Hysterectomy is the removal of the uterus. It is the most common gynaecological operation done in females worldwide [1]. It can be a subtotal hysterectomy, where the uterus is partially removed, a total hysterectomy where the uterus with the cervix is removed, or pan hysterectomies where the uterus with the cervix is removed along with a bilateral salphingo-oophorectomy. The uterus is not just an organ for childbearing and removing it impacts a woman’s health in various ways [2].
A hysterectomy has mental, physical, social, economic and psychosexual impact, apart from intraoperative and postoperative complications [1,2]. Choice of the type of hysterectomy done is also important, as some procedures are more likely to damage pelvic floor causing damage to nerve supply of the area which in turn affect the sexual wellbeing [3].
Despite the fact that hysterectomy is a popular surgery it has a number of complications associated with it. The most common are haemorrhage, infection, and injuries to adjacent organs; unintended major surgical procedures and second operations occur in approximately 4% of patients undergoing hysterectomy, while the rates of visceral injuries range between 0.5 to 2% [6]. Microwave endometrial ablation is an established treatment for DUB [7].
There are variations in hysterectomy rates among developed and developing countries rate being higher in developed countries [8]. Apart from the already known impacts, the choice to undergo a hysterectomy also depends on the education of the woman.
Acceptability of hysterectomy among women also depends upon various socio-demographic factors: married, educated, multiparous women postreproductive age was more open to the procedure [6]. Considering that the procedure has a 20-35% life risk, it calls for a thorough justification before consideration [9].
An audit of hysterectomies can help us know the spectrum of histopathological findings and can help recognise malpractice and lacunae in the knowledge or training of health care service providers or nonavailability of newer alternatives for hysterectomy [10].
This audit will therefore help both, the layman in having a better understanding of hysterectomies and the medical fraternity in better decision making and assessment of symptoms. As there are no hysterectomy audits published from India recently, present study may provide a basis for a future audit of the gynaecologic practice and for comparison of this practice with others. Last audit study published on hysterectomies in was in 2014 [5].
Materials and Methods
This was a cross-sectional study which included all elective hysterectomies performed for gynaecological indications conducted at the District Hospital of Kodagu Institute of Medical Sciences, Madikeri from January 2018-June 2019. The Institutional Ethical committee clearance was obtained, IEC number “KoIMS/IEC/4/19-20”
Inclusion and Exclusion criteria:
All cases of hysterectomies except Caesarean peripartal hysterectomies were considered
Case records were reviewed to collect information of patient characteristics, surgical indications, clinical histories, histopathological diagnosis and complications, if any.
Cases were divided in 4 categories based on age:
0-20 years
21-40 years
41-60 years
More than 60 years.
Among all the cases, various indications were reviewed. Histopathology reports were obtained from the Pathology Department. The corresponding patient details, preoperative diagnosis, and type of surgery were obtained from the histopathology request forms from the Medical Records of the Pathology Department. The histopathological findings of the endometrium, myometrium, cervix, ovaries and fallopian tubes were recorded. Findings were tabulated. Then, the data was analysed to know if the hysterectomy was justified.
Results
A total of 238 hysterectomies were performed during 18 months in the District Hospital. Abdominal and vaginal approaches were used.
Types of hysterectomy: Panhysterectomy via abdominal approach was the most common type of hysterectomy (169, 71%) [Table/Fig-1].
Distribution of cases according to route of hysterectomy.
| Type | No. of cases | Percentage (%) |
|---|
| PAH | 169 | 71 |
| VH | 40 | 16.8 |
| TAH | 26 | 10.92 |
| TAH w ULSO | 3 | 1.2 |
| Total | 238 | 100% |
PAH: Pan-abdominal hysterectomy; VH: Vaginal Hysterectomy; TAH: Total abdominal hysterectomy; TAH w ULSO: Total abdominal hysterectomy with unilateral salphingo oophorectomy
Age of the subjects: The ages of the subjects were divided into four categories, 0-20, 21-40, 41-60, >60 years. The mean age of the patients was 46.46 years. The most common age group where hysterectomy occurred was 41-60 years (143, 60.08%) [Table/Fig-2].
Age groups undergoing hysterectomy.
| Age | No. of cases | Percentage (%) |
|---|
| <20 | 0 | 0 |
| 21-40 | 67 | 28.15 |
| 41-60 | 143 | 60.08 |
| >60 | 28 | 11.76 |
| Total | 238 | 100 |
Indication of hysterectomy: The most common indication for hysterectomy was found to be Fibroid uterus (152, 63.87%). This was followed by Uterovaginal prolapse (48, 20.17%) [Table/Fig-3].
