Intra-abdominal Abscesses by Burkholderia cepacia in Poorly Controlled Diabetes Mellitus: A Case Series
Aditya Dhanawat1, Partisha Gupta2, Lalatendu Mohanty3, Guncha Maheshwari4
1 PG Resident, Department of Internal Medicine, Kalinga Institute of Medical Sciences, Bhubaneswar, India.
2 PG Resident, Department of Internal Medicine, Kalinga Institute of Medical Sciences, Bhubaneswar, India.
3 Professor, Department of Internal Medicine, Kalinga Institute of Medical Sciences, Bhubaneswar, India.
4 PG Resident, Department of Radiation Oncology, Sardar Patel Medical College, Bikaner, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Lalatendu Mohanty, Professor, Department of Internal Medicine, Kalinga Institute of Medical Sciences, Bhubaneswar, India.
E-mail: lalatendumohanty3@gmail.com
Burkholderia is a gram-negative bacillus causing infections in immunocompromised patients. It is commonly seen in the tropics and is known to mimic tuberculosis clinically. Six patients were reviewed who were admitted in our hospital between July 2018 to June 2019 after obtaining their consent. All the six patients were uncontrolled diabetics with HbA1c levels between 8.2-13.9% who presented with fever more than 2 weeks and had abdominal symptoms like vomiting, abdominal pain or loss of appetite. Some also had respiratory symptoms like cough, chest pain and breathlessness. All of them had leucocytosis (neutrophilic). Mild transaminitis was also observed. CT abdomen revealed presence of multiple hepatic and splenic abscesses in all the patients. Chest X-ray revealed bilateral pneumonia in five patients. Burkholderia cepacia was found in the blood of four patients, sputum of one patient and splenic pus aspirate of one patient. Four patients were treated with meropenem and rest with ceftazidime. All of them responded well to treatment and became asymptomatic. Ultrasonography abdomen at follow-up was negative for any intra-abdominal abscesses. They were also put on long term oral co-trimoxazole. The clinical presentation of Burkholderia closely mimics tuberculosis as it predominantly affects immunocompromised and causes a long-duration multi-systemic illness. There has been several case series of intra-abdominal abscesses caused by Burkholderia pseudomallei but infections by Burkholderia cepacia in the abdomen is a rare finding. The diagnosis of burkholderia is often delayed due to its inconspicuous nature, lack of clinical suspicion and often mimicking tuberculosis clinically.
Immunocompromised, Splenic abscess, Tropical, Tuberculosis
Introduction
Burkholderia Cepacia Complex (BCC) is an opportunistic nosocomial pathogen which causes mild to severe illness in immunocompromised patients. They are known to cause respiratory tract infections, bacteremia, septic arthritis and peritonitis. Burkholderia infection mimics tuberculosis closely due to similar clinical profile and long-standing symptoms especially in endemic regions of the world. The authors reported a series of six cases [Table/Fig-1], who were immunocompromised (uncontrolled diabetes mellitus), with no prior history of hospitalisation in 90 days and were found to have intra-abdominal abscesses caused by Burkholderia cepacia.
