral Patol Oral Cir Bucal 2010 15(3):e509-11.10.4317/medoral.15.e50920038889 [Google Scholar] [CrossRef] [PubMed]
[14]. Borgonovo A, Grossi GB, Maiorana C, Santoro F, Cicciù M, Management of the upper third molar displaced in the infratemporal fossa: A case reportInt J Clin Dent 2010 3(4):301-08. [Google Scholar]
[15]. Selvi F, Cakarer S, Keskin C, Ozyuvaci H, Delayed removal of a maxillary third molar accidentally displaced into the infratemporal fossaJournal of Craniofacial Surgery 2011 22(4):1391-93.10.1097/SCS.0b013e31821cc25421772176 [Google Scholar] [CrossRef] [PubMed]
[16]. Baig MH, Punjabi SK, Khan M, Displacement of maxillary third molar in the infra-temporal fossaPakistan Oral and Dental Journal 2012 32(1) [Google Scholar]
[17]. Bodner L, Joshua BZ, Puterman MB, Removal of a maxillary third molar from the infratemporal fossaJournal of Medical Cases 2012 3(2):97-99.10.4021/jmc455w [Google Scholar] [CrossRef]
[18]. Condal CD, Sánchez RR, García CG, Eliminaciónquirúrgica de tercer molar maxilardesde la fosa infratemporal, por Trismus severoActaodontológicavenezolana 2012 50(3):25-26. [Google Scholar]
[19]. Corega C, Vaida L, Festila D, Bertossi D, Unusual anatomical detection of a third molar in the infratemporal fossaChirurgia (Bucur) 2013 108(6):907-09. [Google Scholar]
[20]. Primo BT, Stringhini DJ, Klüppel LE, Da Costa DJ, Rebellato NL, de Moraes RS, Delayed removal of maxillary third molar displaced into the infratemporal fossaRevista Española de Cirugía Oral y Maxilofacial 2014 36(2):78-81.10.1016/j.maxilo.2012.05.012 [Google Scholar] [CrossRef]
[21]. Roshanghias K, Peisker A, Zieron JO, Maxillary tooth displacement in the infratemporal fossaDental Research Journal 2016 13(4):37310.4103/1735-3327.18788127605997 [Google Scholar] [CrossRef] [PubMed]
[22]. Lutz JC, Cazzato RL, Le Roux MK, Bornert F, Retrieving a displaced third molar from the infratemporal fossa: Case report of a minimally invasive procedureBMC Oral Health 2019 19(1):14910.1186/s12903-019-0852-z31307439 [Google Scholar] [CrossRef] [PubMed]