Chronic Obstructive Pulmonary Disease (COPD) is defined as a “clinically treatable disease distinguished by respiratory symptoms that are persistent, and is associated with a significant airflow limitation that is chronic and not completely reversible” [1]. It includes emphysema, chronic bronchitis and small airway disease. It is ranked fourth among the major causes of mortality on the global stage at present [2] and is expected to occupy the third position by 2020 [3]. In patients with moderate to severe COPD, exacerbation of symptoms has a devastating impact on the progression of disease as well as quality of life. Hence, a comprehensive approach including prevention, prompt diagnosis and immediate management of the exacerbation is required. According to The American Thoracic Society and European Respiratory Society, AECOPD is defined as an “acute change in the patient’s cough, sputum or dyspnoea that is beyond normal variability and that is sufficient to warrant a change in therapy” [4]. Multiple parameters appear to influence outcomes in AECOPD, such as length of hospital stay, need for mechanical ventilation and mortality. Due to this, the exact estimation of prognosis in such patients is difficult. In patients with stable form of COPD, there are well known scores such as BODE (Body mass index, airway Obstruction by FEV1, Dyspnoea by Modified Medical Research Council (MMRC) score, Exercise tolerance by 6 minute walking distance) index which have been rigorously scrutinised [5]. For episodes of acute exacerbation, many indices have been proposed to predict the outcomes. DECAF [6] score and BAP 65 [7] score are two of these prognostic indices. Parameters in BAP 65 score are BUN, altered mental status, pulse rate and age >65 years. Parameters in DECAF score are dyspnoea grade, eosinopenia, consolidation, acidemia and atrial fibrillation. For the physician in the emergency room, in a resource-poor country like India where there is a large volume of patients, it is necessary to have a set of guidelines regarding the requirement of mechanical ventilation and ICU admission so as to use the available sparse resources in a judicious manner. While the variables of DECAF score are obtained in a well-equipped emergency room setting, BAP 65 score is a relatively easy score to calculate in patients admitted with AECOPD. Hence, comparison of the two scores will aid in directing the physician towards logical use of resources, thereby decreasing deaths and significant morbidity.
We therefore aimed to compare the performance of BAP 65 and DECAF scores in accurately predicting need for mechanical ventilation and mortality in patients with AECOPD.
Materials and Methods
This prospective, observational study was conducted from February 2018 to September 2019 in a university hospital situated in a semi-urban area after obtaining Institutional Ethics Committee clearance (1337/IEC/2018). Sample size was calculated assuming the proportion of people with “COPD” to be 37% as per the study by Gupta D et al., using the formula N=4 PQ/L2 [8].
Patients of either sex diagnosed with AECOPD in General Medicine and Pulmonology Out Patient Department (OPD) and Emergency Room (ER) and older than 40 years were included in the study at the time of admission to the hospital using convenience sampling. Subjects who were already on domiciliary ventilation support, less than 40 years of age and unwilling to give consent were excluded from the study. All the eligible subjects were recruited into the study consecutively until the required sample size was obtained.
After obtaining informed consent, patient demographics and history was recorded and a complete physical examination was performed. Score of <14 on Glasgow Coma Scale (GCS) or physician assessment as disoriented, drowsy was taken to indicate altered mental status [9]. All routine investigations were performed. BUN, total and differential White Blood Cell (WBC) count. ECG, Chest X-ray, arterial blood gas analysis were done on all patients. Blood urea >43 mg% and BUN >20 mg% (as per hospital reference range) were taken as abnormal. The two scores were calculated with information obtained. Following this all patients were followed by a daily visit until discharge or death. The outcome of the patient was noted as either improved (Survivor) or death (Non- Survivor). The number of patients needing mechanical ventilation was also noted.
The two scores were then compared on the basis of the outcome, using statistical analysis.
Statistical Analysis
Statistical analysis was done using SPSS software version 23. If the variables were continuous, they were represented as “Mean±SD” and if the variables were of uneven distribution they were expressed as median. All the categorical variables were stated as frequencies and percentages. Continuous variables having a normal distribution with respect to the outcome were compared using “Student’s t-test”, while those having a non-normal distribution were compared by “Mann-Whitney U test”. Categorical data across the various groups was evaluated by “Chi-square test or Fisher’s-exact test”. ROC analysis was computed to decide on the actual cut-off value for DECAF score and BAP 65 score. The AUC, sensitivity and specificity were computed so as to compare the diagnostic efficacy of DECAF score and BAP 65 score. For all the tests, p<0.05 was deemed to be significant.