Comparison between the cases in the present case series. HbA1c: Glycated Haemoglobin
| Parameters | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 |
|---|
| Age (years) | 49 | 62 | 40 | 45 | 32 | 52 |
| Sex | Male | Male | Female | Male | Male | Male |
| HbA1c | 13.9% | 12.4% | 9.3% | 8.2% | 10.5% | 10.5% |
| Duration of fever (days) | 14 | 15 | 30 | 30 | 18 | 30 |
| Site of culture specimen | Blood | Pus | Blood | Blood | Sputum | Blood |
| Diagnosis | Hepatic and Splenic abscess with right lower lobe pneumonia | Splenic abscess with bilateral pneumonia | Hepatic and Splenic abscess with left lower lobe pneumonia | Hepatic and Splenic abscess with left upper lobe cavity | Splenic abscess with left lower lobe cavity | Hepatic and Splenic abscess |
| Treatment | Meropenem + Co-trimoxazole | Meropenem + Co-trimoxazole | Meropenem + Co-trimoxazole | Meropenem + Co-trimoxazole | Ceftazidime + Co-trimoxazole | Ceftazidime + Co-trimoxazole |
| Follow-up (days) | 15 | 30 | 15 | 30 | 15 | 15 |
Case 1
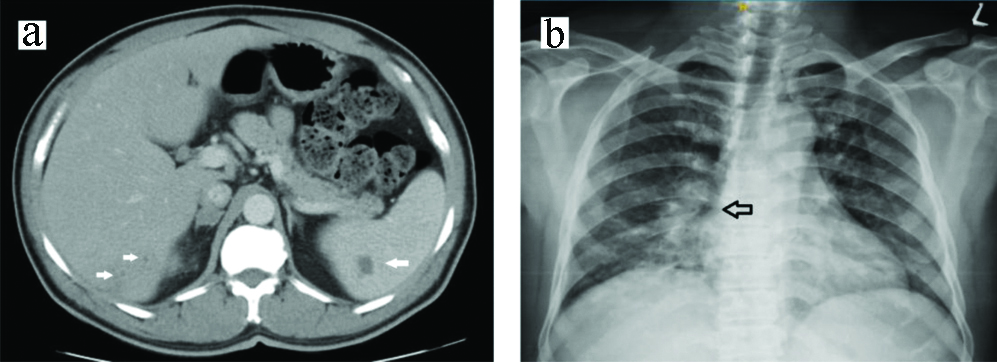
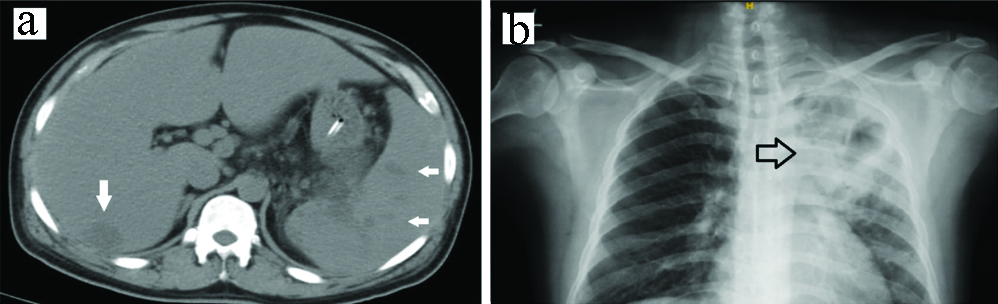
A 49-year-old diabetic male was admitted with high grade fever with chills and rigours for 14 days, dry cough for 10 days and pain in right upper abdomen for 10 days which was associated with anorexia and nausea/vomiting. Medication history revealed glimepiride 1 mg, metformin 500 mg and insulin glargine 20 IU per day. On examination, pulse was 124/min, Blood Pressure (BP) was 100/74 mm Hg, respiratory rate was 22/min and oral temperature was 101.4°F. Chest examination revealed presence of crackles in right interscapular and infrascapular region. Abdominal examination revealed tender right hypochondrium and epigastrium and there was no palpable organomegaly or free fluid in the abdomen. Investigations revealed leucocytosis (neutrophilic) and normal kidney function. Serum bilirubin of 1.52 mg/dL, Aspartate Aminotransferase (AST) of 53 U/L, Alanine Transaminase (ALT) of 137 U/L, Alkaline Phosphatase (ALP) of 382 U/L and Glycated Haemoglobin (HbA1c) was 13.9%. Chest X-ray revealed right lower lobe pneumonia. Ultrasonography of abdomen revealed evolving liver and splenic abscess which was confirmed by Computerized Tomography (CT) abdomen [Table/Fig-2]. Blood culture was done using Automated Blood Culture System (BACTEC). Antibiotic sensitivity was obtained by disc diffusion NCCLS (Clinical and Laboratory Standards Institute) method [1]. Blood culture was positive for Burkholderia cepacia which was sensitive to meropenem [Table/Fig-3]. The patient was given meropenem 1 g intravenous thrice daily for 10 days following which he was discharged with oral trimethoprim 160 mg and sulfamethoxazole 800 mg to be taken thrice daily for 6 months. The patient was followed-up after 15 days and was found to be afebrile. Repeat ultrasonography abdomen was negative for liver and splenic abscess.
