Diabetes Mellitus (DM) is a group of disorders that occur when the pancreas produce little or no insulin or the body develops resistance to insulin, or both, leading to an increase in blood glucose levels [1]. When not appropriately managed, diabetes can result in complications affecting many parts of the body leading to several microvascular disorders like nephropathy, retinopathy, neuropathy, and macrovascular complications like atherosclerosis and stroke [2]. Diabetic Retinopathy (DR) is the one of the commonest and leading causes of vision loss among middle-aged adults worldwide, which may instigate ocular manifestations together with changes in corneal Endothelial Cell Density (ECD), corneal thickness, and intraocular pressure [3] A previous study has estimated that diabetic patients are 25 to 30 times more susceptible to vision loss than non-diabetics belonging to the same age group [4]. Diabetes affects all the layers of the cornea, as the diabetic cornea is susceptible to many abnormalities such as corneal endothelial damage, recurrent corneal erosions, persistent epithelial defects, punctate epithelial keratopathy, impaired corneal sensitivity, ulcers, slowed wound repair, and superficial keratitis [5]. The common issue affecting almost 70% of diabetic patients is corneal damage [6]. In the past, it has been reported that diabetic patients showed alterations in corneal endothelium morphology like decreased corneal endothelial cell density, thicker corneas with increased endothelial permeability, lesser corneal sensitivity, and elevated corneal autofluorescence [7].
Thus, we performed this study to compare corneal Endothelial Cell Density (ECD), Corneal Thickness (CCT), Co-efficient of Variation (CV), and hexagonality in diabetic patients and non-diabetic patients. Also, the association between these corneal changes and the duration of DM and glycemic control (HbA1c level) were observed.
Materials and Methods
This was a prospective, hospital-based study. The study was approved by the institutional ethics committee of the hospital in September 2016 (HMH/IEC/2016/EA06) and adhered to the tenets of the Declaration of Helsinki, Seventh revision. All the participants signed detailed consent forms after explanation of the possible risks and benefits of the study before beginning investigations. All patients were recruited from the ophthalmology department at Hindu Mission Hospital, Tambaram, Chennai, by consecutive sampling method from 24th September 2016 to 29th March 2018.
Inclusion criteria: A total of 155 patients were included in the study, of which 100 were type 2 diabetic and 55 controls. The diagnosis of type 2 DM was based on the criteria of the World Health Organisation (WHO) [1]. All patients with fasting blood sugar of less than 100 mg/dL were included as controls in the study.
Exclusion criteria: The patients with high myopia, retinal degenerations, history of intraocular surgery, patients with corneal dystrophy such as Fuch’s endothelial dystrophy and Posterior polymorphous dystrophy, other corneal degenerations, pterygium, history of contact lens wear, glaucoma or any chronic uveitis, were excluded.
Also the patients with an active or previous eye infection or inflammation, any previous trauma, lid abnormalities like entropion, trichiasis, chronic use of any eye drops or known systemic drugs that can potentially interfere with tear formation (such as hormone replacement therapy and antihistamines), patients with other systemic comorbidities like neurological diseases, renal abnormalities, rheumatoid arthritis, and pregnancy were excluded.
Age, sex, duration of diabetes, most recent HbA1c value, latest fasting, and postprandial blood sugars, systolic and diastolic blood pressures, blood urea, serum creatinine were recorded. In this study, both eyes of each patient were tested and recorded, but only the right eye of all patients was included for statistical analysis. All subjects underwent a complete ophthalmic examination that included visual acuity assessment using the digital Snellen eye chart, refraction using an auto-refractometer (Topcon, CT-80, Tokyo, Japan). The patient was seated in a chair in front of the EM-3000 Specular Microscope. The patient was then asked to place his or her chin on the chin rest with the forehead rested comfortably. The patient was instructed to keep to looking at the red light from the microscope for a few seconds until the instrument automatically took a clear image of the corneal endothelium simultaneously measuring the Corneal thickness at the same time. Changes in the endothelium morphology were studied by measuring factors like ECD, CV, and percentage of hexagonal cells. The measurements were done in the right eye of all patients first and the average of three readings was recorded for the study. Diabetic patients were further divided into groups according to the duration of diabetes (< or ≥ 3 years) and HbA1c% (< or ≥ 7%).
Statistical Analysis
The data were analysed using a statistical program (SPSS V.16.0, Chicago, IL). The results were expressed as means±standard deviation. An independent t-test was performed to compare the mean of endothelial characteristics between study subjects and the control group and also between duration of diabetes and HbA1c levels. A p-value of less than 0.05 was considered statistically significant.