Indications for Hysterectomy.
| Indication | No. of cases | Percentage (%) |
|---|
| Fibroid | 152 | 63.87 |
| UV prolapse | 48 | 20.17 |
| DUB | 18 | 7.56 |
| DUB w fibroid uterus | 12 | 5.04 |
| PID | 5 | 2.10 |
| UV prolapse and cystocoele | 3 | 1.26 |
| Total | 238 | 100 |
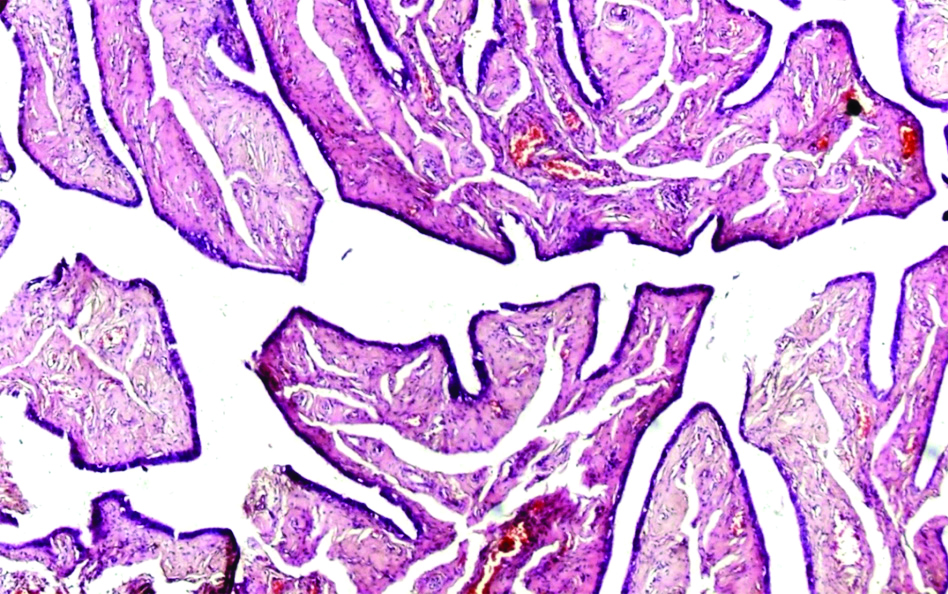
Summary of the histopathological findings of hysterectomies in the present study are given in [Table/Fig-4,5,6,7,8,9,10,11,12 and 13]. The most common endometrial finding was proliferative endometrium (105, 44.12%). Analysis of the myometrial findings revealed that the most common finding was leiomyoma (alone and with adenomyosis) (152, 63.86%) [Table/Fig-4]. Analysis of the cervical findings was done. It was found that chronic cervicitis (133, 55.88%) was the commonest pathological finding in the cervix [Table/Fig-4].
Summary of the histopathological findings in endometrium, myometrium and cervix.
| Histopathological findings In endometrium | No. of cases | Histopathological findings of the myometrium | No. of cases | Histopathological findings in cervix | No. of cases |
|---|
| Proliferative | 105 (44.12%) | Leiomyoma only | 146 (61.34%) | Chronic cervicitis | 133 (55.88%) |