Case 2
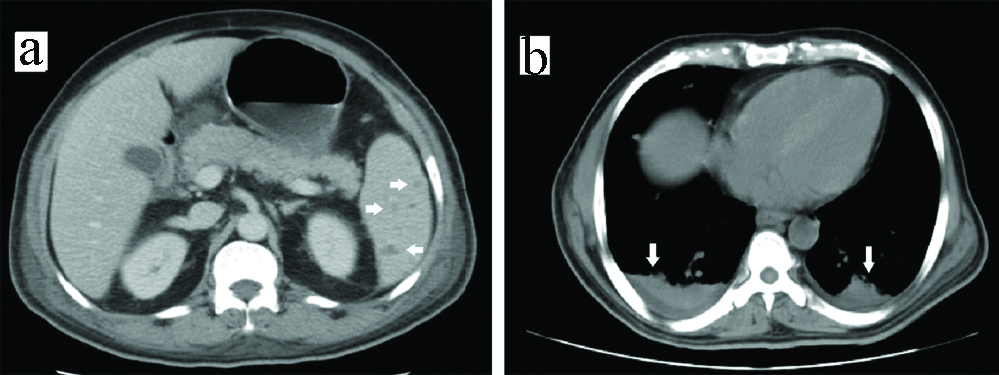
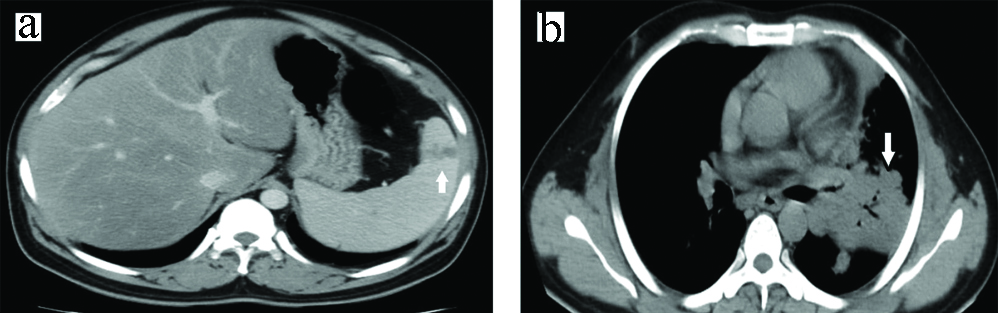
A 62-year-old diabetic male was admitted with high grade fever for 15 days, diffuse abdominal pain and 3-4 episodes of vomiting for 3 days. There was no history of diarrhoea or constipation. Medication history revealed that the patient was on regular insulin 12 U thrice daily and metformin 500 mg twice daily. On examination, pulse was 132/min, BP was 116/70 mm Hg, respiratory rate was 26/min and oral temperature was 102.6°F. Chest examination revealed presence of crackles in bilateral infra-scapular area. Abdominal examination revealed tenderness in left hypochondrium but there was no organomegaly or free fluid in abdomen. Investigations revealed leucocytosis (neutrophilic). Kidney function was normal. Serum bilirubin was 3.78 mg/dL. AST was 18 U/L and ALT was 72 U/L. HbA1c was 12.4%. CT chest was suggestive of bilateral consolidation with pleural effusion. CT abdomen showed features suggestive of multiple splenic abscesses [Table/Fig-4]. Ultrasonography guided aspiration of pus from the splenic abscess revealed Burkholderia cepacia which was sensitive to meropenem. The patient was given meropenem 1 g intravenous thrice daily for 10 days and discharged with oral trimethoprim 160 mg and sulfomethoxazole 800 mg thrice daily for 6 months. The patient was followed-up after one month and was found afebrile with normal ultrasonography of abdomen.
