Tetralogy of Fallot is characterised by ventricular septal defect, narrowing of the right ventricular outflow tract (pulmonary stenosis), overriding aorta (dextroposition of the aorta), and right ventricular hypertrophy. It constitutes for 5-10% of congenital cardiac defects, with an incidence of 0.24-0.56 per 1000 live births. It is often caused due to anterior displacement of the conotruncus, resulting in an unequal division of conus into a small anterior right ventricular portion and large posterior left ventricular portion. Aortic overriding occurs due to incomplete closure of the septum [3]. Pulmonary stenosis is usually observed at the valvular level or the infundibulum. It is observed in 7.4% of newborns and is associated with tetralogy of fallot, anomalous pulmonary venous return, Noonan syndrome, maternal rubella, atrial septal defect, and supravalvular aortic stenosis [3]. The prenatal diagnosis based on ultrasound findings may be inadequate for the parents to decide on pregnancy termination. Therefore, a multidisciplinary approach through clinicians, geneticists, paediatricians, radiologists, and pathologists is required for the diagnosis of anomalies as well as the application of suitable testing. A specialist paediatric pathologist can provide significant information about the possible risk of recurrence [4]. Interaction with the obstetrician and foetal cardiologist provides valuable information about the pre-autopsy cardiac status. The correlation of autopsy findings with antenatal ultrasound findings during intrauterine life is an important component of medical education and quality improvement, in addition to the direct benefit for the patient’s family [5]. There are very few autopsy studies available in the literature [6,7]. Only a few have compared the autopsy findings with the antenatal ultrasound findings [7,8].
The present study aims to determine the pattern of distribution of cardiovascular anomalies through autopsy and also an association between maternal factors and congenital anomalies, and an association between autopsy and ultrasound findings.
Materials and Methods
This was a descriptive cross-sectional study conducted on 50 stillborn foetuses, which were obtained from the Department of Obstetrics and Gynaecology, in a JSS Medical College and Hospital, Mysuru, Karnataka, India. The duration of the study period was two years, which started in July 2016 and was completed by June 2018. This study was approved by the Institutional Ethics Committee with the approval number JSS/MC/IEC/02/660/2015-16.
Inclusion criteria: All stillborn foetuses at or above 22 weeks and foetuses whose parents gave informed consent were included.
Exclusion criteria: Foetuses with gestational age less than 22 weeks and autolysed foetuses were excluded.
Written consents were obtained from either of the parents for all the stillborn foetuses before conducting the autopsy. A study proforma was prepared to obtain a detailed history of a mother in terms of maternal age, gestational age, obstetric history includes present pregnancy details including date of last menstrual period, GPLA status (Gravida, Para, Living and Abortions), previous pregnancy history including history of any congenital anomaly, mode of termination, history of medical disorders, socioeconomic status of parents, consanguinity, the possible cause of foetal death, and antenatal ultrasonography report. The content and construct validity was ensured through the subject experts in the study proforma.
The various morphometric parameters of stillborn foetuses including birth weight, Crown-Rump Length (CRL), and Rump Heel Length (RHL), head, chest, and abdominal circumferences were measured. The placenta and umbilical cord were examined for any gross abnormality. The external anomalies of the stillborn foetus were noted. The cardiovascular anomalies and associated other organ malformations were studied in detail. Each foetus was coded with the unique autopsy number for the identification of congenital anomalies. Each stillborn foetus was classified based on birth weight, gestational age, maternal age, gravidity of the mother, and socioeconomic status of parents. The socioeconomic status was calculated according to the modified Kuppuswamy’s socioeconomic scale [9].
Foetal Autopsy Procedure
Stillborn foetuses were fixed in 10% formalin and formalin was injected in the thoracic cavity, abdominal cavity, and cranial cavity for fixation of the organs. An autopsy was performed by the standard procedure [8]. A longitudinal incision was started from the suprasternal notch up to the pubic symphysis and it was followed by a horizontal incision to retract the skin flap. The thoracic and abdominal cavities were dissected, and any deviation from the normal anatomy was noted and photographed. The heart was examined by a method adopted by Virchow that is, along the direction of the flow of blood [5]. Sections were taken from the heart specimen and subjected to histopathological examination. Routine Haematoxylin and Eosin (H&E) staining was done and microphotographs were taken in cases with congenital cardiovascular anomalies diagnosed on the histopathological study.