| Secretory | 70 (29.41%) | Leiomyoma with adenomyosis | 6 (2.52%) | Polypoidal endocervicitis | 33 (13.87%) |
| Senile cystic atrophy | 37 (15.55%) | Unremarkable | 48 (20.17%) | Unremarkable | 30 (12.61%) |
| Simple hyperplasia | 11 (4.62%) | Adenomyosis only | 23 (9.66%) | Chronic cervicitis with nabothian cyst | 19 (7.98%) |
| Simple hyperplasia without atypia | 6 (2.52%) | Hyalinised blood vessel | 9 (3.78%) | Papillary endocervicitis | 8 (3.36%) |
| Disordered proliferative | 4 (1.68%) | DUB | 4 (1.68%) | Chronic cervicitis W squamous metaplasia | 8 (3.36%) |
| Simple hyperplasia with atypia | 2 (0.84%) | Monckeberg’s calcification | 1 (0.42%) | Tunnel clusters | 4 (1.68%) |
| Syncytial aggregate | 1 (0.42%) | Calcified blood vessel | 1 (0.42%) | Endocervical glandular hyperplasia | 2 (0.84) |
| Simple hyperplasia W adenomyomatous polyp | 1 (0.42%) | | 238 | Chronic cervicitis W leiomyomatous polyp | 1 (0.42%) |
| Malignant cells in sheets, columns, papillary pattern | 1 (0.42%) | | | | 238 |
| 238 | | | | |
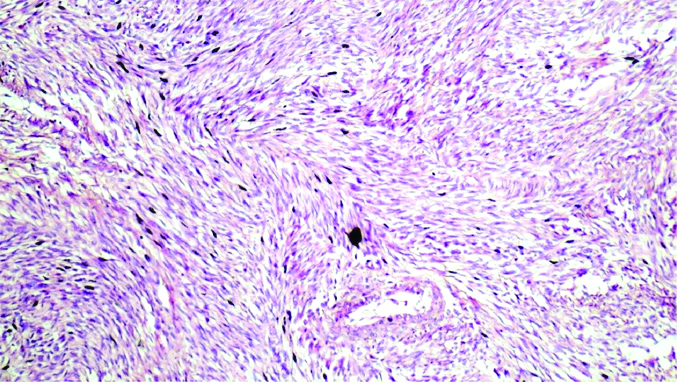
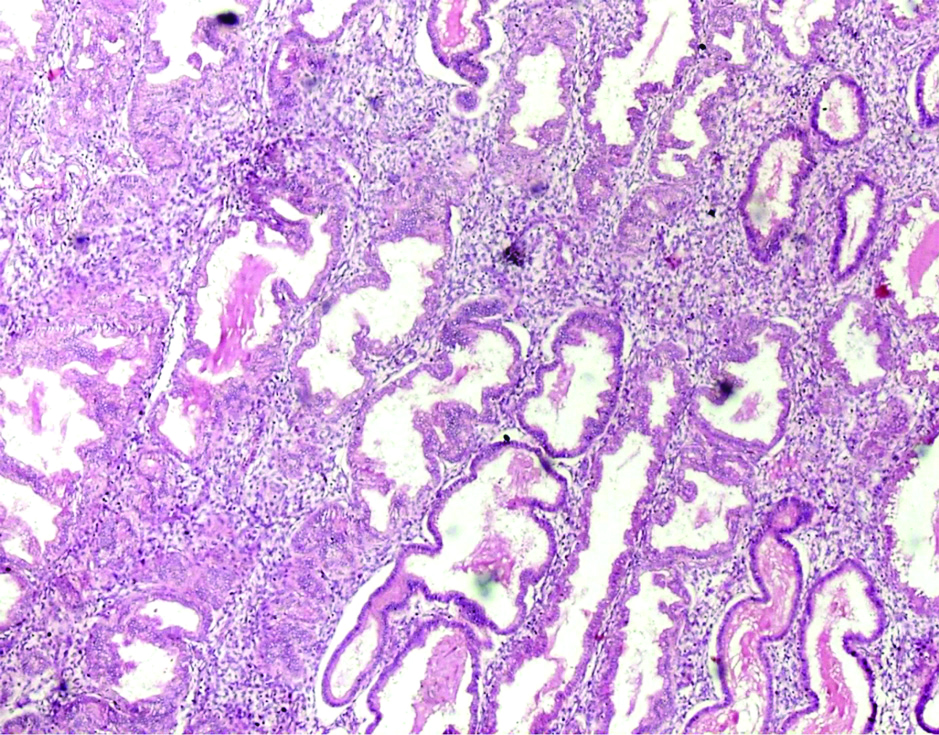
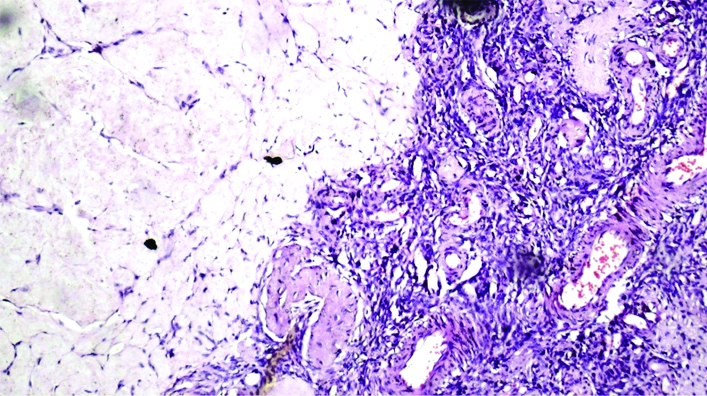
Smooth muscle cells arranged in bundles and fascicles with whorled pattern H&E Stain (100X).
Haemorrhage with focal glandular and stromal breakdown H&E Stain (100x).