Results
The present study included 155 participants, comprising of 100 diabetic patients (52 males/48 females) and 55 controls (13 males/42 females). The age range of the diabetic group was 18-73 years and for the control group it was 36-58 years. There was no statistical significance in terms of age, urea, creatinine, and IOP between study subjects and controls. Whereas, the other baseline characteristics like blood pressure FBS, PPBS, HbA1c were significantly higher in the diabetic group when compared to controls [Table/Fig-1].
Baseline demographics of study patients.
| Parameters | Study subjects (100) | Control group (55) | p-value |
|---|
| Age (years) | 50.63±10.24 | 45.54±5.7 | 0.7 |
| Systolic BP (mmHg) | 128±26.28 | 113±20.67 | <0.001** |
| Diastolic BP (mmHg) | 81±14.50 | 73±10.74 | <0.001** |
| FBS (mg/dL) | 173±79.46 | 99±6.19 | <0.001** |
| PPBS (mg/dL) | 251±108 | 125±4.3 | <0.001** |
| HbA1C (%) | 7.6±3.05 | 4.3±0.36 | <0.001** |
| Urea (mg/dL) | 23±18.2 | 25.4±3.41 | 0.5 |
| Creatinine (mg/dL) | 1.0±1 | 0.8±0.1 | 0.2 |
| IOP (mmHg) | 17.13±2.23 | 16.53±2.5 | 0.1 |
Data represented as Mean±Standard Deviation, p<0.001** denotes statistically highly significant
FBS: Fasting blood glucose; PPBS: Post prandial blood glucose; IOP: Intraocular pressure; BP: Blood pressure; p-value <0.05 to be considered as significant
When morphological characteristics of endothelial cells and CV were compared between diabetic patients and the control population, the former group showed lower reduction in ECD and CV (p>0.05) than the latter group but the difference observed was not significant. A significant difference in corneal thickness (p-value=0.01) and hexagonality (p-value <0.001) were also observed between both groups [Table/Fig-2].
Morphologic characteristics of endothelial cell.
| Parameters | Diabetic (100) | Non-diabetic (55) | p-values |
|---|
| Endothelial cell density (ECD), cells/mm2 | 2534±277.3 | 2568±213 | 0.39 |
| Central corneal thickness, mm | 555±33.7 | 541±33.28 | 0.01* |
| Coefficient of variation (CV) (%) | 40±10.70 | 42.5±18.29 | 0.35 |
| Hexagonality (%) | 45.97±2.00 | 42.7±6.03 | <0.001** |
Data represented as Mean±Standard Deviation, *denotes statistically significant p<0.05
**denotes statistically highly significant p<0.001
When the endothelial cell characteristics were compared between diabetic patients with duration <3 years and those with duration ≥3 years; a difference was observed between groups that were not statistically significant (p>0.05) [Table/Fig-3].
Correlating endothelial cell characteristics with duration of diabetes.
| Parameters | Duration of diabetes <3 years (52) | Duration of diabetes ≥3 years (48) | p-values |
|---|
| Cell density, cells/mm2 | 2540±272.1 | 2527±285.5 | 0.8 |
| Central corneal thickness, mm | 548±30.07 | 555±37.10 | 0.3 |
| Coefficient of variation (%) | 40.11±6.87 | 45.25±25.28 | 0.16 |
| Hexagonality (%) | 45.69±1.91 | 45.27±2.08 | 0.15 |
Data represented as Mean±Standard Deviation; p-value <0.05 to be considered significant
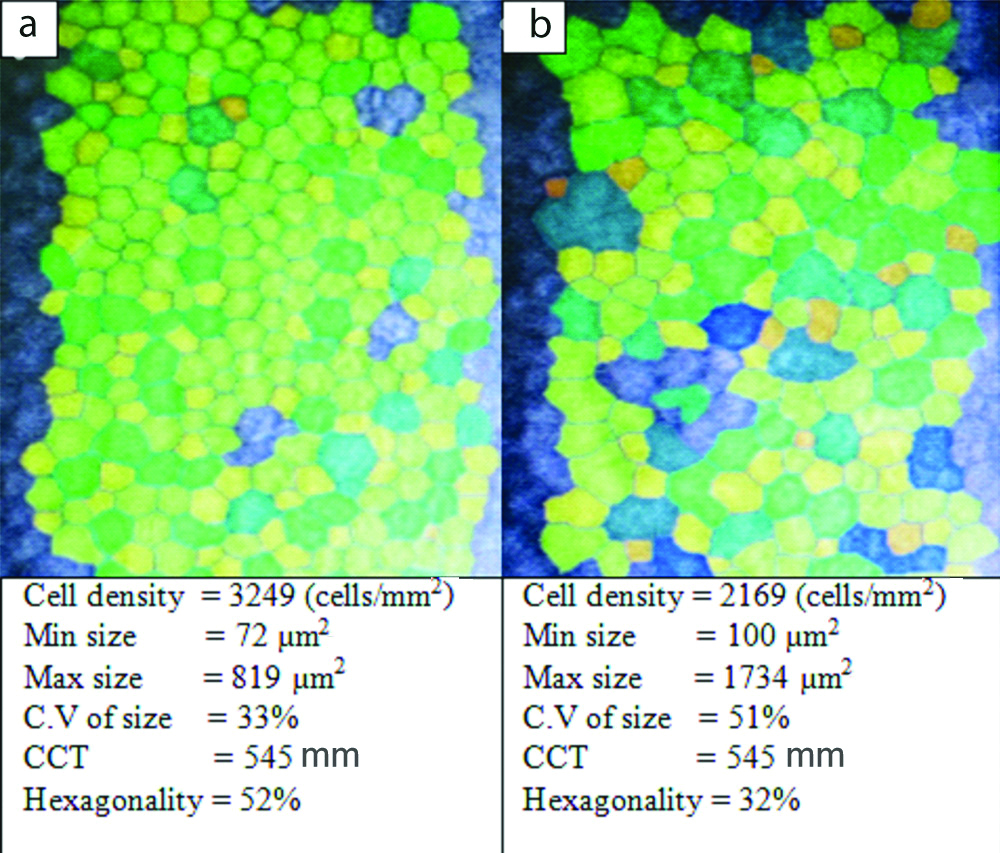
