Immune Thrombocytopenia (ITP) is an autoimmune disorder characterised by a low circulating platelet count. ITP is caused by destruction of antibody-sensitised platelets in the reticuloendothelial system. Majority of the patients with ITP remain asymptomatic or develop only purpura, petechiae or epistaxis (83%) but few, very rarely, may present with abnormal uterine bleeding. On the other hand, Neurofibromatosis is an autosomal dominant disorder which can present with either precocious puberty or delayed puberty. This case report highlights a case of a 14-year-old female who presented with heavy menstrual bleeding as a presenting symptom of ITP and was co-incidentally also diagnosed as Neurofibromatosis type 1 (NF-1) during work-up of ITP for multiple hyperpigmented macules (Café-au-lait spots) noticed on her neck, forearm and back and the presence of Lisch nodules in iris. She was managed with steroids, oral contraceptive pills, iron and multivitamin tablets.
Café-au-lait spots, Heavy menstrual bleeding, Lisch nodules, Platelet count, Steroids
Case Report
A 14-year-old girl presented to the Gynaecology Outpatient Department with heavy menstrual bleeding from last 3 months. Bleeding was associated with the passage of clots but there was no dysmenorrhoea. She had menarche at 12 years of age and since then, the cycles were of 3-5 days duration at 30 days interval with average flow. But for the last three months, she experienced heavy bleeding which got relieved to some extent on tranexamic acid and for the last 15 days, it was continuous with no response even on hormonal tablets (norethisterone 30 mg daily). For this, the patient was investigated at a private centre and received three units of Packed Red Blood Cells (PRBC) for severe anemia, 11 units of platelets for thrombocytopenia and was then, referred to a higher centre for further management. She also has a history of easy bruising and gum bleeding from last two months. There was no history of any viral illness or prolonged use of nonsteroidal drug intake.
On examination, her general condition was fair, moderate pallor was present and respiratory and cardiovascular system was within normal limits. Abdominal examination revealed no hepatosplenomegaly. On admission, her haemoglobin was 7.2 gm%, platelet count was 4000 per cubic mm, peripheral blood film was suggestive of normocytic and normochromic anaemia with immature platelets >35%. Total leukocyte count, liver and renal function test and coagulation screen were normal, dengue antibodies (Ig G and Ig M), rapid malarial antigen, Antinuclear Antibody (ANA), anti-neutrophil cytoplasmic antibody (pANCA & cANCA) and anti-double-stranded DNA antibody tests were also negative. She was screened negative for hepatitis B, C and Human Immunodeficiency Virus (HIV). No abnormality was detected on ultrasonography of abdomen and pelvis. Hence, a diagnosis of ITP based on exclusion of other causes was made.
