Introduction
Maintaining a vital pulp of immature permanent teeth is an essential and important requirement for dentin formation. Every effort must be made to preserve the vitality of teeth with incomplete apices to maintain the physiological apex generation process as much as possible. Pulpotomy is considered as one of the successful procedures to maintain this process in immature teeth.
Aim
To evaluate the treatment success of pulpotomy of first immature molars with irreversible pulpitis using Platelet-Rich Fibrin (PRF) or Mineral Trioxide Aggregate (MTA) and monitoring the teeth for one year.
Materials and Methods
A randomised clinical and radiological double-blinded evaluation was conducted in the Department of Paediatric Dentistry at Damascus University, Damascus, Syria. The research sample consisted of 24 first permanent immature molars in 20 children between age group of 6-8 years. Each of them had at least one first permanent immature molar with irreversible pulpitis. The research sample was randomly divided into two equal groups according to the treatment method: 1) pulpotomy with PRF; and 2) pulpotomy using MTA. Treatment were evaluated through periodic reviews and clinical and radiological examinations of the treated teeth by three specialists to assess treatment success. The treatment outcome was determined in terms of success or failure during two study periods (after six months and after one year). McNemar’s and Chi-square tests were applied using IBM SPSS version 20.0. The significance level was set at p-value <0.05.
Results
Chi-square test showed that there were no statistically significant differences in the treatment success or failure between the treatment groups after six months and one year follow-up, p>0.05. After analysing the results statistically using McNemar’s test, it was observed that the treatment success rate after one year (50%, n=6) was lesser than that after six months (100%, n=12) in the MTA treatment group (p=0.031). In the treatment group using PRF, no significant difference (p=0.125) was observed in the success or failure of treatment between the two studied time periods (after six months and one year). Overall, the success rate of MTA was slightly higher than the success rate of PRF at the two study time periods (after six months and one year), the difference however was not statistically significant.
Conclusion
Performing first immature molar pulpotomy using MTA had a slightly higher success rate than PRF pulpotomy.
Introduction
The mixed dentition period begins when the child reaches the age of six years, as the eruption of immature permanent teeth begins, which are defined as the teeth that emerge into the oral cavity without completion of root formation and closure of apices [1]. Usually, the apex is formed two to three years after eruption of the tooth in the oral cavity [1]. Maintaining a vital pulp of immature permanent teeth is an essential and important requirement for dentin formation. The loss of vitality in the immature permanent teeth before the root formation has completed would lead to the formation of weak root, thin walls that fractures easily so that the usual endodontic techniques become unsuitable to seal off the canals of these teeth [2]. Every effort must be made to preserve the vitality of teeth with incomplete apexes to maintain the physiological apex generation process as much as possible.
The direct and indirect pulp capping and pulpotomy procedures are successful procedures when dealing with these immature teeth due to the abundant blood supply from the open apex and thus, the application of such treatments is coupled with the availability of qualifying factors for such cases to succeed [3].
Immature permanent teeth are important in the development and growth of the alveolar bone and periodontal ligament, they are considered an important source of tissue to do research on stem cells in adults. Reimplantation of immature permanent teeth has a high success rate. Open apex measurement of immature permanent teeth is useful to determine the chronological age. Stem cells in the apical papilla of these teeth can differentiate into dentin-generating cells and give tissue similar to dentin [4].
Materials used in permanent teeth pulpotomy may vary; some have more biocompatibility and more success rate than others such as PRF and MTA which have better properties than calcium hydroxide powder [5].
The first use of PRF was reported by Choukroun J et al., specifically in the field of oral and maxillofacial surgery, and it is considered as a new generation of platelet concentrate [6,7]. PRF consists of a self-fibrinous template rich in platelets, formed by a quaternary molecular structure containing cytokines, platelets and stem cells, and helps in the development of microvasculature and is able to direct the migration of epithelial cells to its surface [8-10]. The PRF possesses a complex structure of a strong fibrous culture with appropriate mechanical properties, which can be slowly reconfigured resembling a blood clot [11].
