A Case of Disseminated Extensively Drug Resistant Extrapulmonary Tuberculosis
Diti V Gandhasiri1, Tilak M Dhamgaye2, Ulhas Jadhav3, Babaji Ghewade4
1 Resident, Department of Respiratory Medicine, Jawaharlal Nehru Medical College, DMIMS University, Wardha, Maharashtra, India.
2 Professor, Department of Respiratory Medicine, Jawaharlal Nehru Medical College, DMIMS University, Wardha, Maharashtra, India.
3 Professor and Head, Department of Respiratory Medicine, Jawaharlal Nehru Medical College, DMIMS University, Wardha, Maharashtra, India.
4 Professor, Department of Respiratory Medicine, Jawaharlal Nehru Medical College, DMIMS University, Wardha, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Tilak M Dhamgaye, Department of Respiratory Medicine, Jawaharlal Nehru Medical College, Sawangi(M), DMIMS University, Wardha, Maharashtra, India.
E-mail: tmdhamgaye@yahoo.co.in
Tuberculosis (TB) strains with drug resistance are more difficult to treat than drug susceptible ones and jeopardise global progress towards the targets set by the World Health Organisation’s End TB Strategy. Although disseminated TB is well known as an opportunistic infection in HIV infected individuals, it is uncommon in HIV negative individuals. The present case is a rare case of Extensively Drug Resistant (XDR)-TB in disseminated TB involving the extrapulmonary sites in an immunocompetent adult. We report a case of a young man who has disseminated TB involving pleura and peritoneum. Prior to this, he had taken category II anti-TB treatment with no satisfactory response. Drug sensitivity test of pleural fluid revealed resistance to quinolones, kanamycin, isoniazid and rifampicin. Patient was administered second line anti-TB therapy with remarkable response. Therefore, this case highlights the importance of investigating aggressively for Drug Resistance (DR) in suspected cases of extrapulmonary TB.
Disseminated tuberculosis, Extensively drug resistant tuberculosis, Extrapulmonary tuberculosis
Case Report
A 33-year-old male patient presented to the emergency department with complaints of abdominal distention, vomiting associated with pain in the abdomen and loss of appetite of one week duration. He was a previously diagnosed case of smear positive pulmonary TB at a peripheral health centre three months before admission to this hospital and was on treatment for the same since four months. Patient had a history of alcoholism with consumption of around 120 mL of country liquor on a daily basis since the age of 15 years along with tobacco chewing. He also gave history of hepatotoxicity that he developed due to his medications. His anti-tuberculous drugs were modified twice during the course. Patient gave history of smear positive pulmonary TB twice in the past and in both cases, he had defaulted the recommended treatment.
The patient was examined in supine position and appeared to be in considerable distress due to abdominal pain with a heart rate of 120 beats/minute, respiratory rate of 24 breaths/minute, a temperature of 37.4°C, and blood pressure of 110/70 mmHg. The patient was icteric, Grade II clubbing was present and bilateral pitting pedal oedema was noted without elevated jugular venous pressure. Respiratory examination revealed the possibility of a left sided pleural effusion. Per abdomen examination showed a slightly distended abdomen and confirmed the presence of free fluid in the abdominal cavity suggestive of ascites without any organomegaly. Rest of the systemic examination was unremarkable. Laboratory investigations revealed a normal hemogram with elevated liver enzymes (Alanine Aminotransferase (ALT): 186 IU/L and Aspartate Aminotransferase (AST): 245 IU/L), raised serum bilirubin levels (total bilirubin: 3.54 mg/dL, conjugated: 1.47 mg/dL and unconjugated: 2.07 mg/dL) and decreased serum total protein and albumin levels (total protein: 5.8 g/dL and albumin: 2.9 gm/dL). Patient’s serum was negative for Human Immunodeficiency Virus (HIV), Hepatitis B (HbsAg) antigen and Hepatitis C Virus (HCV).