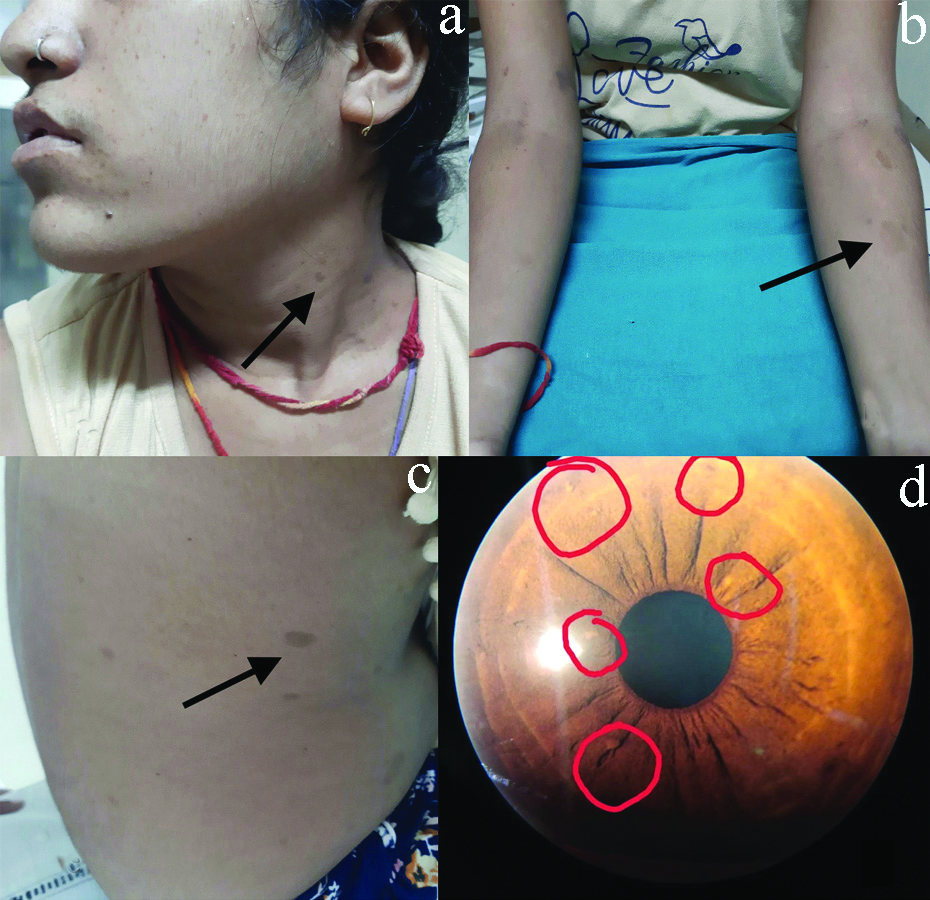
During the course of her evaluation, multiple hyper-pigmented macules (Café-au-lait spots) were noticed on her neck, forearm and back, with few measuring more than 15 mm [Table/Fig-1a-c]. Axillary freckling was also noticed. Neurofibromatosis type 1 was considered a differential diagnosis. Further, the presence of Lisch nodules [Table/Fig-1d] in iris confirmed the diagnosis.
Arrow showing Café-au-lait spots (a,b,c) and Lisch nodules in iris (d).
However, there were no noticeable cutaneous neurofibromas or skeletal deformity in the girl. Moreover, parents also did not reveal any similar history in the family. She has two siblings who were also found to be normal on clinical examination. Psychiatric evaluation showed average intelligence with Intelligence Quotient (IQ) of 85 and 2D echocardiography was also normal.
On account of ITP, she was managed with steroids (Prednisone 60 mg per day) for one week and then, gradually the dose was tapered and stopped after six weeks. Oral contraceptive pills (Ethinyl oestradiol-0.03 mg and Levonorgesterol- 0.15 mg combination) along with iron and multivitamin tablets were given for three months. The platelet count started increasing from third day onwards (from 4000/cumm on day of admission to 1.5 lacs/cumm on day three of steroid). On discharge from the hospital on 11th day, haemoglobin was 10.5 gm% and platelet count was 2.09 lacs per cubic mm. For Neurofibromatosis, she was advised routine follow-up in the medicine clinic of the institute.
On her subsequent visit after two weeks, her platelet count was 2.56 lacs per cu mm. At three months follow-up visit, she had normal menstrual flow following a period of amenorrhoea, probably due to continuous Oral Contraceptive Pills (OCPs), one episode of heavy bleeding at five months which was controlled on tranexamic acid (Platelet count -1.85 lacs/cu mm) and normal bleeding thereafter for three cycles at eight months follow-up. On each visit, the examination was unremarkable with no new development of neurofibromas or sensory or motor neurological abnormalities. However, she was counseled regarding possibility of restarting of steroids in future due to recurrent nature of ITP.