CT abdomen (a) showing hepatic and splenic abscesses; Chest X-ray (b) showing right lower lobe pneumonia.
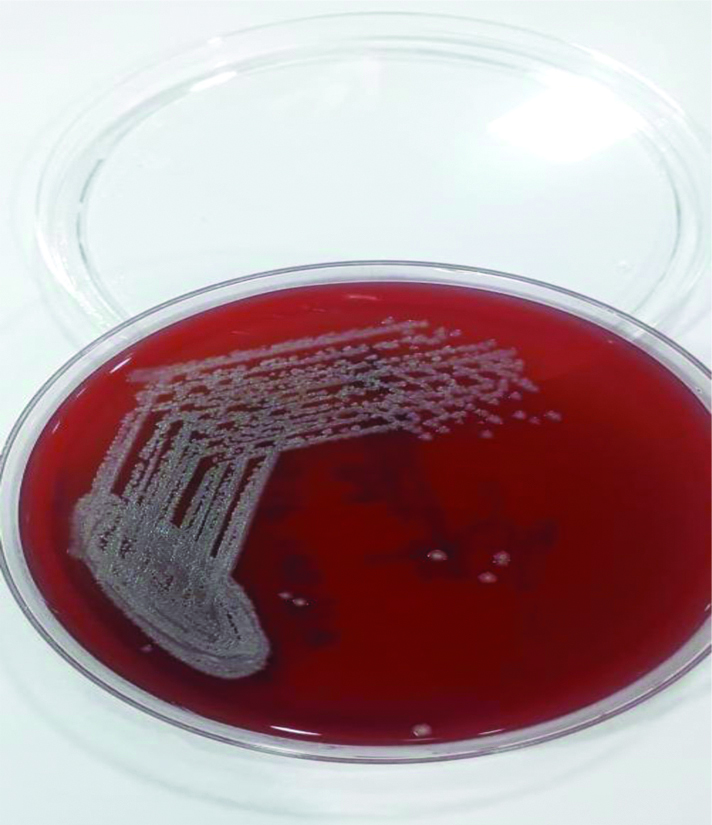
Burkholderia cepacia colonies on blood agar.
CT abdomen (a) showing multiple splenic abscesses; CT thorax (b) showing bilateral consolidation and pleural effusion.
Case 3
A 40-year-old diabetic female was admitted with complaints of fever with chills and rigour for 1 month, cough with expectoration for 1 month, multiple episodes of vomiting for 5 days and breathlessness for 3 days. She was on glimepiride 2 mg and metformin 1000 mg once daily. On examination, pulse was 110/min, BP was 132/84 mm Hg, respiratory rate was 28/min and oral temperature was 101°F. Chest examination revealed presence of crackles in left infrascapular and infra-axillary region. Abdominal examination revealed tenderness in left hypochondrium and splenomegaly. Investigations revealed normal CBC and kidney function. Serum bilirubin was 0.76 mg/dL, AST of 1499 U/L and ALT of 593 U/L. HbA1c was 9.3%. CT abdomen revealed hepatic and splenic abscesses and mild ascites [Table/Fig-5]. Blood culture was positive for Burkholderia cepacia which was sensitive to meropenem. The patient was given 10 days of meropenem 1 g intravenous thrice daily and discharged with oral medication of trimethoprim 160 mg and sulfamethoxazole 800 mg thrice daily for 6 months. She was followed-up after 15 days and found to be afebrile with normal ultrasonography of abdomen.
CT abdomen (a) showing multiple hepatic and splenic abscesses. Chest X-ray; (b) showing consolidation in left lower lobe.