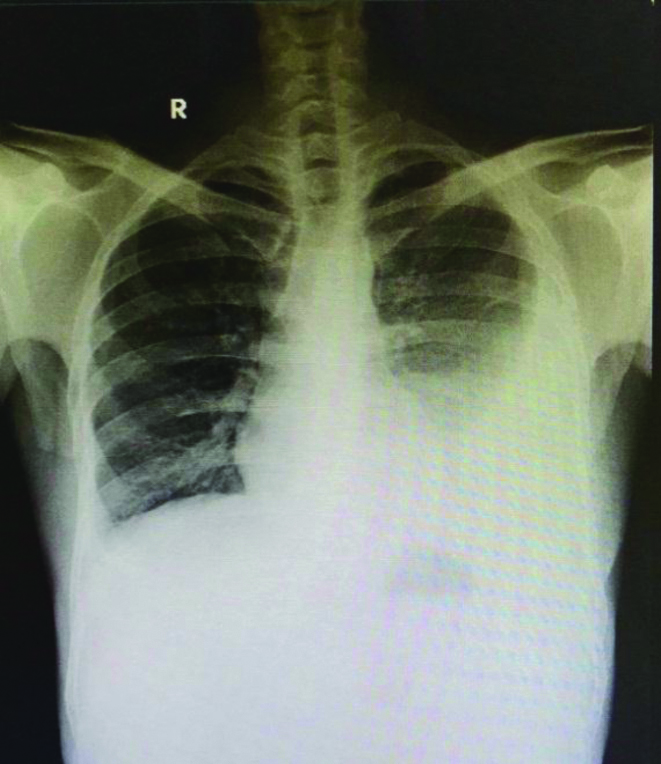
Chest roentgenogram showed blunting of bilateral costophrenic angles suggestive of pleural effusion which was mild on the right side and moderate on the left [Table/Fig-1]. Chest ultrasonogram revealed moderate fluid in the left pleural cavity. Abdominal ultrasonogram showed moderate ascites with liver normal in size and echotexture with no focal lesion.
Chest radiograph PA view showing moderate pleural effusion.
PA: Posteroanterior
With due aseptic precautions and under ultrasonographic guidance pleural and ascitic fluid was tapped and sent for evaluation. Pleural fluid was exudative with acute inflammatory, mixed leukocytic exudation on cytology and ascitic fluid had a SAAG of 1.0 with a lymphocytic predominant exudate on cytopathology report. Pleural fluid Adenosine Deaminase (ADA) (62 U/L) and ascitic fluid ADA (106 U/L), both strongly suggested the possibility of TB. Establishing a diagnosis of TB was no surprise, but what did intrigue us was the possibility of Drug Resistance (DR) as the patient had history of previous incomplete treatment and was on category II of Directly Observed Treatment Short-Course Chemotherapy (DOTS) for TB for three months with serious adverse drug reaction and no improvement. As the patient developed jaundice with elevated serum bilirubin and liver enzyme level, treatment with the hepatotoxic drugs (isoniazid, rifampicin, and pyrazinamide) were stopped. Patient was administered a modified regimen comprising of ethambutol, streptomycin, and quinolone.
Patient’s pleural fluid’s Ziehl-Nielson staining for acid-fast bacilli was negative. GeneXpert MTB/RIF of the pleural fluid showed Mycobacterium Tuberculosis (MTB) complex and rifampicin resistance. Sputum GeneXpert MTB/RIF examination showed no evidence of MTB. Therefore, the patient was diagnosed as a case of Multidrug Resistant (MDR) TB involving the pleura as well as abdomen. Later as patient was clinically improved and biochemical parameters including serum bilirubin were stabilised, MDR regimen of Antitubercular Chemotherapy (ATT) under Revised National TB Control Programme (RNTCP) Programmatic Management of Drug Resistant TB (PMDT) was started. Subsequently, the pleural fluid was sent for Line Probe Assay (LPA) which revealed additional resistance to quinolones and low-level resistance to Kanamycin and final diagnosis of disseminated XDR extrapulmonary TB was given.
After conducting the pre-evaluation tests patient was started on Capreomycin, Ethionamide, Ethambutol, Cycloserine, Pyrazinamide, Linezolid, Clofazimine, and Bedaquiline 400 mg twice daily for five days followed by 200 mg once daily on alternate days. Patient has showed considerable improvement with treatment at the end of one year and was followed-up in our hospital with good adherence to the anti-tubercular drugs.
Discussion
TB is a global public health concern with an estimated 10.0 million developed cases of TB in 2018 worldwide. On the other hand, DR-TB continues to be a public health threat. In 2018, globally, there were about half a million new cases of rifampicin-resistant TB/MDR TB. India accounts for 27% of the global TB burden i.e., 2.7 out of 10 million cases annually [1]. India has the highest burden of both TB and MDR-TB in the world with daily incidence of more than 6000 new cases and daily mortality of almost 600 cases. TB strains with DR-TB are more difficult to treat than drug susceptible ones and threaten global progress towards the targets set by the End TB Strategy of the WHO [2].