Results
170 patients were admitted with AECOPD were included in the study. Maximum numbers were in the age group of 61-70 years (37.1%) [Table/Fig-1]. A total of 108 (63.5%) were male and 62 (36.5%) were female.
| Age (years) | Frequency | Percentage |
|---|
| 40-50 | 52 | 30.6 |
| 51-60 | 22 | 12.9 |
| 61-70 | 63 | 37.1 |
| 71-80 | 23 | 13.5 |
| >80 | 10 | 5.9 |
| Total | 170 | 100.0 |
Of 170 patients, 23 (13.5%) patients died while 147 (86.5%) patients survived. A total of 48 patients required non-invasive ventilation and 30 required invasive ventilation and 23 expired. Among the total of 170 subjects with AECOPD, 86 were smokers and 42 had history of significant biomass exposure. Sputum culture sensitivity was positive in 76 (44.7%) patients and negative in 94 patients (55.3%).
Older age, longer duration of disease, increased smoking pack years and increased duration of hospital stay were associated significantly with death. Previous hospital admissions in the preceding year were also associated with bad outcome [Table/Fig-2].
Comparison of baseline characteristics of two groups.
| Variables | Survivors (n=147) | Non-survivors (n=23) | p-value* |
|---|
| Age (years) | 59.28±12.11 | 69.1±12.9 | 0.002 |
| Sex (Male/Female) | 90/57 | 18/5 | 0.16 |
| Duration of illness (Median) (years) | 9 (2-14) | 10 (8-18) | 0.04 |
| Smoking pack years | 12.13±14.67 | 31.87±17.88 | <0.0001 |
| Duration of hospital stay (days) | 7.84±2.87 | 11.9±5.09 | 0.001 |
| No. of hospital admissions in past one year | 0.93±0.57 | 2.78±1.38 | <0.0001 |
(*Independent t-test. For gender, Chi-square test); p<0.05 was deemed to be significant.
Among basic laboratory investigations, haemoglobin value, Total Leucocyte Count (TLC) and BUN level at baseline were all significantly different between survivor and non-survivor groups [Table/Fig-3].
Comparison of laboratory parameters.
| Variables | Survivors (N=147) | Non-survivors (n=23) | p-value* |
|---|
| Haemoglobin (g/dL) | 12.04±1.34 | 11.33±1.86 | 0.03 |
| Total leucocyte count/mm3 | 10698.98±3724.78 | 14935.09±4264.65 | <0.001 |
| Blood urea nitrogen (mg/dL) | 21.49±11.02 | 31.57±19.02 | 0.02 |
(*Independent t-test); p<0.05 was deemed to be significant.
For DECAF score, dyspnoea grade 5a and atrial fibrillation did not significantly differ between the two groups [Table/Fig-4].
| Variable | Survivors | Non-survivors | p-value* |
|---|
| Dyspnoea grade 5a | 28 (19%) | 3 (13%) | 0.6 |
| Dyspnoea grade 5b | 19 (12.9%) | 20 (87%) | 0.0005 |
| Eosinopenia (<0.05×109/l) | 9 (6.1%) | 9 (39.1%) | 0.0005 |
| Consolidation | 60 (40.8%) | 18 (78.3%) | 0.001 |
| Acidemia (ph <7.3) | 27 (18.4%) | 20 (87%) | 0.0005 |
| Atrial fibrillation | 11 (7.5%) | 4 (17.4%) | 0.125 |
(*chi-square test); p<0.05 was deemed to be significant.
All parameters of the BAP 65 score showed significant difference between survivor and non-survivor groups [Table/Fig-5].
| Variable | Survivors (N=147) | Non-survivors (N=23) | p-value |
|---|
| Blood urea nitrogen >25 mg % | 36 (24.5%) | 14 (60.9%) | 0.0005 |
| Altered mental status | 29 (19.7%) | 9 (39.1%) | 0.038 |
| Pulse >109/min | 25 (17.0%) | 8 (34.8%) | 0.045 |
| Age >65 years | 57 (38.8%) | 17 (73.9%) | 0.002 |
(chi-square test); p<0.05 was deemed to be significant.