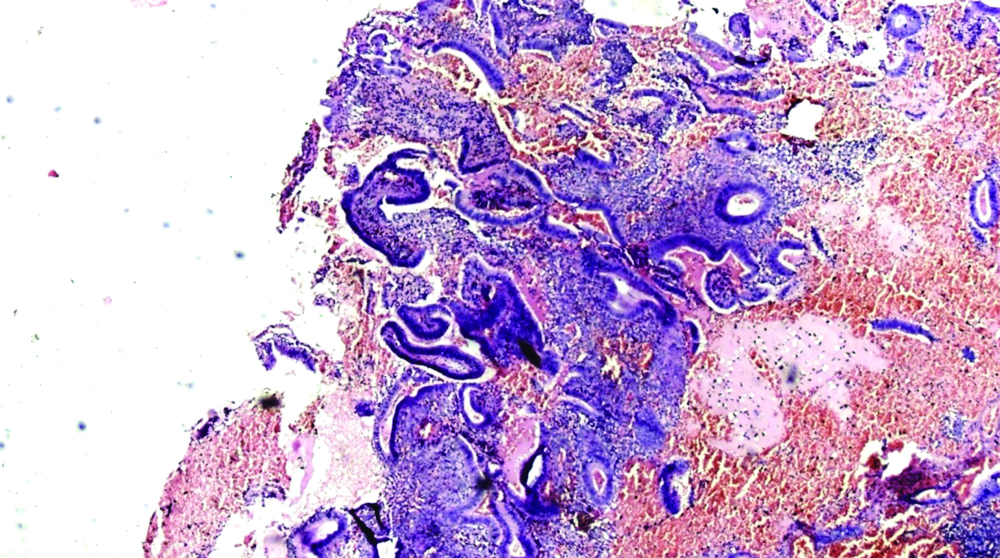
Endometrial glands showing back to back arrangement without atypia, H&E Stain (100X).
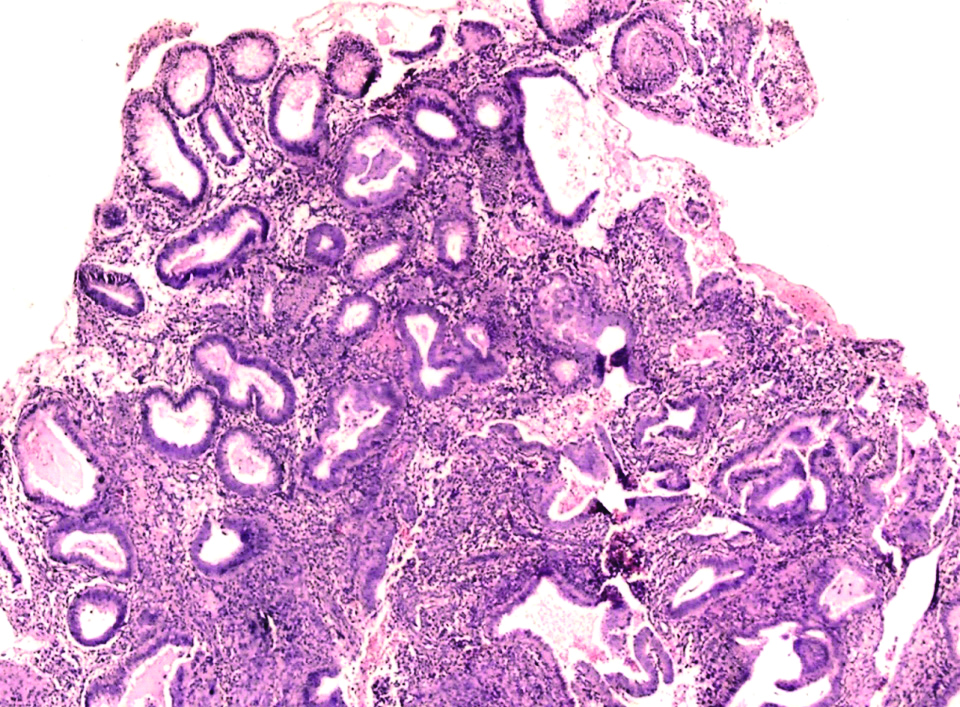
Proliferative endometrium, H&E Stain (100X).
Secretory endometrium, H&E Stain (100X).