The MTA was first described in literature by researcher Lee SJ et al., in which they tested the ability of this substance to repair lateral root perforations and prevent marginal leakage compared to amalgam and zinc oxide-eugenol cement (IRM), they concluded that the MTA had significantly lower marginal leakage and had greater sealing ability and was more stable than amalgam and IRM [12]. MTA does not show any signs of solubility, except when using an excessive amount of liquid during mixing which may increase its solubility. In 2013, it was found that when MTA was exposed to water, it released Ca(OH)2 which could be responsible for the induction of cementogenesis [13].
Because of the current situation in Syria, dentists find it difficult to perform sedation or general anaesthesia when treating uncooperative children, therefore, instead of Root Canal Treatment (RCT) for open apex, that needs a highly cooperative child [14], which may not be the case, dentists in Syria are trying to find alternatives, by using MTA and PRF pulpotomy as cheaper alternative options.
Thus, the aim of the study was to compare and evaluate the treatment outcomes of the pulpotomy procedure in the first immature molars with irreversible pulpitis using PRF or MTA by monitoring the teeth for one year.
Materials and Methods
This was a randomised double-blinded study. The study was approved by the Ethics Committee of the Damascus University, Damascus, Syria with registration number (No. 789/02.01.2018). The procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975 that was revised in 2013.
Sample estimation was done using the G*Power 3.1.9.4 computer program, a minimum sample of 11 teeth in each group was set to ensure that an adequate sample size was collected to show 80% power, an effect size of 1.1 and 5% level of significance.
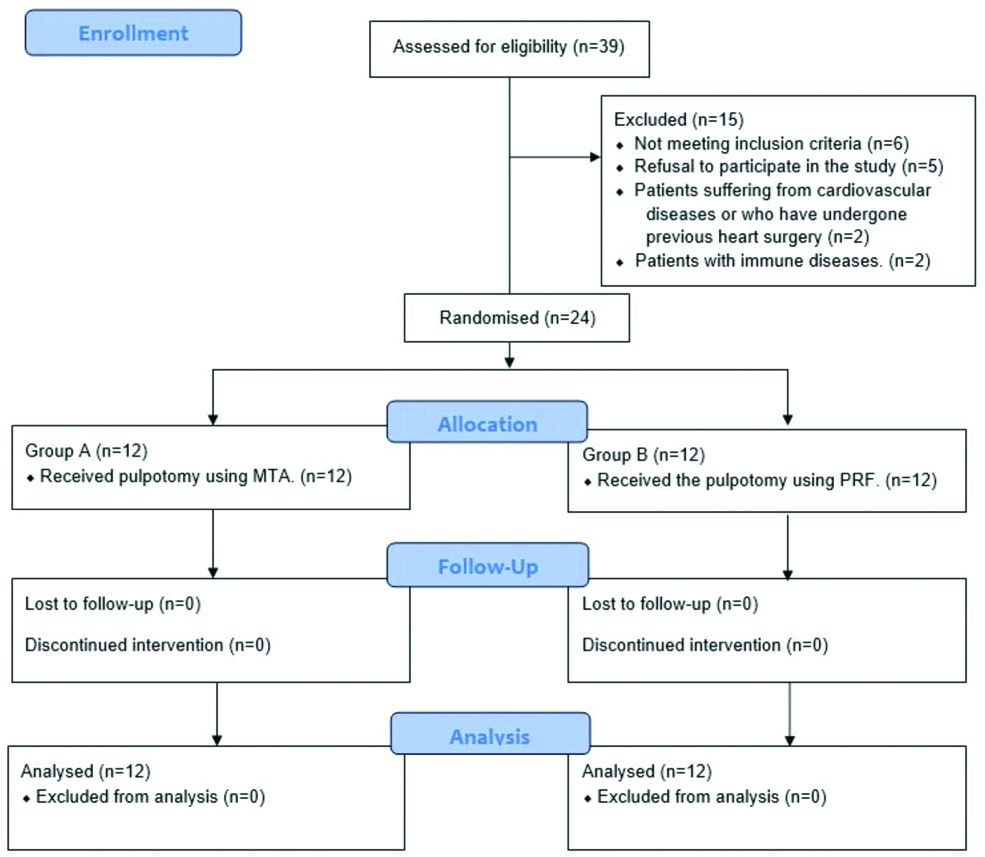
Eligible population for this study were 33 children with 39 teeth suffering from irreversible pulpitis. Fifteen teeth were excluded. The research sample thus consisted of 24 first permanent immature molars in 20 children between the age group of 6-8 years referred to the Department of Paediatric Dentistry (Damascus University, Syria) from January 2018 to June 2019, each of them had at least one first permanent immature molar Stage 9 according to Nolla’s method (Root almost complete; open apex) [15] with irreversible pulpitis [Table/Fig-1]. Informed consent was obtained from all the children’s parents.