Case 4
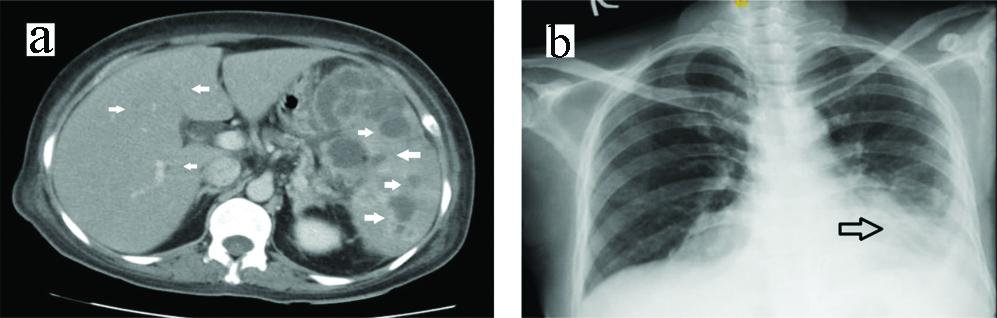
A 45-year-old diabetic male was admitted with complaints of high-grade fever with chills and rigours for one month diffuse pain abdomen for 15 days and cough with expectoration for 15 days. Medication history revealed that he was on gliclazide 80 mg and metformin 500 mg once daily. On examination, pulse was 120/min, BP was 98/64 mm Hg, respiratory rate was 22/min and oral temperature was 101.6°F. Chest examination revealed crackles in the left suprascapular, interscapular and axillary region. Abdominal examination revealed hepatosplenomegaly. Rest of the systemic examination was normal. Investigations revealed he had leucocytosis (neutrophilic), serum urea was 64 mg/dL and creatinine of 2.6 mg/dL. Serum bilirubin was 1.74 mg/dL, AST was 643 U/L and ALT of 301 U/L. HbA1c was 8.2%. Ultrasonography abdomen was suggestive of multiple hepatic and splenic abscesses which were confirmed by CT abdomen [Table/Fig-6]. Blood culture was positive for Burkholderia cepacia which was sensitive to meropenem. The patient was given meropenem 1 g intravenous thrice daily for 10 days and then discharged with oral trimethoprim 160 mg and sulfamethoxazole 800 mg to be taken thrice daily for six months. He was followed-up after 1 month and found afebrile with normal ultrasonography of abdomen.
CT abdomen (a) showing multiple hepatic and splenic abscesses. Chest X-ray; (b) showing consolidation with cavity in left upper lobe of lung.
Case 5
A 32-year-old diabetic male was admitted with high grade fever with chills for 18 days, cough with expectoration and left-sided chest pain for 10 days and multiple episodes of vomiting for three days. He was on glimepiride 1 mg, metformin 1000 mg and voglibose 0.2 mg once daily. On examination, patient had a pulse of 130/min, BP of 120/76 mm Hg, respiratory rate of 28/min and oral temperature of 102.5°F. Chest examination revealed bronchial breath sound and presence of crackles in left interscapular, infrascapular and infra-axillary region. Abdominal examination revealed tenderness in right hypochondrium but there was no palpable organomegaly. Rest of the systemic examination was within normal limits. Investigations revealed leucocytosis (neutrophilic) with an HbA1c of 10.5%. CT thorax revealed consolidation with cavities in left lower lobe of lung. CT abdomen showed presence of splenic abscess [Table/Fig-7]. Sputum culture was positive for Burkholderia cepacia which was sensitive to ceftazidime. The patient was given ceftazidime 2 g intravenous thrice daily for 10 days and was discharged with oral trimethoprim 160 mg and sulfomethoxazole 800 mg to be taken thrice daily for six months. On follow-up after 15 days, the patient was afebrile and ultrasonography abdomen was negative for splenic abscess.
CT abdomen (a) showing splenic abscess. CT thorax (b) showing consolidation with cavity in left lower lobe of lung.