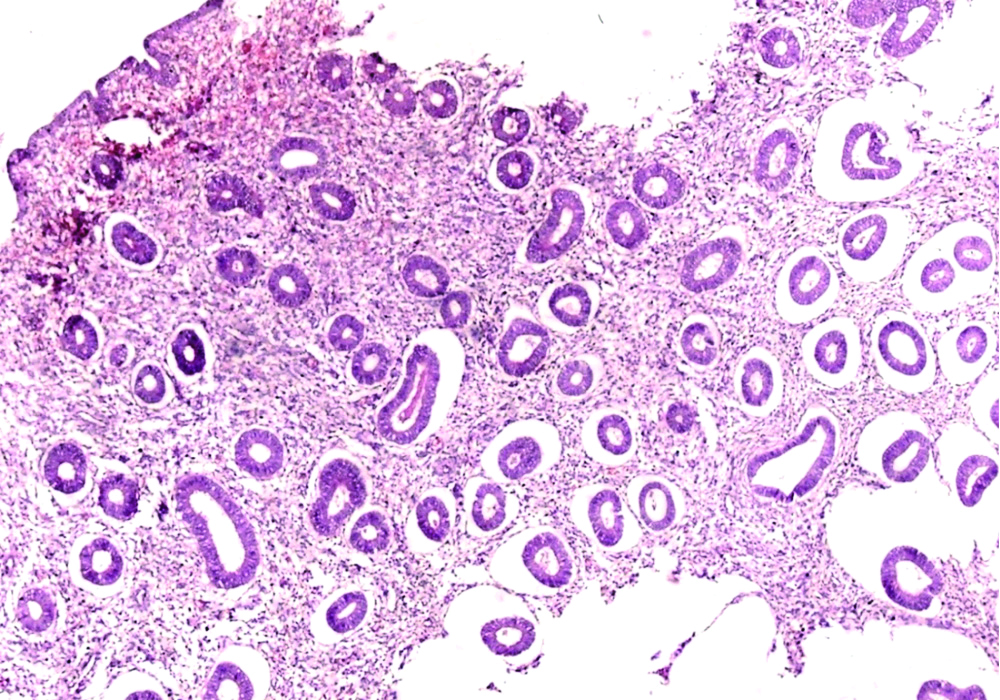
Polypoidal endocervicitis, H&E Stain (100X).
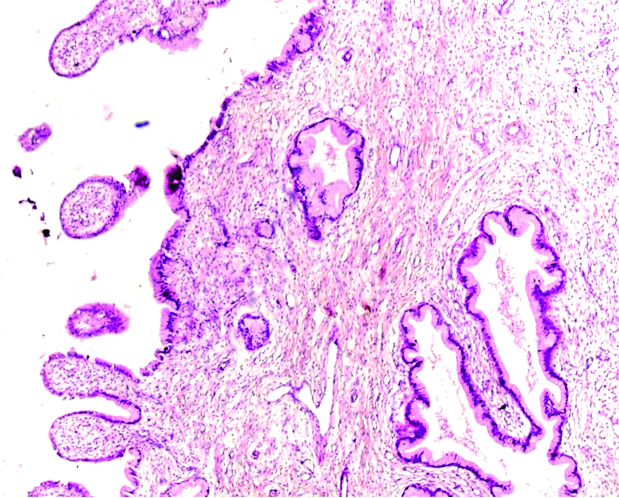
Normal fallopian tube, H&E Stain (100X).
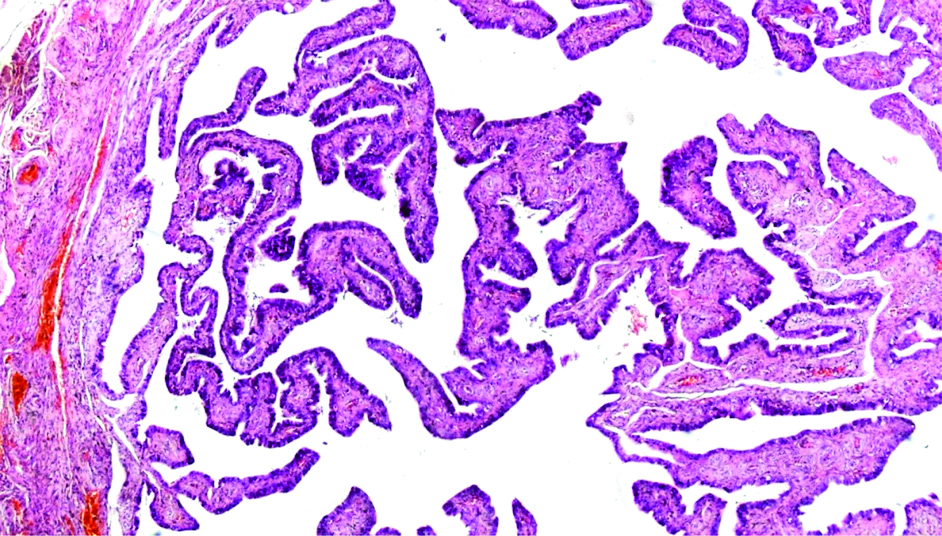
Fallopian tube lined by flattened plicae hydrosalphinx, H&E Stain (100X).
Normal ovary showing ovarian stroma and corpus albicans, H&E Stain (100X).