The emergence of MDR TB and XDR is another threat to the control of the disease [3]. MDR is defined as resistance to isoniazid and rifampicin, two of the most potent first line drugs; XDR is resistance to isoniazid, rifampicin, fluoroquinolones, and any of the second line injectable agents. The most important risk factor in the development of DR is an improper implementation of the guidelines in the management of TB and defaults in treatment. Other risk factors like diabetes, alcohol misuse, and intravenous drug abuse also play an important role in the development of DR [4]. Disseminated TB diagnosis can be made when the infection involves the blood stream, bone marrow or two or more noncontiguous body sites [5]. Disseminated TB is estimated to occur in 1-5% of all TB cases [6]. Dissemination of TB occurs through haematogenous or lymphatic spread from the primary site of TB to many distant organ sites. This occurs more commonly in HIV-infected patients (upto 31% of patients) [7]. Young men are at a greater risk of developing DR than women, possibly due to excessive consumption of alcohol, smoking and drugs [8]. Several studies reported significant associations between alcohol misuse status and MDR-TB occurrence [9].
In India, extrapulmonary TB comprises about 15-20% of all TB, mostly TB lymphadenitis and pleural effusion. Patients with extrapulmonary manifestations require specialised investigations and the diagnosis is usually based upon an array of clinical, radiological or histopathological findings rather than solely on bacteriologic evidence [10]. Detection of MDR/Rimfapicine-Resitant (RR-TB) requires bacteriological confirmation of TB and testing for DR using rapid molecular tests, culture methods or sequencing of technologies [1]. Molecular-based resistance testing Xpert MTB/RIF detects resistance to rifampicin and provides results within one and a half hours. LPA detects resistance to isoniazid, rifampicin, ethambutol, fluoroquinolones as well as second-line injectable drugs such as amikacin, kanamycin, capreomycin and provide results within two days.
Published data on the prevalence and drug resistance pattern among extrapulmonary TB cases are sparse. In a study done in New Delhi, on extrapulmonary TB patients, MDR-TB was evident in 8.1% while XDR-TB in 2.6% of the total extrapulmonary specimens collected [11]. Another study in Greece on pattern of DR among patients with tuberculous pleural effusion showed resistance to at least one first line drug in 11% of cases. MDR and XDR-TB were found in 3% and 1% of tuberculous pleural effusion cases respectively [12]. Treatment of multidrug resistant TB and XDR-TB is challenging because of the longer treatment duration, adverse effects, and lower efficacy of second line drugs [13].
This patient had developed jaundice during antitubercular category II therapy. Patient’s serum HbsAg antigen and HCV examination was negative and abdominal ultrasonogram showed that the liver was normal. All possible causes of jaundice were ruled out. Treatment with the hepatotoxic drugs was stopped and patient was administered a modified regimen comprising of ethambutol, streptomycin and quinolone. In the course of DR investigation, pleural fluid LPA revealed resistance to quinolone, kanamycin, isoniazid, in addition to rifampicin and patient was diagnosed as a case of XDR-TB. Patient was administered three new drugs-Bedaquiline, Clofazimine and Linezolid.
Bedaquiline is the first new anti-TB drugs in 40 years. Bedaquiline inhibits mycobacterial ATP synthase and it has shown more rapid sputum culture conversion in MDR and XDR-TB cases. Studies have indicated its effectiveness in treating pulmonary XDR-TB in combination with other new drugs [14]. Treatment duration of 18-24 months is standard for these severely ill patients, and the selection of drugs for treatment should be guided by phenotypic and genotypic sensitivity testing. Monitoring strategy of drug resistant extrapulmonary TB depends mainly on the clinical and radiological observation [Table/Fig-2] [10]. According to WHO global TB report, treatment success rate in MDR/RR TB cases started on second line treatment in 2016 was 48% and in XDR-TB it was 30% [1].
Follow-up chest radiograph PA view after six weeks showing improvement.

Limited drug susceptibility laboratories jeopardise the new diagnosis of XDR-TB cases. Drug susceptibility testing is the main stay of diagnosing XDR-TB but its use is widely limited because of lack of laboratories in resource limited countries.