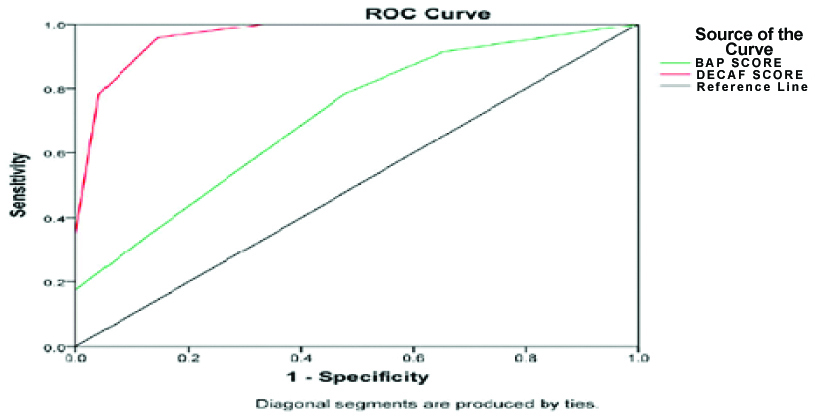
The ROC curve shows that, for the outcome of mortality, both DECAF and BAP 65 scores were valid scores (AUC 0.965 and 0.712, respectively). But positive predictive value and sensitivity was more with DECAF. It showed a higher chance of prediction of mortality when compared to the BAP 65 score [Table/Fig-6a,b].
Comparison of scores with respect to mortality.
| DECAF score | BAP 65 score |
|---|
| Area under curve (95% Confidence interval) | 0.965 (0.936-0.993) | 0.712 (0.600-0.823) |
| Sensitivity (%) | 78.26% | 34.78% |
| Specificity (%) | 95.92% | 87.07% |
| Positive predictive value (%) | 75% | 29.63% |
| Negative predictive value (%) | 96.58% | 89.51% |
| p-value | 0.0005 | 0.001 |
| Accuracy (%) | 87.09% | 60.93 |
ROC curve with respect to mortality.
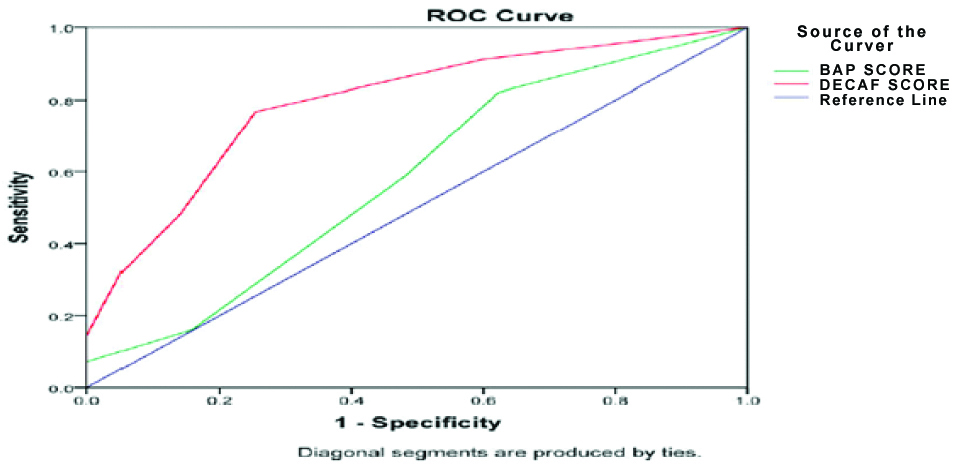
ROC curves for both scores showed validity for both with respect to the need for mechanical ventilation. However, the BAP 65 score as a predictor for mechanical ventilation had an AUC of 0.583, which is just above the baseline required for a score to be valid while DECAF had AUC of 0.791 [Table/Fig-7a,b].
Comparison of scores with respect to need for mechanical ventilation.
| DECAF score | BAP 65 score |
|---|
| Area under curve (95% Confidence interval) | 0.791 (0.718-0.865) | 0.583 (0.494-0.671) |
| Sensitivity (%) | 32.14% | 16.07% |
| Specificity (%) | 94.74% | 84.21% |
| Positive predictive value (%) | 75% | 33.33% |
| Negative predictive value (%) | 73.97% | 67.13% |
| p-value | 0.0005 | 0.081 |
| Accuracy (%) | 63.44% | 50.14% |
ROC curve for mechanical ventilation.
Discussion
The study population comprised 170 patients admitted with AECOPD. The majority were males (n=108, 63.5%). 37.1% of patients were in the age group 61-70 years. Older age group is a known risk factor for AECOPD [10,11]. 23 (13.1%) patients succumbed. The mortality rate is lower when compared to a study done by Jayadev A et al., wherein the mortality rate was around 16.8% [12], but higher than those reported by Steer J et al., and Shorr AF et al., (10.4% and 4%, respectively) [6,7]. In the present study, 39.4% of the subjects required ICU care. Out of the 67 patients transferred to ICU, 23 patients died. A total of 78 patients required mechanical ventilation, while 30 (17.6%) required invasive ventilation. The frequency of people requiring invasive mechanical ventilation in this study was higher when compared to Mohan A et al., where 15.5% of the subjects required invasive mechanical ventilation [13]. Smoking burden increased the risk of death due to AECOPD [Table/Fig-2]. This is similar to a Korean study which found that in people aged more than 60 years who have been smoking for greater than 20 years, the risk of having severe COPD is high [14]. Another risk factor for death was higher rate of hospital admission in the year prior to current admission. A retrospective study of 900 patients in Spain found that previous severe exacerbations were associated with new AECOPD [15]. Also, Slenter R et al., showed in another retrospective study that one year mortality for hospitalised patients with AECOPD was 27.7% [16]. Significant difference in TLC between survivors and non-survivors points to the role of infection as an important prognostic factor in the estimation of mortality.