Discussion
Abnormal uterine bleeding in adolescents is a common gynaecological issue. Approximately, 37% of the teenage girls suffer from it and the most common aetiological factor attributed to it is anovulation owing to immaturity of the hypothalamic-pituitary-ovarian axis followed by coagulation or haemostatic disorder [1]. ITP, previously called idiopathic thrombocytopenic purpura is a rare cause of AUB. Majority of the patients with ITP remain asymptomatic or develop only purpura, petechiae or epistaxis (83%) but few, very rarely, may present with abnormal uterine bleeding [2]. It is an autoimmune disorder characterised by a significant fall in peripheral blood platelet count from 150-450×109/L (normal reference range in healthy individuals) to less than 100×109/L [3]. In adults, the incidence of ITP is approximately two to four per 100,000 [4,5] whereas, the incidence in children vary with age with a higher incidence in young as compared to adolescents [6]. In the present case, all possible causes of thrombocytopenia (dengue, malaria, disseminated intravascular coagulation, thrombotic thrombocytopenic purpura, haemolytic uremic syndrome and systemic lupus erythematosus) were excluded as evidenced by laboratory investigations and subsequently the diagnosis of ITP was made. She was also concurrently diagnosed as Neurofibromatosis type 1 based on the clinical findings.
Although, the authors could not find any literature suggesting an association of ITP with NF-1 except one case report in which a girl was diagnosed to have NF-1 at six years of age and later developed ITP at 11 years of age [7], this case is unique as there was a strange concurrence of the two conditions at the same time.
NF-1 is an autosomal dominant disease caused by mutations in the NF-1 gene located at the 17q11.2 chromosome. Its prevalence is one in 3,000 births [8]. The manifestations in NF-1 can range from mild lesions to severe complications and functional impairment. The diagnosis is usually clinical and is considered if any two of the seven features are present [Table/Fig-2] [9]. Café-au-lait spots are symmetrical flat areas of skin hyperpigmentation with rounded edges and are seen in 95% cases of NF-1. Besides, 70% cases show freckling of the intertriginous area of the axilla or groin. About 95% of individuals with NF-1 develop Lisch nodules which are benign multiple melanotic hamartomas of the iris [8]. All these three features were present in this case. Very rarely, one may require molecular testing for the confirmation of NF-1 by sequencing neurofibromin gene but most of the time, it is not feasible in the clinical setting.
Diagnostic criteria of Neurofibromatosis by Gutmann DH et al., [9].
| The patient should have two or more of the following: |
| 1. Six or more café-au-lait spots |
| • 11.5 cm or larger in post-pubertal individuals |
| • 0.5 cm or larger in pre-pubertal individuals |
| 2. Two or more neurofibromas of any type or one or more plexiform neurofibroma |
| 3. Axillary or groin freckling |
| 4. Optic glioma |
| 5. Two or more Lisch nodules (benign melanotic iris hamartomas) |
| 6. A distinctive bony lesion |
| • Dysplasia of the sphenoid bone |
| • Dysplasia or thinning of long bone cortex |
| 7. A first degree relative with NF-1 |
Usually, NF-1 is associated with precocious puberty and occasionally delayed puberty but in the present case, the girl had menarche at 12 years of age and the parents did not give any history suggestive of precocious puberty. Her height was 153 cm and her IQ was 85. Since, her primary concern was heavy menstrual bleeding, the focus was on ITP.
Corticosteroids are usually the first choice for initial treatment of ITP. However, patients with active bleeding respond faster with Intravenous Immunoglobulin (IVIG) which can increase platelet count more rapidly [10]. The most common regimens followed are oral prednisone 0.5-2.0 mg/kg per day for two to four weeks followed by a gradual taper or dexamethasone 40 mg per day for four days every two to four weeks for one to four cycles with no taper [3].
The American Society of Haematology (ASH) [11] and International Consensus Report on ITP [12] recommend that bone marrow examination is not necessary for children and adolescents with the typical features of ITP, before initiation of treatment with corticosteroids or before splenectomy. The testing for anti-nuclear antibodies is also not necessary for the evaluation of children and adolescents with suspected ITP. This patient received prednisone and had an explicit response in platelet count as well as symptoms.
For Neurofibromatosis, regular follow-up is necessary. On every visit, a detailed cutaneous examination for the development of new neurofibromas or progression of preexisting lesions to be done, to check blood pressure, to ask for incontinence and any minor sensory or motor changes must be documented. The present case was attached with the medicine clinic and during follow-up till eight months after the discharge, she was absolutely fine with no significant new complaints. However, for last four months due to the COVID-19 pandemic, she didn’t follow-up.