Statistical Analysis
Data collected was entered in MS Excel 2010 and analysed using SPSS version 22 to obtain relevant statistics. Descriptive measures like percentages, mean, and Standard Deviation (SD) were calculated. Fisher’s-Exact test was done to find the association between maternal diabetes and cardiovascular anomalies. The results were interpreted as statistically significant at p<0.05.
Results
Out of the total 50 foetuses studied, cardiovascular anomalies were present in five cases (10%). Among the five foetuses, four were male and one was female and the ratio of male to female is 4:1. The ventricular septal defect was the most common cardiovascular anomaly observed. The other anomalies were tetralogy of Fallot, atrial septal defect, and pulmonary stenosis [Table/Fig-1]. Among five foetuses, four were isolated cardiovascular anomalies and one foetus with tetralogy of Fallot was associated with the unascended left polycystic kidney.
Distribution of cardiovascular anomalies among stillborn foetuses.
| Cardiovascular anomalies | Number (n) | Percentages (%) |
|---|
| Ventricular septal defect | 2 | 40 |
| Tetralogy of fallot | 1 | 20 |
| Atrial septal defect | 1 | 20 |
| Pulmonary stenosis | 1 | 20 |
| Total | 5 | 100 |
Among five foetuses of cardiovascular anomalies, three were born to primigravida, and one each foetus was born to the second gravida, and third gravida. But there was no previous history of any congenital anomaly among them. Among 50 stillborn foetuses studied, 27 foetuses were terminated by normal vaginal delivery and 23 foetuses were terminated by performing Lower Segment Caesarean Section (LSCS). Twenty-two mothers had a history of medical disorders which includes eight diabetes, seven hypertension, five hypothyroidism, and two infections. The history of consanguinity was present in 10 (20%) mothers.
The maximum number of stillborn foetuses was between 500-1000 grams followed by 1001-1500 grams [Table/Fig-2].
Distribution of birth weight among the stillborn foetuses studied.
| Birth weight (in grams) | Number (n) | Percentages (%) |
|---|
| 500-1000 | 29 | 58 |
| 1001-1500 | 11 | 22 |
| 1501-2000 | 3 | 6 |
| 2001-2500 | 4 | 8 |
| >2501 | 3 | 6 |
| Total | 50 | 100 |
The number of stillborn foetuses was maximum between 22-26 weeks of gestational age followed by 27-30 weeks [Table/Fig-3].
Distribution of gestational age among the stillborn foetuses studied.
| Gestational age (in weeks) | Number (n) | Percentages (%) |
|---|
| 22-26 | 20 | 40 |
| 27-30 | 15 | 30 |
| 31-34 | 9 | 18 |
| 35-38 | 4 | 8 |
| >39 | 2 | 4 |
| Total | 50 | 100 |
The number of stillborn foetuses was a maximum between 26-30 years of the maternal age group followed by 21-25 years [Table/Fig-4]. The number of stillborn foetuses was observed maximum in the primigravida followed by the second gravida [Table/Fig-5]. The number of stillborn foetuses was observed maximum in the lower middle class followed by the upper middle class [Table/Fig-6].
Distribution of maternal age among the stillborn foetuses studied.
| Maternal age (in years) | Number (n) | Percentages (%) |
|---|
| <20 | 3 | 6 |
| 21-25 | 19 | 38 |
| 26-30 | 24 | 48 |
| >31 | 4 | 8 |
| Total | 50 | 100 |
Distribution of gravida of the mother among the stillborn foetuses studied.
| Gravida of the mother | Number (n) | Percentages (%) |
|---|
| Primi | 22 | 44 |
| Second | 17 | 34 |
| Third | 8 | 16 |
| Fourth | 2 | 4 |
| Fifth | 1 | 2 |
| Total | 50 | 100 |
Distribution of socioeconomic status of parents among the stillborn foetuses.
| Socioeconomic status of parents | Number (n) | Percentages (%) |
|---|
| Upper | 1 | 2 |
| Upper middle | 15 | 30 |
| Lower middle | 25 | 50 |
| Upper lower | 7 | 14 |
| Lower | 2 | 4 |
| Total | 50 | 100 |
Two cases of a ventricular septal defect were observed. In a male foetus of 23 weeks gestation, ventricular septal defect showed a deficiency of about 3 mm in the membranous part of the interventricular septum [Table/Fig-7].