Analyses of fibroids: Fibroids were analysed in particular since this was the most common indication in the present study. Two parameters, whether fibroids were single or multiple, and the size of the fibroid were analysed. It was found that out of the total 152 fibroid uteri, 115 (75.65%) of them possessed a single fibroid. 37 (24.34%) of them possessed multiple fibroids [Table/Fig-14]. The analysis of the sizes of the fibroid revealed that most of the fibroids lied in the range of 4.1-6 cm in diameter (54, 35.5%) [Table/Fig-15].
| No. of fibroids | Number of cases | Percentage of cases |
|---|
| Multiple fibroids | 37 | 24.34% |
| Single fibroid | 115 | 75.65% |
| Total | 152 | 100% |
| Diameter of fibroid (in cm) | Frequency | Percentage (%) |
|---|
| <4 | 47 | 30.9 |
| 4.1-6 | 54 | 35.5 |
| 6.1-8 | 13 | 8.55 |
| >8 | 38 | 25 |
| Total | 152 | 100 |
Analysis of the ovary revealed that the ovary was unremarkable in 60 (34.8%) of the cases, followed by corpus albicans 37 (21.5%). All the lesions that were identified were benign. Analysis of the fallopian tubes revealed that in a majority of cases (142, 82.55%) it was within normal limits [Table/Fig-16].
Summary of the histopathological findings in fallopian tubes and ovaries.
| Histopathological findings of ovary | No. of cases | Histopathological findings of fallopian tube | No. of cases |
|---|
| Unremarkable | 60 (34.8%) | Within normal limits | 142 (82.55%) |
| Corpus albicans | 37 (21.5%) | Congestion | 4 (2.32%) |
| Follicular cyst | 22 (12.7%) | Simple serous cyst | 3 (0.17%) |
| Simple serous cyst | 22 (12.7%) | Follicular cyst | 3 (0.17%) |
| Corpus haemorrhagicum | 15 (8.7%) | Paratubal cyst | 2 (0.11%) |
| Corpus luteum | 6 (3.48%) | Mucinous cystadenoma | 1 (0.05%) |
| Luteal cyst | 4 (2.3%) | Cortical cyst | 1 (0.05%) |
| Congestion | 4 (2.3%) | Endometriosis | 1 (0.05%) |
| Serious cystadenoma | 1 (0.58%) | Hydrosalphinx | 11 (6.39%) |
| Fimbrial cyst | 1 (0.58%) | Salphingitis | 4 (2.32%) |
| 172 | | 172 |
Study in the Age Group 21-40 Years
A detailed analysis of the age group 21-40 years was done. As they are in the reproductive age, they experience the full-blown consequences of a hysterectomy, both reproductively and in other aspects. The most commonly performed surgery was still panhysterectomy (59, 88.05%) [Table/Fig-17].
Distribution of types of hysterectomies in 21-40 years age group.
| Type of hysterectomy | No. of cases | Percentage (%) |
|---|
| PAH | 59 | 88.05 |
| TAH | 4 | 5.97 |
| VH | 3 | 4.47 |
| TAH w ULSO | 1 | 1.49 |
| Total | 67 | 100 |
The indications and spectrum of histopathological findings was studied and results were tabulated. Out of the 67 cases, 53 cases in the age group of 21-40 years showed histopathological findings of fibroids, irrespective of the reason operated. It was found that the most common indication was fibroids in this age group (53, 79.10%). The size of the fibroid that most commonly occurred was in the range of 4.1-6 cm (20, 37.73%) [Table/Fig-18,19].
Size of fibroid in age group 21-40 years.
| Size of fibroids | No. of cases |
|---|
| <4 cm | 17 |
| 4.1-6 cm | 20 |
| 6.1-8 cm | 9 |
| >8.1 cm | 7 |
| Total | 53 |
Comparison of preoperative indications and histopathological findings in women in the age group of 21-40 years.
| Indications for surgery | No. of cases | Histopathology findings |
|---|
| Fibroids | 53 | Fibroids | 46 |
| Adenomyosis | 3 |
| Ademyosis with fibroid | 2 |
| Endometrial polyp | 1 |
| Adenocarcinoma | 1 |
| Pelvic inflammatory disease | 4 | PID+ Adenomyosis | 2 |
| PID+ Fibroid | 2 |
| UVP | 6 | 4 Cases had unremarkable histology2 cases showed fibroids in addition to UV Prolapse |
| DUB/AUB | 4 | 3- Unremarkable histology1-Fibroid |
UVP: Uterovaginal prolapse; DUB: Dysfunctional uterine bleeding; AUB: Abnormal uterine bleeding
Discussion
Hysterectomy was the most common operative procedure done after caesarean section in women. Many of these surgeries are done in reproductive age women for nonmalignant indications. Many alternate therapeutic options like levonorgestrel-releasing intrauterine system, endometrial ablation or fibroid embolisation can be tried in many cases before the hysterectomy is considered [11]. In one study, done by Kriplani A et al., Ormeloxifene was an effective and a safe therapeutic option for the medical management of menorrhagia [12].