Conclusion(s)
ITP remains a rare but important cause of AUB in adolescents and steroids can be preferred over IVIG and/or splenectomy. A regular follow-up is required for Neurofibromatosis, even if the patient is asymptomatic. Moreover, further research is required to prove or disprove any relation of neurofibromatosis with ITP.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes (from parents)
For any images presented appropriate consent has been obtained from the subjects. Yes (from parents)
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jul 14, 2020
Manual Googling: Sep 15, 2020
iThenticate Software: Oct 15, 2020 (4%)
[1]. Karaman K, Ceylan N, Karaman E, Akbayram S, Akbayram HT, Kaba S, Evaluation of the hemostatic disorders in adolescent girls with menorrhagia: Experiences from a tertiary referral hospitalIndian J Hematol Blood Transfus 2016 32(3):356-61.10.1007/s12288-015-0583-527429530 [Google Scholar] [CrossRef] [PubMed]
[2]. Camacho S, Zahouani T, Mendez M, Adolescent with transvaginal bleeding: Rare presentation of immune thrombocytopenic purpuraPediatr Ther 2016 6(4)10.4172/2161-0665.1000304 [Google Scholar] [CrossRef]
[3]. Khan AM, Mydra H, Nevarez A, Clinical practice updates in the management of immune thrombocytopeniaPharmacy and Therapeutics 2017 42(12):756-63. [Google Scholar]
[4]. Lambert MP, Gernsheimer TB, Clinical updates in adult immune thrombocytopenia (ITP) Blood 2017 129(21):2829-35.10.1182/blood-2017-03-75411928416506 [Google Scholar] [CrossRef] [PubMed]
[5]. Abadi U, Yarchovsky-Dolberg O, Ellis MH, Immune thrombocytopenia: Recent progress in pathophysiology and treatmentClin Appl Thromb Hemost 2015 21(5):397-404.10.1177/107602961452663924623064 [Google Scholar] [CrossRef] [PubMed]
[6]. Yong M, Schoonen WM, Li L, Kanas G, Coalson J, Mowat F, Epidemiology of paediatric immune thrombocytopenia in the General Practice Research DatabaseBr J Haematol 2010 149(6):855-64.10.1111/j.1365-2141.2010.08176.x20377590 [Google Scholar] [CrossRef] [PubMed]
[7]. Singh R, Gardner S, Allen J, TRTH-20. Treatment of optic pathway glioma and Immune Thrombocytopenia (ITP) with everolimusNeuro Oncol 2017 19(Suppl 4):iv5510.1093/neuonc/nox083.231PMC5475206 [Google Scholar] [CrossRef] [PubMed]
[8]. Cunha KS, Barboza EP, Dias EP, Oliveira FM, Neurofibromatosis type I with periodontal manifestation. A case report and literature reviewBr Dent J 2004 196(8):457-60.10.1038/sj.bdj.481117515105854 [Google Scholar] [CrossRef] [PubMed]
[9]. Gutmann DH, Aylsworth A, Carey JC, Korf B, Marks J, Pyeritz RE, The diagnostic evaluation and multidisciplinary management of neurofibromatosis 1 and neurofibromatosis 2JAMA 1997 278(1):51-57.10.1001/jama.1997.035500100650429207339 [Google Scholar] [CrossRef] [PubMed]
[10]. Raj AB, Immune thrombocytopenia: Pathogenesis and treatment approachesJ Hematol Transfus 2017 5(1):1056-65. [Google Scholar]
[11]. Neunert C, Lim W, Crowther M, Cohen A, Solberg L, Crowther M, The American Society of Hematology 2011 evidence-based practice guideline for immune thrombocytopeniaBlood 2011 117(16):4190-207.10.1182/blood-2010-08-30298421325604 [Google Scholar] [CrossRef] [PubMed]
[12]. Provan D, Arnold DM, Bussel JB, Chong BH, Cooper N, Gernsheimer T, Updated international consensus report on the investigation and management of primary immune thrombocytopeniaBlood Adv 2019 3(22):3780-817.10.1182/bloodadvances.201900081231770441 [Google Scholar] [CrossRef] [PubMed]