Case Report
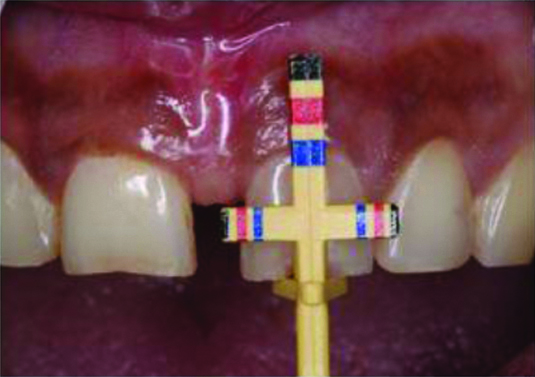
A 30-year-old female patient reported to the Department of Conservative Dentistry and Endodontics, Bapuji Dental College and Hospital with a complaint of gap in upper front teeth. Patient’s oral hygiene was satisfactory and had no contributory medical history [Table/Fig-1].

The clinical examination revealed a maxillary anterior diastema of 4 mm between the central incisors 11 and 21 with a healthy gingiva and no hard tissue pathology. The presence of gingival type of labial frenum attachment was detected [Table/Fig-2]. Probing pocket depth was less than 3 mm with absence of gingival recession. No aesthetic problem was evident in mandibular anterior teeth.
Pre-operative labial view- high frenal attachment.

The option of comprehensive orthodontic treatment and multiple ceramic veneers (six teeth) was offered to the patient but was rejected due to time and economic considerations. Therefore, a multidisciplinary treatment plan was designed to address the patient’s concerns that included labial frenectomy, crown lengthening and porcelain laminate veneers for the upper two maxillary central incisors for diastema closure.
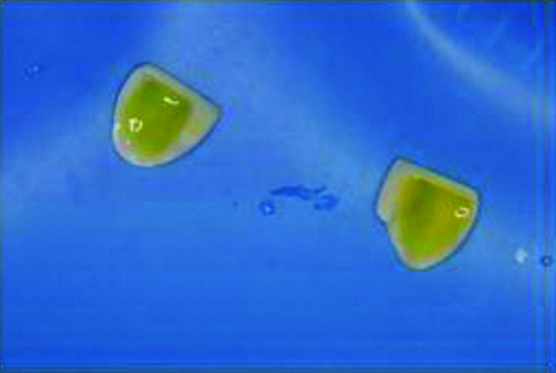
Following oral prophylaxis, the area was anaesthetised utilising local infiltration technique with 2% lignocaine with 1:80000 adrenaline. After which, a haemostat was used to engage the labial frenum and inserted into the depth of the vestibule. Furthermore, incisions were placed using Scalpel No. 15 on the upper and the under surface of the haemostat until the haemostat was free. Using the haemostat, the triangular resected portion of the frenum was removed [Table/Fig-3].

The fibrous attachment was relieved by blunt dissection along the bone. The edges of the wound were sutured using interrupted sutures (4-0 black silk) and covered with a periodontal pack [Table/Fig-4].

The periodontal pack and sutures were removed one week post-operatively. The post-operative sequelae at one month of follow-up included labial tissue scarring.
Surgical Crown Lengthening using Chu’s Gauge
After the frenectomy and healing of the tissues, patient was recalled after four weeks to assess for the crown lengthening procedure. On examination, the width of the attached gingiva was 4 mm and the periodontal pockets were less than 3 mm. Bone sounding was performed to rule out the necessity for any osseous surgery. The case was classified as a Type 1 crown lengthening procedure with adequate width of keratinised tissues without any biologic width violation according to the classification system proposed by Lee EA [1].
The incisal stop of the Chu’s proportion gauge was rested on the incisal edge of the tooth. The colour coded band on the horizontal arm corresponded to the colour coded band on the vertical arm. The red band stood for the length and width of the central incisors, blue for lateral incisors and yellow for canines. If the colour coded bands do not match with existing tooth proportions, a diagnosis of width to length discrepancy can be concluded [1]. Chu’s gauge was placed individually on the maxillary central incisors to assess the correct length of the tooth and plan for the amount of crown lengthening necessary according to the tooth proportions for a pleasant final outcome. The length of maxillary central incisors was measured to be 8.5 mm and a crown lengthening of 3 mm was required to achieve the correct tooth proportions.
Using the Chu’s proportion gauge (Hu-Friedy Inc, Chicago, IL®), bleeding points were established using pocket markers so as to establish reference points for the external bevel incision. Using the Kirkland gingivectomy knife, the incision was placed from the attached gingiva to a level just apical to the pocket markings. Orban’s interdental knife was used to complete the interdental incision [Table/Fig-5,6].
CHU’s Gauge for Crown lengthening.
Immediately after Crown lengthening.
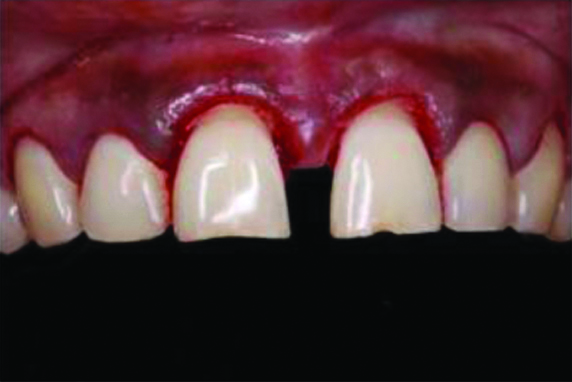
Following the surgical completion, periodontal dressing was packed (Coe-Pak, GC America Inc®) and the patient was recalled after one week. [Table/Fig-7] shows post-operative view after four weeks of crown lengthening.
Post-operative after four weeks.