Flow diagram of study design (n=number of teeth).
Inclusion Criteria
The presence of caries exposed pulp on first permanent immature molars causing long and continuous episodes of pain (irreversible pulpitis).
No signs of pulp necrosis, such as swelling, fistula, or pathological tooth movement.
Absence of radiological signs (bifurcation lesions-internal or external resorption-calcified root canals-apical lesion-periapical abscess).
The tooth must be restorable after the treatment is completed.
Exclusion Criteria
Patients with immune diseases.
Patients suffering from cardiovascular diseases or who have undergone previous heart surgery.
Refusal to participate in the study.
The research sample (teeth) was randomly divided into two equal groups, using block randomisation method, according to the treatment method followed: pulpotomy with PRF, pulpotomy using MTA.
Group A: Comprised of 12 first permanent immature molars in which the pulpotomy was conducted using PRF [Table/Fig-2]. PRF was prepared using Dohan’s procedure [9]. After centrifugation three layers were formed; upper layer platelet poor plasma; middle layer consisting of PRF clot and in the base, a layer of red blood cells.
Platelet-Rich Fibrin (PRF) clot.

Group B: Included 12 first permanent immature molars in which pulpotomy were performed using MTA (PD™ MTA White) according to the following method:
Local or regional anaesthesia was given with a 1.8 mL, 2% ampoule of lidocaine with 1:100000 adrenaline.
The tooth was isolated with rubber dam (Hygenic® Dental Dam non latex, Coltène/Whaledent GmbH + Co. KG).
Caries was removed using a high-speed turbine with a spherical diamond bur and cooling with water. After removal of the caries completely, the ceiling of the cavity was removed with the same bur, making sure to remove the entire ceiling of the cavity.
The cavity was washed with a saline solution (0.9% w/v) {THE ARABIAN MEDICAL CO (THAMECO)} to make sure the removal of residue.
Coronary pulp was removed by using a large spoon curette or using a large spherical micromotor bur.
The pulp chamber was rinsed completely with a saline solution (0.9% w/v) and it was ensured that the entire coronary pulp is removed, then the bleeding was controlled with a moist cotton ball and the canal orifices were sqeezed for 10-15 minutes, then the materials for pulpotomy were uesd as followed:
Group A: After stopping the bleeding, PRF membrane was placed over the orifices of the canals, and then the MTA plug was applied with a wet cotton ball over it. The cavity was packed with glass ionomer cement (Promedica Dental Material GmbH). On next day, the cement and cotton ball were removed then a thick layer of IRM (Dentsply Sirona Canada) was placed followed by amalgam (BMS DENTAL) restoration [14].
Group B: After stopping the bleeding, MTA material was mixed on a glass slab using a plastic spatula to achieve putty like paste consistency. This mix was covered with moistened cotton pellet to prevent dehydration. The mix was placed in the bottom of the pulp chamber, above the canal orifices, and closed with a wet cotton ball. The cavity was packed with glass ionomer cement, and on the next day the cement was removed with the cotton and then a thick layer of IRM was placed and amalgam restoration was done [16].