Ventricular septal defect in a male foetus of 23 weeks gestation (The circle represents the ventricular septal defect).

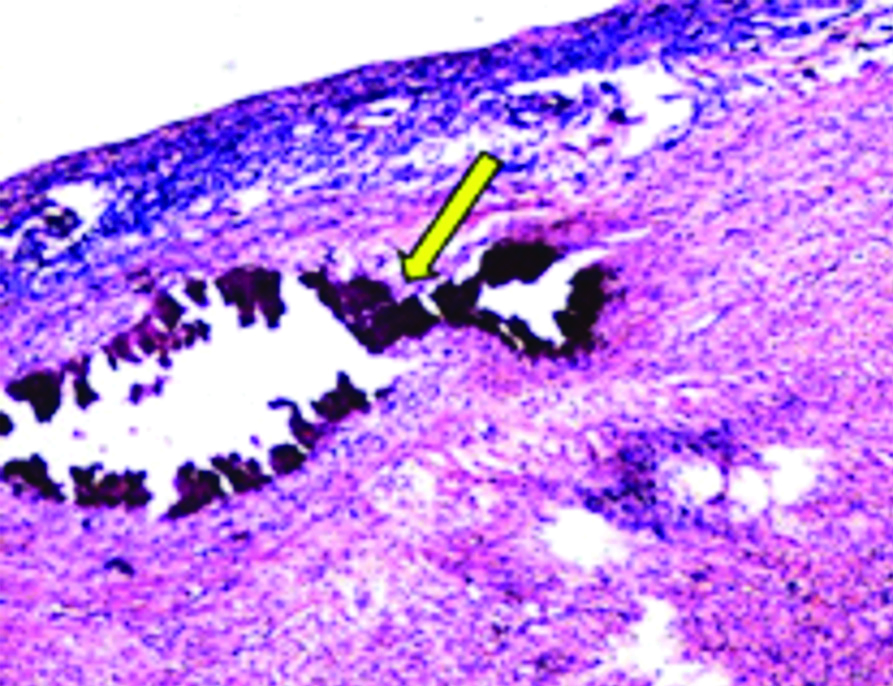
In a female foetus with 29 weeks of gestation, ventricular septal defect with cardiac calcification was noted in the autopsy. The gross cut section of the cardiac specimen showed chalky white discoloration measuring 0.2 to 0.3 mm involving all the layers of the heart. On routine H&E staining, it showed basophilic deposits [Table/Fig-8].
Microphotograph showed cardiac calcification in a female foetus of 29 weeks gestation and routine H&E stain (100X) showing basophilic deposits (The arrow represents the cardiac calcification).
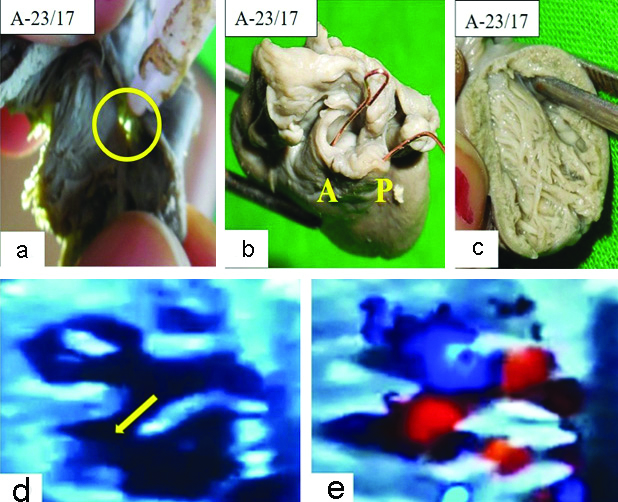
In a male foetus of 24 weeks of gestation with tetralogy of Fallot, ventricular septal defect showed a deficiency of about 4 mm in the membranous part of the interventricular septum seen [Table/Fig-9a], overriding of the aorta, pulmonary stenosis of about 2 mm was observed [Table/Fig-9b]. The interior of the right ventricle was visualised [Table/Fig-9c]. An antenatal ultrasound showed the overriding of the aorta with membranous ventricular septal defect [Table/Fig-9d] and the aorta was filled by both right ventricle and left ventricle [Table/Fig-9e].