Tooth Surface Reduction
Shade selection was done at the beginning of the appointment [Table/Fig-8]. Horizontal cuts were made using Aesthetic Pre-Evaluative Temporary (APT) technique with a depth cutter bur (0.5 mm-Shofu porcelain veneer kit®) by moving it across the labial surface from mesial to distal over the temporaries in three different orientations to develop three evenly spaced grooves cervically, mid-facially and incisally.

The grooves were pinpointed with a pencil to allow for a better visualisation of preparation [Table/Fig-9].

The maxillary central incisors were prepared for lithium disilicate laminate veneers with a 0.5-mm chamfer at the gingival margin, 0.7-mm facial reduction and an incisal butt joint with 1 mm reduction using a two grit diamond bur. The reduction was then, extended interproximally creating wrap around effect so that the proximal finish line is palatal and is not visible during diastema closure. The cervical chamfer margin finish line was equigingival in order to preserve the gingival health, facilitate cleaning and allow for an adequate bonding. Finally, all the preparation margins were rounded to reduce stress concentration [Table/Fig-10].

At the same appointment, the impression was made using vinyl polysiloxane addition silicone (3 M ESPE®). Gingival tissue management was done with double cord displacement technique using two retraction cord (#000 and #00, Ultradent®). The retraction cords were removed and the impression was made with a stock tray with a two-step double mix impression technique [Table/Fig-11].
Dual impression (Putty and light body).

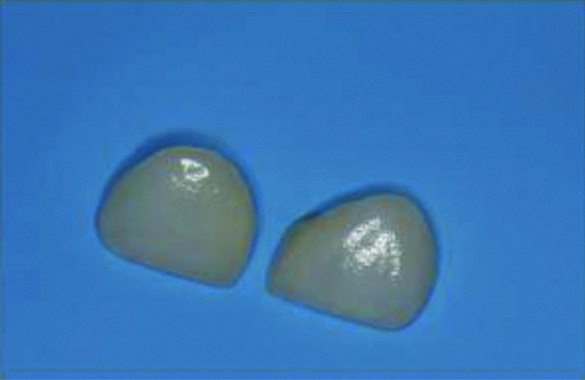
The impression was then, disinfected with 2% glutaraldehyde solution (3 M India®) and sent to the laboratory for fabrication of lithium disilicate veneers (E-max, Dent care, Kerala®) along with the shade and intraoral photographs.
Provisional restoration was done using putty index along with temporization material (ProTemp Plus, 3 M ESPE®). The provisionals were finished and luted to the preparation after spot etching.
Isolation and Cementation
Once the lithium disilicate veneers were obtained from the laboratory, the provisionals were removed and the surface was cleaned with pumice to remove any remnants of provisional luting cement [Table/Fig-12]. First, the veneers were tried intraorally to evaluate the fit, position, shade and patient satisfaction. Isolation was done using Rubber dam (Heavy 6x 6’’Sanctuary dam sheets®,) (Brinker clamp B4, Coltene®) from #13 to #23 [Table/Fig-13] and Teflon tape (M seal®, India) was placed to protect the adjacent teeth from inadvertent etching and bonding procedures.