Evaluation after Completion
Treatment were evaluated thoroughly after periodic clinical and radiological examination of the treated tooth after one month, six months and 12 months by three specialists to assess the success of the treatment. Both the specialists who evaluated the results and patients were blinded to the treatment given.
Pulpotomy success criteria were:
The absence of spontaneous or evoked pain.
The absence of redness, gingival swelling, or fistula after treatment.
The absence of a pathological tooth movement.
The absence of radio-translucency around the apex or in the bifurcation region.
No internal or external root resorption [4].
Upon clinical failure of treatment, a traditional RCT was performed and an MTA plug was placed in order to complete the apex formation.
The treatment outcome was determined clinically and radiologically in terms of success or failure at two phases (after six months, after one year) for every first permanent premature molar in the research sample.
Statistical Analysis
Data was recorded by a separate dentist to prevent investigator bias. The data was statistically analysed using SPSS version 20.0. Data were presented as frequency and percentage. Chi-square test was conducted to study the significance of differences in the frequency of treatment success or failure between the treatment groups at six months and one year follow-up. McNemar’s test showed any statistically significant difference in treatment outcomes between the two studied time periods (after six months and after one year) in the research sample according to the treatment methods used in group A and B.
Results
A total of 24 first permanent immature molars in 20 children between 6-8 years of age and a mean age of 6.9±0.6 years. Teeth were randomly divided into two equal groups according to the treatment method: 1) pulpotomy with PRF; and 2) pulpotomy using MTA.
The results of the Chi-square test showed that there were no statistically significant differences in treatment success or failure between the treatment groups using PRF and the treatment group using MTA in the research samples at six months [Table/Fig-3] and one year [Table/Fig-4].
The results of monitoring treatment success and failure in the research sample according to the treatment method used six months post-treatment. Chi-square Test: *p<0.05 (significant).
| The treatment method used | The number of the first permanent premature molars | Degree of freedom | χ2 value | p-value |
|---|
| Failure (n/%) | Success (n/%) | Sum (n/%) |
|---|
| Treatment using PRF (Group A) | 3 (25.0%) | 9 (75.0%) | 12 (100%) | 1 | 3.429 | 0.064 |
| Treatment using MTA (Group B) | 0 (0.0%) | 12 (100%) | 12 (100%) |
The results of monitoring treatment success and failure in the research sample according to the treatment method used one year post-treatment. Chi-square Test: *p<0.05 (significant).
| The treatment method used | The number of the first permanent premature molars | Degree of freedom | χ2 value | p-value |
|---|
| Failure (n/%) | Success (n/%) | Sum (n/%) |
|---|
| Treatment using PRF (Group A) | 7 (58.3%) | 5 (41.7%) | 12 (100%) | 1 | 0.168 | 0.682 |
| Treatment using MTA (Group B) | 6 (50.0%) | 6 (50.0%) | 12 (100%) |
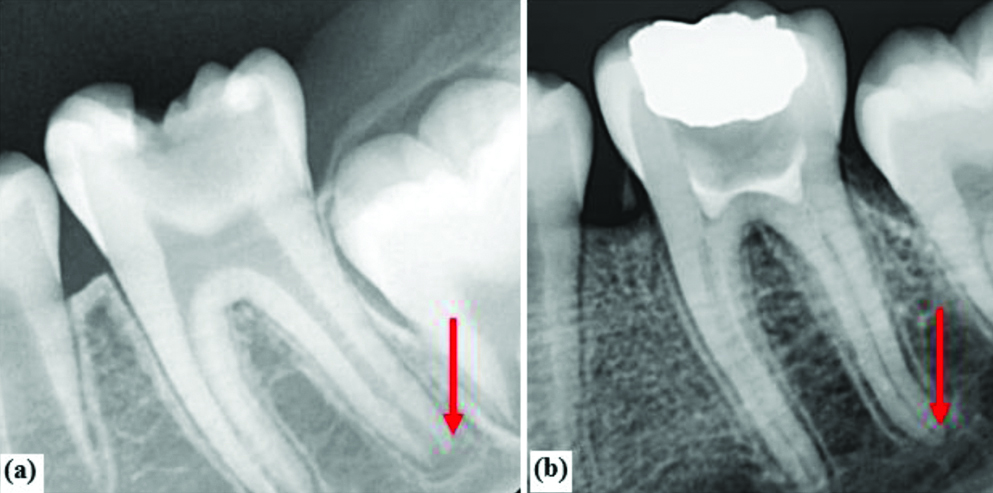
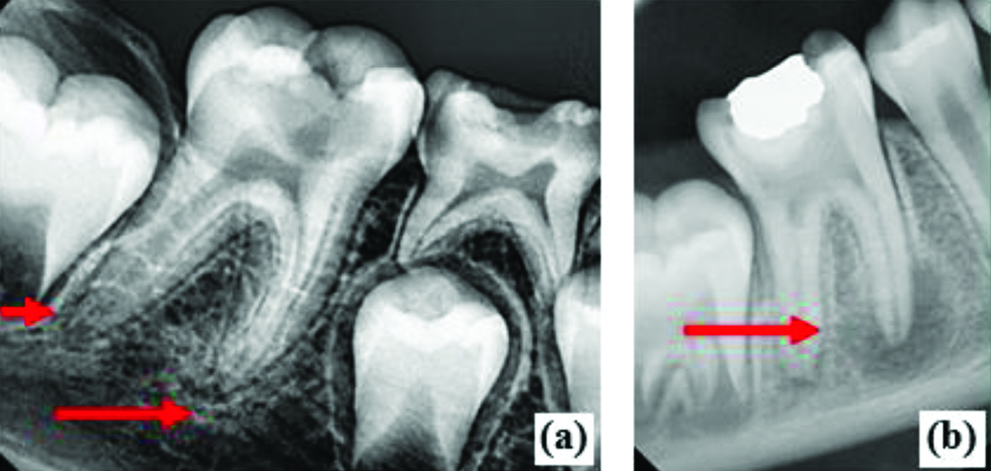
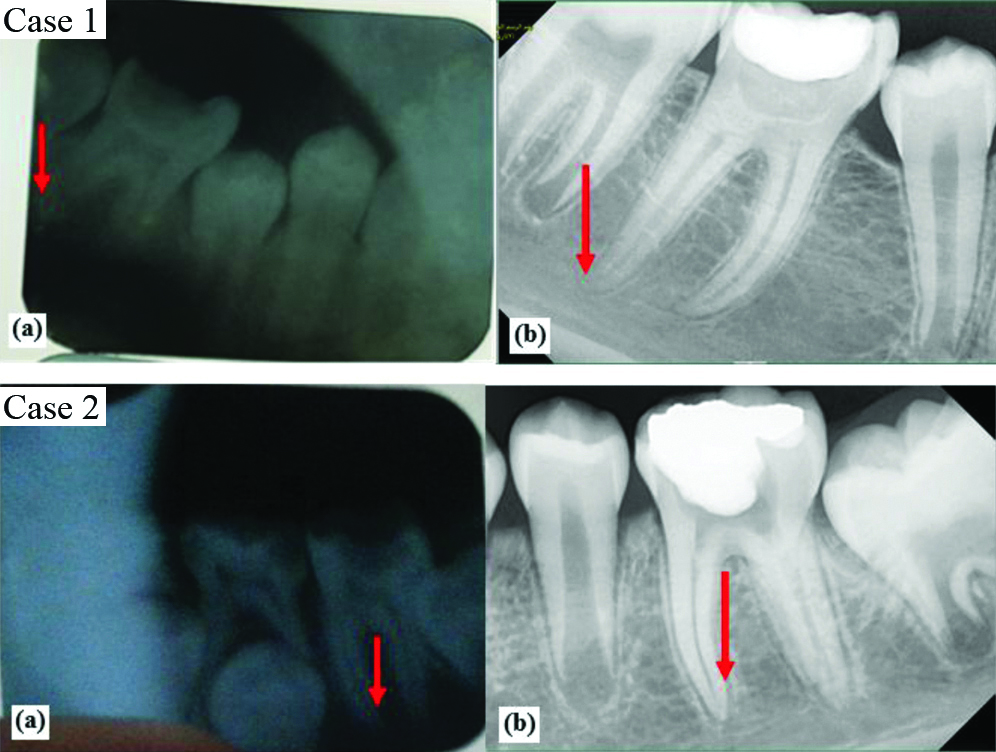
[Table/Fig-5,6 and 7] shows some radiographic images of treatment success and failure from both groups.