a) A case of tetralogy of Fallot showing a defect in membranous part of the interventricular septum (The circle represents the ventricular septal defect). b) Overriding of the Aorta (A) and Pulmonary stenosis (P) noted, and c) Demonstration of the interior of the right ventricle in a male foetus of 24 weeks gestation. d) Ultrasound image showing overriding of the aorta with membranous ventricular septal defect (The arrow represents the membranous ventricular septal defect). e) Aorta is being filled by both right ventricle and left ventricle in a case of tetralogy of Fallot.
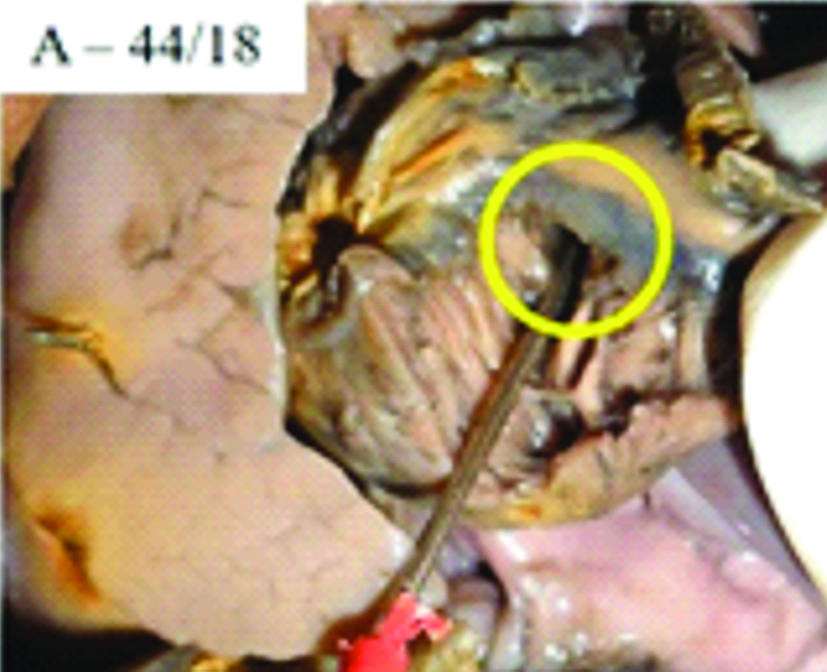
A case of atrial septal defect showed a deficiency of about 3 mm in the interatrial septum in a male foetus of 29 weeks gestation [Table/Fig-10].
Atrial septal defect in 29 weeks male foetus (The circle represents the atrial septal defect).
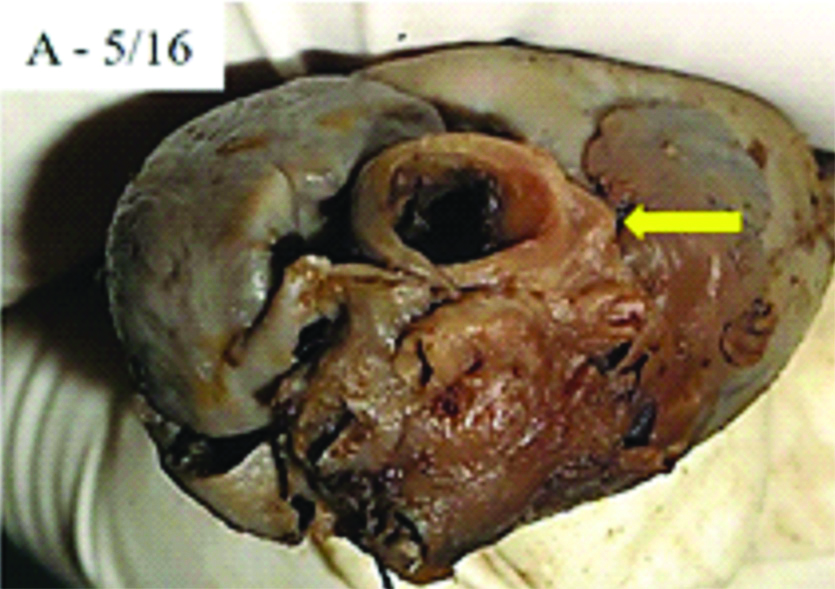
A case of pulmonary stenosis was observed in a male foetus of 24 weeks gestation [Table/Fig-11].