The teeth surfaces of both the maxillary central incisors were etched with 37% phosphoric acid (Etchant gel, prime dent®) for 20 seconds and rinsed with water followed by drying [Table/Fig-14]. The internal surfaces of the veneers were etched with 9.5% hydrofluoric acid for 20 seconds (Porcelain Etch, Ultradent Products, Provoh, UT, USA®). The surfaces were then, washed with water and silanised with a silane coupling agent (Ultradent, Provoh, UT, USA®) for one minute and then, allowed to dry which was followed by application of bonding agent [Table/Fig-15]. (Scotchbond Universal Etchant, 3M ESPE®).
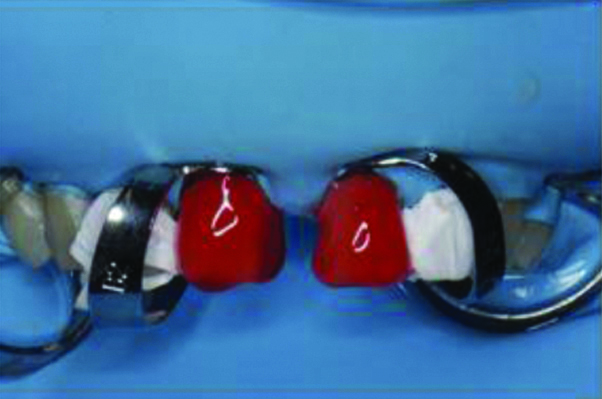
Hydrofluoric acid etching on veneer.
A thin layer of Single Bond Universal (3M ESPE®) was applied on the teeth using applicator tip for 20 seconds followed by mild air drying for five seconds. Veneers were then luted simultaneously over the maxillary incisors using Rely X Veneer cement (3 M ESPE®) Light curing was done for two-three seconds [Table/Fig-16].

Then, the restorations were flossed to remove excess cement from the interproximal area and the final polymerisation was completed [Table/Fig-17].

[Table/Fig-18] shows post-operative smile of the patient after one week. Informed consent was taken from the patient for the use of photographs for the purpose of case presentation and documentation.
Post-operative smile after one week.

Follow-up
The case was kept under follow-up for one year for assessment of gingival healing and aesthetic rehabilitation [Table/Fig-19].
Post-operative follow-up after one year.