Successful case of MTA group: (a) Preoperative intraoral periapical radiograph showing (arrow) an open apex of mandibular first permanent immature molar; (b) Follow-up intraoral periapical radiograph after one year showing (arrow) permanent molar’s apical foramen closed.
Failure case of PRF group: a) Preoperative intraoral periapical radiograph showing open apices of mandibular first permanent immature molar; b) Follow-up intraoral periapical radiograph after one year showing (arrow) periapical radiolucency of mesial root of mandibular first permanent immature molar.
Two successful cases of PRF Group: a) Preoperative intraoral periapical radiograph showing (arrow) open apexes of mandibular first permanent immature molar; b) Follow-up intraoral periapical radiograph after one year showing (arrow) permanent molar’s apical foramen closed.
McNemar’s test showed the significant differences of treatment success and failure between the two studied time periods (after six months, after one year) in the research sample according to the treatment method used [Table/Fig-8].
The results determining treatment success and failure in the research sample according to the method of treatment followed and the time period studied.
| The method of treatment followed | Studied time period | Number of successful first permanent premature molars | Total number of the first permanent premature molars | McNemar’s test |
|---|
| PRF treatment Group A | 6 months later | n=9 | 12 (100%) | p=0.125 |
| After 1 year | n=5 |
| MTA treatment Group B | 6 months later | n=12 | 12 (100%) | p=0.031* |
| After 1 year | n=6 |
*p<0.05 statistically significant
For group A, it was noted there was no statistically significant difference in the success or failure of the treatment between the two studied time periods (after six months and after one year) p=0.125.
In Group B, statistically significant differences were found between six months and one year follow-up results p=0.031, thus indicating there was a greater failure with increasing duration of follow-up.
Discussion
To the best of our knowledge, this study was the first to investigate differences between the use of MTA and PRF in permanent immature molars with irreversible pulpitis. Case reports [16-18] were previously published emphasising clinical significance of PRF but no comparison has been done between the use of MTA and PRF in permanent immature molars. Patidar S et al., carried out a study on 50 primary molars comparing using MTA and PRF as pulpotomy agents and concluded that PRF can be used successfully as an appropriate alternative material in pulpotomy of primary teeth. They emphasised that further investigation with histological assessment is needed [14]. They also mentioned that they did not encounter any uncooperative behaviour from children, howsoever young while collecting blood sample or performing procedure [14], which was in agreement with the present study observation.
The present study partly agreed with Dujana R and Al-halabiah H, that pulpotomy as a treatment option using either MTA or PRF had acceptable clinical success rates and the differences were not significant. Dujana R and Al-halabiah H, treated asymptomatic permanent teeth using PRF, whereas in the index study the comparison was done between MTA and PRF in symptomatic permanent immature molars with irreversible pulpitis [19].
The present study also agreed with Prasanthi NNVD et al., who showed two successful cases using PRF as a pulpotomy medicament of symptomatic permanent fully developed molars with irreversible pulpitis with a two-year observation period and concluded that there was reasonable evidence to carry out pulpotomy as a possible alternative treatment in mature permanent teeth with pulpitis [20], however the case reports did not show any comparative evaluation with other agents in permanent immature molars as the present study did.