Case 6
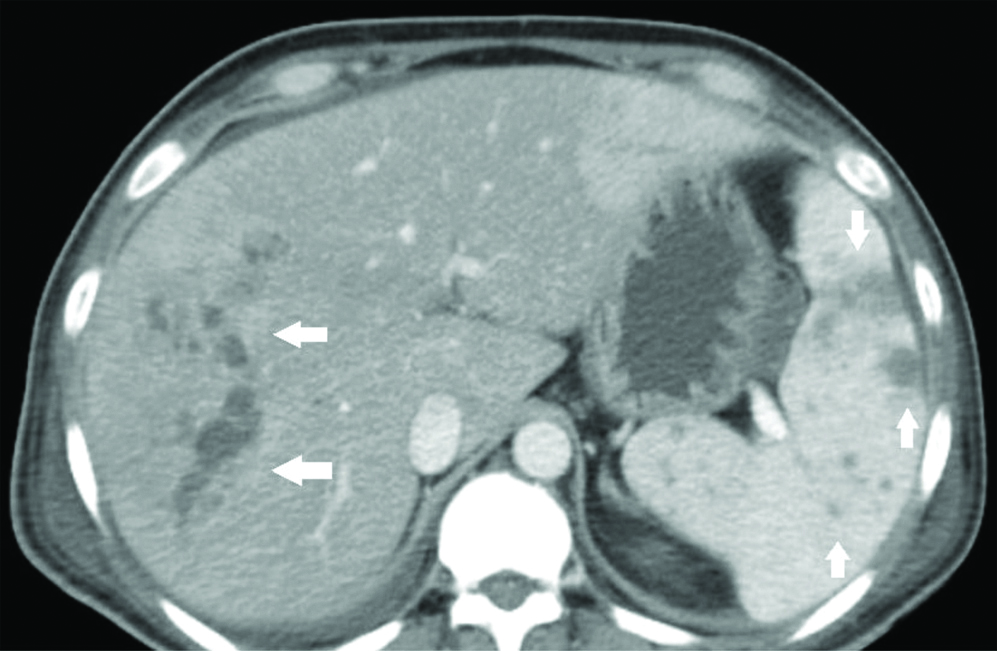
A 52-year-old diabetic male was admitted with complaints of high-grade intermittent fever for one month. The fever was associated with multiple episodes of vomiting and decreased appetite. He also had pain in the right upper abdomen which was dull aching for the last 10 days. He also complained of shortness of breath for last three days. Medication history revealed that the patient was on regular insulin 10 U thrice daily and insulin glargine 10 U once daily. On examination, the patient had a pulse of 116/min, BP of 110/76 mm Hg, respiratory rate of 24/min and oral temperature of 101°F. Abdominal examination revealed hepatomegaly which was tender, firm with sharp margins. Investigations revealed leucocytosis (neutrophilic) and raised serum transaminases. HbA1c was 10.5%. Contrast CT Abdomen revealed multiple liver abscesses with thrombosis of portal venous radicles, multiple splenic abscesses and mild ascites [Table/Fig-8]. Blood culture was positive for Burkholderia cepacia which was sensitive to ceftazidime. Patient was given ceftazidime 2 g intravenous thrice daily for seven days. The patient became afebrile and his appetite improved following which he was discharged with oral trimethoprim 160 mg and sulfomethoxazole 800 mg thrice daily for six months. On follow-up after 15 days, he was afebrile and Ultrasonography abdomen did not reveal any abscesses.
CT abdomen showing multiple hepatic and splenic abscesses.