Hysterectomy is a major surgery which has its own physical, economical, emotional, sexual and medical significance in women [1,2]. Various previous studies were in concordance with the findings found in this study [Table/Fig-20] [3,4,5,6,7,13-17].
Studies with similar findings.
| Author name | Year of publishing | Number of cases | Important findings agreeing with present study |
|---|
| Sivapragasam V et al., [14] | 2018 | 198 | The route of hysterectomy was most commonly abdominal (83.07%) followed by vaginal route (18.4%)Proliferative endometrium (41%) was the most common endometrial finding.Leiomyoma (51.7%) was the most common myometrial finding.Non-specific chronic cervicitis was the most common cervical finding.The ovaries were unremarkable in 62% and the fallopian tubes were unremarkable in 91% of specimens. |
| Chavhan S et al., [16] | 2018 | 50 | Leiomyoma (66%) was the most common myometrial finding.Non-specific cervicitis (78%) was the most common cervical finding. |
| Imam ZS et al., [17] | 2018 | 220 | The route of hysterectomy was most commonly abdominal (73.18%)75% of the endometrial specimens had normal histology.50.45% myometrial specimens were unremarkable, followed by leiomyoma (29.1%).Chronic cervicitis (70.9%) was the most common cervical finding.The ovaries were unremarkable in 45.9% specimens and the fallopian tubes were unremarkable in 36.36% specimens. |
| Verma D et al., [1] | 2016 | 152 | The route of hysterectomy was most commonly abdominal (63.8%) and followed by vaginal (37.5%).Proliferative endometrium was most found.Chronic cervicitis w/ w/o sq. metaplasia was most found. |
| Medhi P et al., [13] | 2016 | 150 | Leiomyoma (26%) followed by Adenomyosis (26%) were the most common myometrial findings.Chronic cervicitis was the most common cervical finding. |
| Gangadharan V et al., [15] | 2016 | 318 | The route of hysterectomy was most commonly abdominal (72.9%), followed by vaginal route (24.3%)Fibroid (39.3%) was the most common indication.Leiomyoma (42.13%) was the most common myometrial finding. |
| Tiwana KK et al., [4] | 2014 | 373 | The route of hysterectomy was most commonly abdominal (95.17%) followed by vaginal (4.83%).Leiomyoma was the most common indication.Leiomyoma followed by adenomyosis were the most common myometrial findings. |
| Pandey D et al., [5] | 2014 | 527 | The route of hysterectomy was most commonly abdominal (74.8%) followed by vaginal route (17.83)Fibroid uterus (39.84%), followed by UV prolapse (16.31%) were the most common indications |
| Bansal N et al., [11] | 2013 | 342 | The route of hysterectomy was most commonly abdominal (41.5%) followed by vaginal route (11.11%)Fibroid (27.8%) followed by DUB (22.80%) were the most common indications. |
| Awoleke JO et al., [6] | 2012 | 103 | The route of hysterectomy was most commonly abdominal (87.37%) followed by vaginal (10.6%).Fibroid uterus (84.46%) followed by malignancies (6.8%) were the most common indications. |
| Siwatch S et al., [10] | 2012 | 1270 | Fibroid (39.3%) followed UV Prolapse (22.6%) were the most common indications. |
| Bashir R et al., [7] | 2005 | 316 | The route of hysterectomy was most commonly abdominal (87.97%) followed by vaginal route (12.02%). |
| Roovers JP et al., [3] | 2003 | 352 | The route of hysterectomy was most commonly abdominal (59.94%) followed by vaginal (25.28%) |
| Present study | | 238 | The route of hysterectomy was abdominal (83.19%)Fibroid was the most common indication (638%) followed by UV prolapse (20.1%)Proliferative endometrium was most commonly found (20.1%)Leiomyoma was the most common myometrial finding (44.11%)Chronic cervicitis was the most common cervical finding (55.88%)25.2% and 59.6% of the ovaries and fallopian tubes respectively were within normal limits. |
In a study by Prusty RK et al., the average prevalence rate of hysterectomy was estimated to be 17/1000 among even married women in the ages of 15-49 years [8]. Out of the very few audits done to compare preoperative diagnosis with histopathological examination of specimens, a study by Tiwana KK et al., pointed out that 7-8% of rural women and 5% of urban women had undergone hysterectomy at an age of 37 years [4].