Predictors of Outcome
Many scores have been devised to predict outcomes in AECOPD. BAP 65 and DECAF are two such well-validated scores. Echevarria C et al., showed robust internal validity (AUC 0.83) and external validity (AUC 0.82) for the DECAF score in predicting mortality [17]. A study from Southern India found that BAP 65 score correlated well with mortality and need for mechanical ventilation with a sensitivity of 71.9% and specificity of 86.9% [18]. Two studies, one from Tamil Nadu and one from Karnataka looked at the ability of DECAF scores in predicting outcomes depending on the severity of the scoring, but did not compare it to other scores [19,20]. A study from Kerala, on the other hand, looked at independent predictors of mortality in AECOPD and concluded that anaemia could be a risk factor [21].
Sangwan V et al., conducted a pilot study with 50 patients comparing DECAF and BAP 65 scores [22]. They opined that both scores did well. Another Indian study from Kannur, Kerala compared multiple scoring systems (DECAF, BAP 65, CAPS, APACHE II and CURB-65) with 150 patients and concluded that a DECAF score ≥2 with an AUROC of 0.729 correlated best with mortality [23]. A retrospective Spanish study compared CURB 65, DECAF and BAP 65. Curb 65 had the highest sensitivity and NPV, while BAP 65 performed least well [24]. On the other hand, two studies from Egypt had different results. Yousif M et al., in a comparison of BAP 65, DECAF, modified DECAF and 2008 scores found that BAP 65 had the highest AUROC (0.861) to predict mortality [25]. Sweed RA et al., compared APACHE II, BAP 65, 2008 and CAPS scores and found that while all correlated significantly with mortality, APACHE II and 2008 scores best predicted need for mechanical ventilation. Furthermore, previous need for mechanical ventilation was the best predictor of need for mechanical ventilation in current admission [26]. Study done by Steer J et al., found that every variable of DECAF score was a self-determining, prognosticator of mortality [6]. In the current study, all variables except atrial fibrillation and Grade 5a dyspnoea were significantly correlated. On the other hand, all variables of BAP 65 were significantly higher in non-survivors than survivors.
In the current study, both DECAF and BAP 65 scores were valid for prediction of mortality (AUC 0.965 and 0.712, respectively) and need for mechanical ventilation. But DECAF had higher sensitivity and higher chance of prediction of mortality than the BAP 65 score. AUC for BAP 65 score as a predictor for mechanical ventilation was 0.583 which is just above the baseline required for a score to be valid whereas the AUC for DECAF score was found to be 0.791 making it a better predictor than BAP 65 score with respect to need of mechanical ventilation.
The sheer number of scoring systems available for AECOPD makes it difficult to choose one for regular clinical application. Many of the above studies have not only validated the DECAF score, but also has given stratifications for predicting mortality in this population. It is easily applicable in centres with medium to higher facilities and should probably be the score used to triage these patients. On the other hand, in resource-poor settings and rural areas, BAP 65 would still be the choice. The small number of studies available also demonstrates the need for well-planned multicentric studies to guide us, given the diversity and size of the Indian population.
The strength of this study lies in the number of patients recruited and the real-life setting in a large university hospital.
Limitation(s)
The following are the limitations of the study. Firstly, admission to ICU and decision to ventilate was physician-based and not protocol-based. Secondly, co-morbidities of the patients may have had a confounding effect on the final outcomes. Thirdly, stratification on basis of age (which is a risk factor) or individual scores was not done and lastly selection bias in the form of patients with mild exacerbation refusing to get admitted or refusal for admission due to other logistical reasons.
Conclusion(s)
In AECOPD, duration of illness, smoking and previous hospitalisations as well as infection trigger to the episode are correlated with poor mortality outcome. Both DECAF score and BAP 65 score are valid scores with respect to likelihood of need for mechanical ventilation and mortality outcome. DECAF score better predicts the need for mechanical ventilation in AECOPD.
(*Independent t-test. For gender, Chi-square test); p<0.05 was deemed to be significant.
(*Independent t-test); p<0.05 was deemed to be significant.
(*chi-square test); p<0.05 was deemed to be significant.
(chi-square test); p<0.05 was deemed to be significant.