A case of pulmonary stenosis in 24 weeks male foetus (The arrow represents the pulmonary stenosis).
Fisher’s-exact test is a statistical significance test, to find out the association between two categorical variables for small-sized samples [10]. This test showed a significant association between maternal diabetes and cardiovascular anomalies [Table/Fig-12].
Association between maternal diabetes and cardiovascular anomalies.
| Major system involved | Diabetes | Fisher’s-Exact test |
|---|
| Present | Absent | Total | χ2 | p-value |
|---|
| CVS | 3 | 2 | 5 | 14.048 | 0.016* |
CVS: Cardiovascular system; *Significant at p<0.05
The autopsy confirmed the antenatal ultrasound findings in 40 (80%) of the cases. There were significant additional findings observed in 7 (14%) cases and ultrasound diagnosis was completely changed in 3 (6%) cases, after the final autopsy procedure. Ultrasound findings along with the additional findings noted in the autopsy and autopsy changed the primary diagnosis of ultrasound findings in a total of 10 (20%) cases are mentioned [Table/Fig-13].
Differences noted between ultrasound findings and autopsy findings.
| Serial No. | Autopsy No. | Ultrasound findings | Additional findings noted in the autopsy | Autopsy changed the primary diagnosis |
|---|
| 1. | A-03/16 | Holoprosencephaly | Low set ears, amniotic band on the right arm, amputated fingers and toes due to amniotic bands | - |
| 2. | A-14/16 | Omphalocele major, kyphoscoliosis | Left lower limb hypoplasia. | - |
| 3. | A-22/17 | Congenital talipes equinovarus | Polydactyly, Intrauterine growth retardation | - |
| 4. | A-23/17 | Tetralogy of Fallot | Unascended left polycystic kidney. | - |
| 5. | A-44/18 | Congenital diaphragmatic hernia | Atrial septal defect | - |
| 6. | A-45/18 | Ventricular septal defect | Cardiac calcification noted in all the three layers of the heart | - |
| 7. | A-48/18 | Occipital meningoencephalocele | Intrauterine growth retardation | - |
| 8. | A-18/17 | Meningomyelocele | - | Meningocele |
| 9. | A-41/18 | Encephalocele | - | Placental insufficiency |
| 10. | A-47/18 | Bilateral hydronephrosis | - | Infantile polycystic kidney disease |
Discussion
The incidence of congenital cardiovascular anomalies shows a wide variation as reported by different studies. Most of the studies focus their observations on clinical aspects alone, with minimal information on autopsy findings. The ventricular septal defect has been reported to be the most common cardiac anomaly in various other autopsy studies [1,11-13]. In the present study also, ventricular septal defect was the most common anomaly (40%). It was observed as an isolated lesion and also in association with Fallot’s tetralogy. The cardiovascular anomalies were classified as isolated when the cardiac defect was alone present; associated with congenital disorders of other organs and systems without a syndromic diagnosis; components of chromosomal or genetic syndromes; components of ruptures and others, which are not included by the previous categories. When there was one cardiac defect, the cardiac anomalies were classified as single anomalies. When more than one cardiac defect was present, they were classified as multiple anomalies [13]. Cardiac anomalies were categorised as either conotruncal or non-conotruncal. Conotruncal anomalies include the truncus arteriosus, transposition of the great arteries, tetralogy of fallot, double-outlet right ventricle, and ventricular septal defect with an overriding aorta. The non-conotruncal abnormalities were isolated coarctation of the aorta or with other associated cardiac abnormalities and hypoplastic left or right heart [2]. In the present study, all the cardiovascular anomalies were of conotruncal type.