Diabetic patients with HbA1c% <7 had higher ECD, CCT, and hexagonality but not statistically significant than those with HbA1c% ≥7 [Table/Fig-4,5]. The mean of CV was lower in diabetic patients with HbA1c% <7 than in the other group [Table/Fig-4].
Comparing endothelial cell characteristics between the diabetic groups, according to HbA1c%.
| Parameters | HbA1c (%) <7 (44) | HbA1c (%) ≥7 (56) | p-value |
|---|
| Endothelial cell density (ECD), (cells/mm2) | 2533±281.64 | 2531±279 | 0.9 |
| Central corneal thickness (CCT), mm | 553±37.70 | 548±30.02 | 0.4 |
| Coefficient of variation (CV) (%) | 40.86±10.36 | 43.94±22.85 | 0.4 |
| Hexagonality (%) | 46.90±2.30 | 45.90±1.78 | 0.6 |
Data represented as Mean±Standard Deviation; p-value <0.05 to be considered as significant
Photograph of Corneal Endothelium taken by EM-300 Specular Microscopic. a) Normal eye; b) Diabetic eye
Discussion
In this study, the corneal endothelial density was compared amongst the diabetic patients and controls, it was observed that the mean ECD was lower in the former group but the difference obtained was not statistically significant (p<0.05). Several studies found no difference in ECD between diabetic patients and controls. Storr-Paulsen A et al., conducted a study in 235 Caucasians observed no significant difference in ECD between diabetic and non-diabetic patients (p=0.60) [8]. Módis L et al., observed corneal endothelial changes in type 1 and type 2 diabetic patients. They found significant differences only in type 1 diabetic patients in terms of ECD, CCT, and CV, whereas in type 2 diabetic patients there was no difference in ECD when compared to healthy patients [9]. Similarly, no significant differences between the groups were also reported by Hugod M et al., (p=0.78) [10] and Inoue K et al., (p=0.2) [11]. However, the results of the present study were not in agreement with the earlier studies carried out in the Indian population. Where, Minu R et al., reported a significant reduction in ECD in diabetic patients over controls (p-value <0.001) among 200 study participants [12]. Comparable results were also observed by Sudhir RR et al., (p=0.001) and Ahuja S et al., p-value 0.001 signifying that endothelial cells are depleting faster in diabetic patients than the controls [13,14].
Previously published studies suggested that age is a risk factor causing severe corneal endothelial damage in diabetic patients. The present study did not assess the effect of age on corneal endothelial damage as the majority of study participants were of specific age group. So, excluding the effect of age, the present study report decreased ECD in diabetic patients. Similarly, Inoue K et al., in their study suggested that the damage to cornea endothelial cells by diabetes was so severe so that the effect of age can be nullified [15]. In addition to age, several factors have also been studied and found related to corneal endothelial changes such as corneal disorders, contact lens-related disorders, intraocular surgery, refractive surgery, and other eye diseases [16,17].