Discussion
Burkholderia Cepacia Complex (BCC) is an aerobic, gram negative bacillus named after Burkholder, a plant pathologist who discovered it in 1949. These organisms are commonly isolated in soil and moist environments where it can survive for months. These pathogens have high intrinsic resistance and one of the most anti-microbial resistant organisms encountered in a clinical setting [2]. A severe presentation known as the “cepacia syndrome” was first described in children with cystic fibrosis who presented with decline in lung function along with fever, leukocytosis and positive respiratory culture for BCC [3]. This syndrome has also been described in non-cystic fibrosis patients [4]. In India, there are no precise reports of prevalence of BCC infection in non-cystic fibrosis patients. There have been few reports from tertiary care centres of north India [5,6]. There have also been reports of intra-abdominal abscesses caused by Burkholderia pseudomallei. In a case report of a 54-year-old diabetic man by Wu Y-C et al., there was no respiratory involvement and presence of multiple splenic abscesses which on pus culture was evident of Burkholderia pseudomallei [7]. In a 10-year retrospective review of case records from a single centre in Singapore by Ng CY et al., there were 21 cases of splenic abscesses and Burkholderia pseudomallei was isolated from blood in 15 (71%) cases. A 14 (93%) out of 15 patients suffering from Melioidosis were diabetic [8]. The other causative organisms found in the review were Klebsiella and Salmonella. In a prospective observational study of 230 culture positive patients of Melioidosis from northeast Thailand by Maude RR et al., a total of 77 patients had abscesses in either liver or spleen out of which 20 (26%) patients had abscesses in the liver, 33 (43%) patients had abscesses in spleen and 24 (31%) patients had abscesses in both liver and spleen [9]. Most of these patients had multiple abscesses. Five patients had abscesses in other areas such as kidneys, prostate, pancreas and adrenal glands. The authors of the present case series could not find any case report or series describing intra-abdominal abscesses caused by Burkholderia cepacia.
Burkholderia is also a great mimicker. Diagnostic confusion with tuberculosis occurs especially in endemic areas owing to similar patient profile, clinical presentation and indolent course of disease. In an interesting case report by Sugi Subramaniam RV et al., a 33-year-old patient with a previous history of pulmonary tuberculosis and splenic abscesses treated with multi-drug anti-tubercular therapy was admitted with 5 days history of fever, abdominal pain and distension [10]. Emergency laparotomy was done and 100 mL of pus was drained which revealed Burkholderia pseudomallei. The patient was treated with antibiotics but he succumbed on the fifth day. Similarly, in a case report by Ninan F et al., a 53-year-old diabetic farmer from a TB-endemic area had fever and left upper abdominal pain for more than one year and was given anti-tubercular therapy for six months empirically for splenic granuloma [11]. The persistence of symptoms prompted an ultrasound-guided fine needle aspiration from the splenic abscess. The pus was negative for Xpert Tuberculosis Polymerase Chain Reaction (TB PCR) and bacterial culture revealed Burkholderia pseudomallei. He was managed with antibiotics and his symptoms resolved.
In a retrospective observational study by Lee YM et al., 216 non-cystic fibrosis patients suffering from BCC bacteremia were taken into study [12]. The rates of susceptibility to trimethoprim-sulfamethoxazole, ceftazidime, meropenem and levofloxacin of BCC isolates were 92.8%, 75.5%, 72.3%, and 64.1%, respectively. In a 17-year nationwide study of BCC bloodstream infections by Chakhtoura NGE et al., 248 patients were identified with BCC bloodstream infection [13]. Co-trimoxazole was active against 94% isolates compared to ceftazidime and meropenem which was active against 70% isolates.
The similarities in the patients of the present case series lies in the fact that they had underlying diabetes mellitus which was poorly controlled, presented with fever for more than two weeks, respiratory and abdominal symptoms. They were found to have leukocytosis and intra-abdominal abscesses. None of the patients had history of prior hospital visit in last 90 days. All of them had Burkholderia cepacia in blood, sputum or pus and were treated with either meropenem or ceftazidime followed by oral co-trimoxazole. All of them responded to treatment.
Conclusion(s)
Burkholderia is a great mimicker of tuberculosis especially in endemic areas. It affects immunocompromised individuals and can cause multitude of clinical manifestations including intra-abdominal abscesses. Clinical suspicion and early institution of antibiotics results in resolution of illness. The patients were given long term co-trimoxazole as burkholderia is a highly-resistant organism.