The frequency of cardiovascular anomalies in the present study was compared with the available literature [Table/Fig-14] [4,7,8,14-17]. The results obtained in the present study are almost similar to other studies.
Frequency of cardiovascular anomalies compared with the available literature [4,7,8,14-17].
| Sl No. | Different authors | Year | CVS anomalies Number/Total Number (n) |
|---|
| 1 | Boyd PA et al., [17] | 2004 | 8/132 |
| 2 | Sankar VH and Phadke SR [14] | 2006 | 4/206 |
| 3 | Andola US et al., [7] | 2012 | 2/44 |
| 4 | Hakverdi S et al., [4] | 2012 | 5/274 |
| 5 | Kapoor K et al., [15] | 2013 | 12/150 |
| 6 | Gole RA et al., [16] | 2014 | 3/100 |
| 7 | Kale PP et al., [8] | 2017 | 7/54 |
| 8 | Present study | 2020 | 5/50 |
Sankar VH and Phadke SR have reported two cases of ventricular septal defect, one case of coarctation of aorta and Ebstein anomaly in their study [14]. Andola US et al., have found two cases of atrial septal defect in their study [7]. Hakverdi S et al., have reported each one case of hypoplastic left heart, truncus arteriosus, hypertrophic cardiomyopathy, Gallen vein malformation, and atrioventricular septal defect [4]. Kapoor K et al., have found 12 (8%) cases of cardiovascular anomalies in their study [15]. Gole RA et al., have reported two cases of atrial septal defect and one case of single ventricle [16]. Kale PP et al., have found each one case each of isolated atrial septal defect, ventricular septal defect with atrial septal defect, atrial septal defect with ventriculomegaly, isolated ventricular septal defect, ventricular septal defect with transposition of great vessels, abnormal aorto-pulmonary communication, and hypoplastic heart syndrome [8]. Padma S et al., have found one case of dextrocardia in their study [18].
Foetal Factors
In the present study, the congenital malformations were more in males than females with male to female ratio being 4:1. Kale PP et al., have found a similar incidence to be more in males (52.63%) with a ratio of 1.25:1 [8]. Andola US et al., have found a male: female ratio of 1:1.5 with female preponderance in their study [7]. Birth weight of stillborn foetuses ranged from 500-2800 grams and a maximum foetuses 29 (58%) were having a birth weight between 500-1000 grams in the present study. Among all the foetuses with congenital malformations, 71.92% were having low birth weight (ranging from 350-1000 grams) for the gestational age. The association between low birth weight and congenital anomalies has been well documented [8]. Gestational age of most of the stillborn foetuses ranged from 22-26 weeks (40%) in the present study. This could be related to termination of pregnancy which is immediately done after detecting congenital anomaly on ultrasonography. Kale PP et al., have found maximum foetuses were having a gestational age of 20-24 weeks (63.15%) in their study [8].
Maternal Factors
In the present study, maximum number of foetuses 24 (48%) were born to mothers in the age group of 26-30 years. About 22 (44%) were born to primigravida followed by the second gravida in 17 foetuses (34%). Kale PP et al., have found most of foetuses 39 (68.42%) were born to mothers in age group of 20-24 years and 50.87% mothers were primipara in their study [8]. Hence, meticulous observation during anomaly scan for cardiovascular findings must be made in primigravida itself to avoid future catastrophes. The number of stillborn foetuses was observed maximum in the lower middle class 25 (50%) followed by the upper middle class in 15 (30%), according to modified Kuppuswamy’s socioeconomic scale. Kapoor K et al., have found 34% cases belonging to upper lower class [15]. History of consanguinity was observed in 10 mothers (20%) in the present study. In four mothers history of consanguinity was present (7.02%) out of all congenitally malformed cases [8]. There was a significant association between maternal diabetes and cardiovascular anomalies in the present study.