In the present study, Authors demonstrated that the CCT was significantly thicker in the diabetic group than in the control group, (p-value 0.01). This finding is consistent with other authors (Storr Paulsen A et al., Busted N et al and Choo MM et al.,) who found that diabetic corneas were thicker when compared to controls [8,18,19]. Literature confirms that patients with diabetes have a significant severe corneal endothelial damage which leads to an increase in CCT, which in turn affects the IOP measurements [20]. As the thickness of cornea indirectly informs about the function of the endothelial layer, the mechanism which induces dysfunction of the cornea is probably the decrease in sodium-potassium adenosine triphosphatase (Na+/K+ATPase) [21]. Another possible explanation for increased corneal thickness in diabetic patients is because of the increased stromal swelling pressure which is due to glycosylation of corneal collagen or accumulation of sorbitol [22].
The present study observed a significant reduction in the percentage of hexagonal cells (pleomorphism) and increased CV (polymegathism) between groups, whereas, only hexagonality indicated a statistically significant difference (p-value <0.001) as the corneal endothelium demonstrated less than 50% hexagonality. Similar results were observed by Choo MM et al., who observed increased pleomorphism (p-value <0.01) with unaffected CCT [19]. A study by Shenoy R et al., reported that polymegathism was 12% percent higher in the diabetic group and corneal endothelial cells with 9% pleomorphism which seems to be positively associated with T2DM [23]. This study with regards to the CV of cell size, demonstrated no significant difference between the diabetic patients and control group (p<0.05), this result was agreeable with those obtained by Sudhir RR et al., (p=0.72) [13] and Islam QU et al., (p=0.07) [24]. A decrease in cell density, polymegathism, and pleomorphism are early signs of endothelial disease. It is presumed that this altered morphology and changes in the corneas may be related to sorbitol accumulation within these cells and reduction in ATP production [25].
In the present study, patients with more than 3 years of diabetes showed reduction in cell density, higher coefficient variation and thicker cornea with no difference in the hexagonality percentage between the two groups. However, the observed reduction between groups was not statistically significant. According to the severity of diabetes, Islam QU et al., Lee JS et al., and Briggs S et al., reported reduced average cell size and thicker corneas in diabetic patients with more than 10 years duration than for diabetic less than 10 years [24,26,27]. However, this difference cannot be compared because other authors have reported a longer duration of DM, in contrast to this study where patients with a long duration of DM were less in number.
This study did not find any association between HbA1c levels and corneal parameters like ECD, corneal thickness, hexagonality and coefficient variation. These results were similar to those of Sudhir RR et al., and Inoue K et al., confirming that there was no significant relationship between HbA1c and corneal endothelial damages in diabetic patients over controls [13,15].
In line with previous studies authors suggest that the result obtained based on a single measurement of HbA1c only reflects the cumulative glycaemic history of the preceding two to three months. Evaluation based on a single measurement is challenging, so continuous monitoring of HbA1c would have helped to overcome the limitation of HbA1c and corneal characteristics [13,15].
Limitation(s)
The present study, being a hospital-based cross-sectional study, had its own limitations. Having a larger sample size and more diverse range in age could have possibly helped us to visualise the effect of age on endothelial damage. Longer follow-ups with more than 10 years of diabetic age would have helped us to observe if the duration of diabetes modifies corneal characteristics and the strength of this study would be adding information to a specific ethnic group.
Conclusion(s)
The present study demonstrated that patients with diabetes had a marginal increase in corneal thickness, and a higher frequency of pleomorphism compared to control subjects. But in terms of ECD and co-efficient variation, no difference was observed between groups. Whereas duration of DM (< or ≥ 3 years) and HbA1c levels (< or ≥ 7%) were not associated significantly with any of the corneal endothelial parameters. The study suggests that diabetes itself would be a major cause of corneal damage, as the difference observed between the diabetic and non- diabetic groups was evident so that the other effects can be nullified.
Data represented as Mean±Standard Deviation, p<0.001** denotes statistically highly significant
FBS: Fasting blood glucose; PPBS: Post prandial blood glucose; IOP: Intraocular pressure; BP: Blood pressure; p-value <0.05 to be considered as significant
Data represented as Mean±Standard Deviation, *denotes statistically significant p<0.05
**denotes statistically highly significant p<0.001
Data represented as Mean±Standard Deviation; p-value <0.05 to be considered significant
Data represented as Mean±Standard Deviation; p-value <0.05 to be considered as significant