Keswani D et al., studied 70 permanent premature molars in which they performed pulpotomy using MTA and PRF, and they found that the success rate of PRF after six months and a year of application was higher than the success rate of MTA, p=0.846 [21]. This is different from what present study stated, where the success rate of the MTA after six months and a year was higher. However, the difference between the two groups was not significant statistically in both studies.
Whereas, Keswani D et al., had performed pulpotomy on premature permanent molars with reversible pulpitis [21], in the present study, pulpotomy was performed on permanent premature molars with irreversible pulpitis.
Kumar V et al., observed that when they performed pulpotomy using the MTA and PRF materials on the permanent molars with irreversible pulpitis, there were no statistically significant differences between the use of the two materials when studying them at six months and 12 months, (p=0.135 at six months, 0.717 at 12 months) [5].
This differs with what the index study says, success rates 100% and 50% at six months and 12 months for the MTA group with no statistically significant difference observed between groups (p>0.05) and the reason might be due to the fact that Kumar V et al., had studied it on permanent, fully developed and with irreversible pulpitis, while this study dealt with permanent premature molars with irreversible pulpitis [5].
Limitation(s)
The present study had a small sample size. Conducting a comparative gender analysis and follow-up over a longer period of time should be considered in future studies.
Conclusion(s)
Although the application of MTA material to perform pulpotomy of the first permanent immature molars had slightly higher success rates than performing pulpotomy using the PRF, there were no statistically significant differences between the use of MTA and PRF.
Conducting a comparative histological study between the use of MTA and PRF for pulpotomy of the first permanent immature molar pulp.
*p<0.05 statistically significant
[1]. Aguilar P, Linsuwanont P, Vital pulp therapy in vital permanent teeth with cariously exposed pulp: A systematic reviewJ Endod 2011 37(5):581-87.10.1016/j.joen.2010.12.00421496652 [Google Scholar] [CrossRef] [PubMed]
[2]. Hargreaves KM, Berman LH, Cohen’s pathways of the pulp expert consult 2015 11th edMosbyElsevier Health Sciences:928 [Google Scholar]
[3]. Baggett FJ, Mackie IC, Worthington HV, An investigation into the measurement of the working length of immature incisor teeth requiring endodontic treatment in childrenBr Dent J 1996 181(3):96-98.10.1038/sj.bdj.48091708810108 [Google Scholar] [CrossRef] [PubMed]
[4]. Jeeruphan T, Jantarat J, Yanpiset K, Suwannapan L, Khewsawai P, Hargreaves KM, Mahidol study 1: Comparison of radiographic and survival outcomes of immature teeth treated with either regenerative endodontic or apexification methods: A retrospective studyJ Endod 2012 38(10):1330-36.10.1016/j.joen.2012.06.02822980172 [Google Scholar] [CrossRef] [PubMed]
[5]. Kumar V, Juneja R, Duhan J, Sangwan P, Tewari S, Comparative evaluation of platelet-rich fibrin, mineral trioxide aggregate, and calcium hydroxide as pulpotomy agents in permanent molars with irreversible pulpitis: A randomised controlled trialContemp Clin Dent 2016 7:512-18.10.4103/0976-237X.19410727994420 [Google Scholar] [CrossRef] [PubMed]
[6]. Kiran NK, Mukunda KS, Tilak Raj TN, Platelet concentrates: A promising innovation in dentistryJ Dent Sci Res 2011 2(1):50-61. [Google Scholar]
[7]. Choukroun J, Adda F, Schoeffer C, Vervelle A, PRF: An opportunity in perio-implantologyImplantodontie 2000 42:55-62. [Google Scholar]