Maternal illnesses such as diabetes and hypertension usually appear with increasing maternal age. Thus, pregnancies in older women have a higher incidence of diabetes, arterial hypertension, and consequently results in complications, like abortion, congenital anomalies, preeclampsia, eclampsia, and premature births [12]. Especially when a major abnormality has been detected, an important contributor to be mistaken in prenatal diagnosis is the failure to perform a complete examination of the foetus. It is avoided by using a systematic approach by performing a comprehensive anatomic survey of the entire foetus and maintaining a high index of suspicion. Perhaps even in the ideal circumstances, always accurate prenatal diagnosis of all associated abnormalities is not possible [19]. When post-mortem examinations were compared with ultrasound findings, in eight cases (11.43%) the ultrasound findings were incorrect. In 18 cases (25.71%), additional information was obtained on autopsy [6].
The association between the autopsy and ultrasound findings was compared with that of previous studies [Table/Fig-15] [6-8,14,19]. The findings in the present study are almost similar to other studies in the available literature.
Association between the autopsy findings and ultrasound findings [6-8,14,19].
| Sl No. | Authors | Year | Total no. of foetal autopsies | Autopsy confirmed ultrasound findings | Changed primary diagnosis |
|---|
| No change in diagnosis | Additional findings noted in the autopsy |
|---|
| 1. | Yeo L et al., [19] | 2002 | 88 | 27 (30.68%) | 30 (34.09%) | 31 (35.22%) |
| 2. | Sankar VH and Phadke SR [14] | 2006 | 134 | 55 (41.04%) | 77 (57.46%) | 2 (1.49%) |
| 3. | Andola US et al., [7] | 2012 | 35 | 22 (50%) | 13 (29.54%) | 4 (9.09%) |
| 4. | Pradhan R et al., [6] | 2013 | 70 | 44 (62.86%) | 18 (25.71%) | 8 (11.43%) |
| 5. | Kale PP et al., [8] | 2017 | 54 | 27 (47.37%) | 27 (47.37%) | 3 (5.26%) |
| 6. | Present study | 2020 | 50 | 40 (80%) | 7 (14%) | 3 (6%) |
Since the foetal autopsy adds significant information in about 25% of the cases or it changes the prenatal diagnosis in a minimum of 5% of the cases, the foetal autopsy should be routinely recommended in the management of the detected malformations, even in the period of striking progress in prenatal diagnosis. There is an alarming decline of autopsy rate now-a-days because of the centralisation of pathology facilities, changes in clinician’s perception about foetal autopsy is mainly because of the developments in diagnostic imaging methods, or inexperienced persons in foetal medicine providing the poor counseling or absence of a pathologist in the counseling team. Hence, parents are refusing to give consent to the conventional invasive autopsy procedure [20]. The finding of additional malformations as well as changing the diagnosis in some cases, obtained by autopsy studies is beneficial in targeting tests in the following pregnancy. The decline in the autopsy rate about the retention of tissues and organs for diagnostic studies, teaching, and research has been a matter of argument since the adverse publicity concerning autopsies and organ retention [17]. Parents should be provided with complete information and cannot be forced into accepting an autopsy examination. Conveying sensitive information for the procedure in an empathetic way would convince them to opt for the foetal autopsy. Complete information to parents about the potential benefits of the autopsy procedure and risk of recurrence guides them towards informed decision making. This discussion should be done by an appropriately trained professional [17].
Limitation(s)
The major challenge associated with the study was difficulty in carrying out the dissection of the heart and its chambers as well as the great vessels of the heart due to its small size. Also, there were hurdles in obtaining the consent of parents for foetal autopsy. The sample size for the generalisation of findings is probably inadequate.
Conclusion(s)
The ventricular septal defect is the most common cardiovascular anomaly observed was similar to other studies. The major anomalies associated with multiple organs or syndromes get terminated early, the remaining progressed to term. Hence, elucidating the causation underlying the anomaly would be essential considering the burden of child care and management. Hence, the mechanism for cardiovascular anomalies must be searched for, to prevent future affected pregnancies. Antenatal ultrasound should be done in all high-risk pregnancies especially with maternal diabetes to rule out congenital cardiovascular anomalies. If there are any preventive measures for maternal diabetes such as maintaining optimal pre-pregnancy weight etc., those measures should be taken care of to avoid anomalies in the antenatal period and future pregnancies.
Funding statement: This study was funded by the JSS Academy of Higher Education and Research, Mysuru, Karnataka, India.
CVS: Cardiovascular system; *Significant at p<0.05