Author Declaration:
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 29, 2020
Manual Googling: Sep 01, 2020
iThenticate Software: Oct 16, 2020 (3%)
[1]. Clinical and Laboratory Standards Institute. 2018. Performance standards for antimicrobial susceptibility testing; 27th informational supplement. M100-S28. Clinical and Laboratory Standards Institute, Wayne, PA [Google Scholar]
[2]. Gautam V, Singhal L, Ray P, Burkholderia cepacia complex: Beyond pseudomonas and acinetobacterIndian J Med Microbiol 2011 29(1):04-12.10.4103/0255-0857.7651621304187 [Google Scholar] [CrossRef] [PubMed]
[3]. Isles A, Maclusky I, Corey M, Gold R, Prober C, Fleming P, Pseudomonas cepacia infection in cystic fibrosis: An emerging problemJ Pediatr 1984 104(2):206-10.10.1016/S0022-3476(84)80993-2 [Google Scholar] [CrossRef]
[4]. Hauser N, Orsini J, Cepacia syndrome in a non-cystic fibrosis patientCase Rep Infect Dis 2015 2015:53762710.1155/2015/53762726357579 [Google Scholar] [CrossRef] [PubMed]
[5]. Gautam V, Arora A, Madhup SK, Das A, Vandamme P, Sharma K, Burkholderia cepacia complex in septicaemic non-cystic fibrosis cases from two tertiary care hospitals in north IndiaIndian J Med Res 2010 131:829-32.PMID: 20571175 [Google Scholar]
[6]. Gautam V, Ray P, Das A, Vandamme P, Malhotra P, Varma S, Two cases of Burkholderia cenocepacia in septicemic patientsJpn J Infect Dis 2008 61(2):133-34. [Google Scholar]
[7]. Wu YC, Hsu JW, Chang TH, Kung WC, Melioidosis in an urban dwelling Taiwanese man with splenic abscessesTrop Doct 2010 40(4):240-41.10.1258/td.2010.09047220709809 [Google Scholar] [CrossRef] [PubMed]
[8]. Ng CY, Leong EC, Chng HC, Ten-year series of splenic abscesses in a general hospital in SingaporeAnn Acad Med Singapore 2008 37(9):749-52. [Google Scholar]
[9]. Maude RR, Vatcharapreechasakul T, Ariyaprasert P, Maude RJ, Hongsuwan M, Yuentrakul P, Prospective observational study of the frequency and features of intra-abdominal abscesses in patients with melioidosis in northeast ThailandTrans R Soc Trop Med Hyg 2012 106(10):629-31.10.1016/j.trstmh.2012.05.00722770892 [Google Scholar] [CrossRef] [PubMed]
[10]. Sugi Subramaniam RV, Karthikeyan VS, Sistla SC, Ali SM, Sistla S, Vijayaraghavan N, Intra-abdominal melioidosis masquerading as a tubercular abdomen: Report of a rare case and literature reviewSurg Infect (Larchmt) 2013 14(3):319-21.10.1089/sur.2011.13623581631 [Google Scholar] [CrossRef] [PubMed]
[11]. Ninan F, Mishra AK, John AO, Iyadurai R, Splenic granuloma: Melioidosis or Tuberculosis?J Family Med Prim Care 2018 7(1):271-73.10.4103/jfmpc.jfmpc_171_1729915776 [Google Scholar] [CrossRef] [PubMed]
[12]. Lee YM, Park KH, Moon C, Kim DY, Lee MS, Kim T, Management and outcomes of Burkholderia cepacia complex bacteremia in patients without cystic fibrosis: a retrospective observational studyEur J Clin Microbiol Infect Dis 2020 39(11):2057-64.10.1007/s10096-020-03960-232583228 [Google Scholar] [CrossRef] [PubMed]
[13]. Chakhtoura NGE, Saade E, Wilson BM, Perez F, Papp-Wallace KM, Bonomo RA, A 17-year nationwide study of Burkholderia Cepacia complex bloodstream infections among patients in the United States Veterans health administrationClin Infect Dis 2017 65(8):1253-59.10.1093/cid/cix55929017247 [Google Scholar] [CrossRef] [PubMed]