[8]. Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C, Dohan SL, Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part IV: Clinical effects on tissue healingOral Surg Oral Med Oral Pathol Oral Radiol Endod 2006 101(3):e56-60.10.1016/j.tripleo.2005.07.01116504852 [Google Scholar] [CrossRef] [PubMed]
[9]. Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part I: Technological concepts and evolutionOral Surg Oral Med Oral Pathol Oral Radiol Endod 2006 101(3):e37-44.10.1016/j.tripleo.2005.07.00816504849 [Google Scholar] [CrossRef] [PubMed]
[10]. Gupta V, Bains VK, Singh GP, Mathur A, Bains R, Regenerative potential of platelet rich fibrin in dentistry: Literature reviewAsian J Oral Health Allied Sci 2011 1:23-28. [Google Scholar]
[11]. Wu CL, Lee SS, Tsai CH, Lu KH, Zhao JH, Chang YC, Platelet-rich fibrin increases cell attachment, proliferation and collagen-related protein expression of human osteoblastsAust Dent J 2012 57(2):207-12.10.1111/j.1834-7819.2012.01686.x22624763 [Google Scholar] [CrossRef] [PubMed]
[12]. Lee SJ, Monsef M, Torabinejad M, Sealing ability of a mineral trioxide aggregate for repair of lateral root perforationsJ Endod 1993 19(11):541-44.10.1016/S0099-2399(06)81282-3 [Google Scholar] [CrossRef]
[13]. Vitti RP, Prati C, Sinhoreti MAC, Zanchi CH, Silva MGSE, Ogliari F, Chemical-physical properties of experimental root canal sealers based on butyl ethylene glycol disalicylate and MTADent Mater 2013 29(12):1287-94.10.1016/j.dental.2013.10.00224183503 [Google Scholar] [CrossRef] [PubMed]
[14]. Patidar S, Kalra N, Khatri A, Tyagi R, Clinical and radiographic comparison of platelet-rich fibrin and mineral trioxide aggregate as pulpotomy agents in primary molarsJ Indian Soc Pedod Prev Dent 2017 35(4):36710.4103/JISPPD.JISPPD_178_1728914251 [Google Scholar] [CrossRef] [PubMed]
[15]. Nolla CM, The development of permanent teeth (Doctoral dissertation, University of Michigan) 1952 :254-66. [Google Scholar]
[16]. Subash D, Shoba K, Aman S, Bharkavi SK, Revitalization of an immature permanent mandibular molar with a necrotic pulp using platelet-rich fibrin: A case reportJ Clin Diagn Res 2016 10(11):ZD210.7860/JCDR/2016/21793.890228050518 [Google Scholar] [CrossRef] [PubMed]
[17]. Hiremath H, Saikalyan S, Kulkarni SS, Hiremath V, Second-generation platelet concentrate (PRF) as a pulpotomy medicament in a permanent molar with pulpitis: A case reportInt Endod J 2012 45(1):105-12.10.1111/j.1365-2591.2011.01973.x22077790 [Google Scholar] [CrossRef] [PubMed]
[18]. Lee KY, Lee SH, Lee NY, Vital pulp therapy using platelet-rich fibrin in an immature permanent toothJ Korean Acad Pediatr Dent 2013 40(2):120-26.10.5933/JKAPD.2013.40.2.120 [Google Scholar] [CrossRef]
[19]. Dujana R, Al-halabiah H, Clinical and radiographic study to investigate the effect of platelet-rich fibrin membranes (PRF) application as partial pulpotomy agentInt J Appl Dent Sci 2020 6(1):74-89. [Google Scholar]
[20]. Prasanthi NNVD, Simpsy GS, Chittem J, Sajjan GS, Biological approach in the management of permanent molars with irreversible pulpitis using platelet-rich fibrin as a pulpotomy medicament: Case reports with 2-year follow-upJ Inter Discip Dentistry 2018 8(1):30-34.10.4103/jid.jid_54_17 [Google Scholar] [CrossRef]
[21]. Keswani D, Pandey RK, Ansari A, Gupta S, Comparative evaluation of platelet-rich fibrin and mineral trioxide aggregate as pulpotomy agents in permanent teeth with incomplete root development: A randomised controlled trialJ Endod 2014 40(5):599-605.10.1016/j.joen.2014.01.00924767550 [Google Scholar] [CrossRef] [PubMed]