Discussion
Treatment of a large maxillary midline diastema often presents with soft tissue challenges. Space can be normally present during the mixed dentition period and generally closes with the eruption of permanent maxillary canines [2]. However for few individuals, the diastema does not close spontaneously. A combined periodontal and restorative approach is necessary to analyse and solve the aesthetic problem. Hence in the present case, the initial intervention was the excision of the labial frenal tissue as it interfered with crown lengthening and restorative procedure and is similar to the treatment plan employed by Calamia V et al., which included periodontal modification of the gingival architecture, maxillary frenectomy, and feldspathic porcelain veneers [3]. To prevent relapse of the diastema, the intrusive maxillary frenum must be removed along with the reticular fibres [2,3]. Similar treatment was performed by Maluly-Proni AT et al., to close the midline diastema of 1.5 mm between maxillary central incisors using conservative and aesthetic option of ceramic veneers [4].
In clinical situations where the teeth exhibit short clinical crowns, it is often necessary to perform the crown lengthening either apically by periodontal surgery, incisally with the addition of restorative material or by a combination procedure for maintaining ideal tooth proportion and harmony [4,5]. Without the crown lengthening procedure, the teeth would seem squarish and unaesthetic [5]. The use of Chu’s aesthetic gauge is employed for biologic increase in crown length and provide a guide for gingival and bone tissue removal, ultimately producing a restoration compatible with the periodontium [6]. This is in contrast to the technique employed by Calamia V et al., and Cosenza H et al., where wax up was made to analyse the golden proportion [3,7].
The gingivectomy technique produces satisfactory results in cases presenting with excessive gingival tissue without need of bone remodeling interventions [7]. This procedure enables the exposure of hidden enamel under gingival tissue as well as create a harmonious gingival architecture [7,8]. Gingivectomy and frenectomy procedures create an oral aesthetic balance between teeth and gingiva in achieving a pleasant smile [8].
In the present case, Aesthetic Pre-Evaluative Temporary (APT) technique was used and enabled the patient to judge the final restorative design before the provisional restoration had been made. APT leads to predictable aesthetic outcome and no under or over preparations of the teeth thus, ensuring minimally invasive tooth preparation within enamel [9]. Therefore, the advantages of APT technique include foreseeable aesthetics, optimal occlusion and phonetics [9,10]. The margin placement of the restorations was equigingival to ensure good periodontal health. In addition, the cervical end was located on enamel thus, ensuring maximum bonding and clinical longevity [10].
The longevity of ceramic veneers is determined by the strength and durability of the bond between the tooth, veneer and luting cement [9,10]. In the present case, lithium disilicate veneers were fabricated of thickness 0.3 to 0.5 mm. Lithium disilicate veneers exhibit high wear resistance and optimum optical properties [10]. The adhesive procedure was according to the recommended protocol under strict rubber dam isolation. In addition, the use of light cured cement (Rely X Veneer cement) was chosen due to its high colour stability and adequate working time [11].
Porcelain laminate veneers are commonly indicated for diastema closures as they allow minimally invasive tooth preparation with optimal aesthetic outcome. The other advantages include resistance to discolouration and surface degradation in comparison to resin composites [12]. The final aesthetic outcome is dependent on a successful collaboration among the team members beginning with the diagnostic phase in order to achieve both the aesthetic and functional parameters [13].
The patient presented with a 4 mm wide diastema between the central incisors which was corrected without any orthodontic intervention. Wider diastema closures often necessitate an orthodontic approach [12,13]. However, owing to the lack of time and cost factor, the patient was not compliant for the same. Hence, an interdisciplinary treatment approach was adopted in which the proposed tooth proportion was combined with periodontal aesthetic procedure to achieve near-ideal results which were satisfactorily achieved. Perio-restorative approach has been reported in the literature for anterior aesthetic rehabilitation [13]. However, to the best of our knowledge, no other case report has emphasised its importance in management of wide diastemas and as a substitute for orthodontic treatment.
Conclusion(s)
An optimum aesthetic and functional outcome of a severe maxillary midline diastema can be achieved with a multidisciplinary approach. The case was managed with a combination of periodontal (gingivectomy and frenectomy) and restorative procedures. Patient was satisfied with the results and the final aesthetic appearance. Rehabilitation with ceramic veneers allowed for a predictable minimally invasive approach. A comprehensive treatment planning combined with the correct selection of dental materials and adhesive technique resulted in a successful treatment outcome.
[1]. Lee EA, Aesthetic crown lengthening: Classification, biologic rationale, and treatment planning considerationsPract Proced Aesthet Dent 2004 16(10):769-80. [Google Scholar]
[2]. Huang WJ, Creath CJ, The midline diastema: A review of its etiology and treatmentPediatr Dent 1995 17(3):171-79. [Google Scholar]
[3]. Calamia V, Pantzis A, Simple case treatment planning: Diastema closureDent Clin North Am 2015 59(3):655-64.10.1016/j.cden.2015.03.01026140972 [Google Scholar] [CrossRef] [PubMed]
[4]. Maluly-Proni AT, Oliveira-Reis B, Assunção WG, Santos PHD, Minimum intervention management of diastema closure using cordless displacement system and laminate veneers: A 2-year follow-upEur J Dent 2018 12(3):446-49.10.4103/ejd.ejd_208_1830147415 [Google Scholar] [CrossRef] [PubMed]
[5]. Fletcher P, Biologic rationale of esthetic crown lengthening using innovative proportion gaugesInt J Periodontics Restorative Dent 2011 31(5):523-32. [Google Scholar]
[6]. Nautiyal A, Gujjari S, Kumar V, Aesthetic crown lengthening using chu aesthetic gauges and evaluation of biologic width healingJ Clin Diagn Res 2016 10(1):ZC51-ZC55.10.7860/JCDR/2016/14115.711026894176 [Google Scholar] [CrossRef] [PubMed]
[7]. Cosenza H, Pamato S, Vermudt A, Pereira JR, Interdisciplinary approach using composite resin and ceramic veneers to manage an esthetic challengeJ Prosthet Dent 2020 :S0022-3913(20)30081-0 [Google Scholar]
[8]. Şen N, Işler S, Multidisciplinary management of a severe maxillary midline diastema: A clinical reportJ Prosthodont 2019 28(3):239-43.10.1111/jopr.1297930350325 [Google Scholar] [CrossRef] [PubMed]
[9]. Soares PV, Spini PH, Carvalho VF, Souza PG, Gonzaga RC, Tolentino AB, Esthetic rehabilitation with laminated ceramic veneers reinforced by lithium disilicateQuintessence Int 2014 45(2):129-33. [Google Scholar]
[10]. Wolff D, Kraus T, Schach C, Pritsch M, Mente J, Staehle HJ, Recontouring teeth and closing diastemas with direct composite buildups: A clinical evaluation of survival and quality parametersJ Dent 2010 38:1001-09.10.1016/j.jdent.2010.08.01720826192 [Google Scholar] [CrossRef] [PubMed]
[11]. Heymann HO, Hershey HG, Use of composite resin for restorative and orthodontic correction of anterior interdental spacingJ Prosthet Dent 1985 53:766-71.10.1016/0022-3913(85)90153-2 [Google Scholar] [CrossRef]
[12]. Furuse AY, Franco EJ, Mondelli J, Esthetic and functional restoration for an anterior open occlusal relationship with multiple diastemata: A multidisciplinary approachJ Prosthet Dent 2008 99:91-94.10.1016/S0022-3913(08)60023-2 [Google Scholar] [CrossRef]
[13]. Horn HR, Porcelain laminate veneers bonded to etched enamelDent Clin North Am 1983 27(4):671-84. [Google Scholar]