Conclusion(s)
This case has been reported to highlight that high degree of suspicion is needed to identify such cases of XDR-TB among the patients with extrapulmonary TB. Access to rapid molecular drug susceptibility testing recommended by WHO at treatment initiation is required to improve outcome in patients with MDR-TB and XDR-TB. It is imperative to extend the universal implementation of high-quality programmatic management of drug resistant TB to all the cases to eliminate TB.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: May 19, 2020
Manual Googling: May 27, 2020
iThenticate Software: Oct 15, 2020 (2%)
[1]. WHO. Global Tuberculosis Report 2019. World Health Organization, Geneva; 2019 [Google Scholar]
[2]. World Health Organization. WHO consolidated guidelines on drug-resistant tuberculosis treatment. [Internet]. 2019 [cited 2020 Apr 16] [Google Scholar]
[3]. Mariandyshev A, Eliseev P, Drug resistant tuberculosis threatens WHOs End-TB strategyLancet Inf Dis 2017 17:674-75.10.1016/S1473-3099(17)30246-3 [Google Scholar] [CrossRef]
[4]. Dadra R, Kajal N, Malhotra B, Pandiyaraj P, Kaur L, kaur G, Disseminated multidrug-resistant tuberculosis in a young patient: A rare case reportJ Assoc Chest Physicians 2020 8(1):2610.4103/jacp.jacp_21_19 [Google Scholar] [CrossRef]
[5]. Crump JA, Reller LB, Two decades of disseminated tuberculosisat a university medical center: The expanding role of mycobacterial blood cultureCli Infect Dis 2003 37:1037-43.10.1086/37827314523767 [Google Scholar] [CrossRef] [PubMed]
[6]. Mert A, Arslan F, Kuyucu T, Koç EN, Ylmaz M, Turan D, Miliary tuberculosis: Epidemiological and clinical analysis of large case series frommoderate to low tuberculosis endemic countryMedicine (Baltimore) 2017 96:e587510.1097/MD.000000000000587528151863 [Google Scholar] [CrossRef] [PubMed]
[7]. Kerkhoff AD, Barr DA, Schutz C, Burton R, Nicol MP, Lawn SD, Disseminated tuberculosis among hospitalised HIV patients in South Africa: A common condition that can be rapidly diagnosed using urine-based assaysSci Rep 2017 7:1093110.1038/s41598-017-09895-728883510 [Google Scholar] [CrossRef] [PubMed]
[8]. Rajendran M, Zaki RA, Aghamohammadi N, Contributing risk factors towards the prevalence of multidrug-resistant tuberculosis in Malaysia: A systematic reviewTuberculosis (Edinb) 2020 122:10192510.1016/j.tube.2020.10192532275233 [Google Scholar] [CrossRef] [PubMed]
[9]. Mohd Shariff N, Shah SA, Kamaludin F, Predictors of death among drug-resistant tuberculosis patients in Kuala Lumpur, Malaysia: A retrospective cohort study from 2009 to 2013J Glob Antimicrob Resist 2016 6:102-07.10.1016/j.jgar.2016.04.00527530850 [Google Scholar] [CrossRef] [PubMed]
[10]. Dusthackeer A, Sekar G, Chidambaram S, Kumar V, Mehta P, Swaminathan S, Drug resistance among extrapulmonary TB patients: Six years experience from a supranational reference laboratoryIndian J Med Res 2015 142(5):56810.4103/0971-5916.17128426658592 [Google Scholar] [CrossRef] [PubMed]
[11]. Sharma S, Chaubey J, Singh BK, Sharma R, Mittal A, Sharma A, Drug resistance patterns among xtr-pulmonary tuberculosis cases in a tertiary care centre in North IndiaInter J Tuberc and Lung Disease 2017 21(10):1112-17.10.5588/ijtld.16.093928911354 [Google Scholar] [CrossRef] [PubMed]
[12]. Anastaskos V, Skouras V, Moschos C, Tsikrika S, Karabela S, Pattern of drug resistance among patients with tuberculous pleural effusion in GreeceInter J Tuberc Lung Dis 2017 21(3):309-13.10.5588/ijtld.16.015528225341 [Google Scholar] [CrossRef] [PubMed]
[13]. Horsburgh CR Jr, Barry CE, Lange C, Treatment of tuberculosisN Eng J Med 2015 373:2149-60.10.1056/NEJMra141391926605929 [Google Scholar] [CrossRef] [PubMed]
[14]. Pym AS, Diacon AH, Tang SJ, Conradie F, Danilovits M, Bedaquiline in the treatment of multidrug and extensively drug resistant tuberculosisEur Respir J 2016 47(2):564-74.10.1183/13993003.00724-201526647431 [Google Scholar] [CrossRef] [PubMed]