An audit was conducted on hysterectomies done in district hospital Madikeri, so that common public can be educated with the choice of hysterectomy and helps the medical fraternity in better decision making and assessment of symptoms. In this study in addition to the audit we gave importance to women in reproductive age groups and studied the pattern of indications and histopathological findings in them, as they are the women who face the brunt of unjustified hysterectomies mostly.
Age distribution: The youngest patient was 26 years while the oldest was 79-year-old. The mean age for hysterectomy was 46.46 years of age.
Indication: Most common indication for hysterectomy in our study was leiomyoma uterus, while few other studies showed different results for most common indication for hysterectomy, Verma D et al., utero-vaginal prolapse, Nausheen F et al., dysfunctional bleeding, Sivapragasam V et al., AUB [1,2,14]. This variation in the most common indication for hysterectomy in other studies and can be because of variation in the age group of predominant population in the study [1].
Adenomyosis was most common incidental finding which was frequently missed preoperatively. This is in concordance with a few other studies [4,13].
This was followed by fibroids of size between 4.1-6 cm (54, 35.5%), fibroids of less than 4 cm in diameter (47, 30.9%). 38 fibroids (25%) were >8 cm in diameter. Least number of fibroids was in the 6.1-8 cm range (13, 8.5%) [Table/Fig-15].
It was observed that these 47 (30.9%) cases which had a fibroid of dimension less than 4 cm in diameter and at least few cases with fibroid between the size of 4.1-6 cm could have been managed non-surgically first, before proceeding with hysterectomies. Adenomyosis cases can initially be treated with hormonal therapy, endometrial ablation and the many other nonsurgical options before deciding to perform surgery.
It is alarming that majority of these ovaries and fallopian tubes showed normal benign conditions histopathologically. Except for one case of adenocarcinoma, where panhysterectomy was justified. All these cases were of women in the reproductive age group where retaining the uterus and adnexa is important. An even more intriguing fact was that except for uterovaginal prolapse, many of these women were also subjected to panhysterectomy with bilateral removal of adnexa. Unnecessary removal of ovaries in these patients lead to deficiency of oestrogen, hastens the onset of menopause and patient’s psychosexual health is affected, apart from the vast array of health issues [8].
In such young population in reproductive age group effort should be made to retain adnexal structures when adnexa are normal and indication is benign. 16 cases had fibroid size more than 6.1 cm and histopathology confirmed the indication. 37 patients had fibroids of size less than six cm and 17 cases were with fibroids less than four cm in diameter in greatest dimensions. In these 37 cases, nonsurgical approach could have been attempted first. Therefore, choosing panhysterectomy over other options needs to be debated on as the aftermath is tremendous. Reporting of all hysterectomies should be made mandatory so that the audit results can be used for improvement in the quality of health services.
Controversies: Is it All the Fault of Health Care Providers?
One report in Maharashtra started with a somewhat troublesome question- “why do many women in Maharashtra’s Beed district have no wombs?” - investigated in a report published on April 11 2019 by India’s Business Line newspaper. Contractors of the sugarcane industry never hired women with wombs, forcing thousands of women to undergo hysterectomies. A PIL was filed and the Government of India decided in 2013 to get a national estimate of hysterectomy in women of reproductive age group through the fourth round of the “National Family Health Survey”. The latest National Family Health Survey, from 2015-16, has state-wise data on hysterectomy. But, unfortunately, many instances of coercive hysterectomies linked to livelihoods are still being reported [18]. In India, the research and debate on hysterectomies for benign reproductive health ailments has tended to focus invariably more on health provider, as said in a study by Desai S, which dealt with complex factors operating in the decision of hysterectomies [19].
Studies have showed that hysterectomies have both pros and cons with respect to women’s health. One such study done by Prusty RK et al., stated that “on the one hand, by relieving suffering from gynaecological ailments such as abnormal bleeding and pelvic pain, hysterectomy is found to lead to decreased anxiety and depression among women and thereby improvement in their quality of life, particularly 6 to 12 months after the surgery. Apart from this, research also shows several adverse effects of hysterectomy such as urinary incontinence, sexual dysfunction, late medical problems such as backache, weakness and early onset menopause [8].
Oophorectomy in reproductive age women can have various complications associated with hormonal imbalance like increased risk of osteoporosis, coronary heart disease and thus poses excess mortality risk [8]. There is need for education among poor rural women about dangers of hysterectomies and alternative management strategies [2].
Taboo against menstruation, poverty, illiteracy, socioeconomic factors, poorly developed medical infrastructure and some degree of possible malpractice by health care providers have together added to the complexity of performing a hysterectomy [19].
India’s health system currently caters to a limited range of health services for women, largely related to pregnancy, delivery, family planning, and postpartum care. There is thus a need for improvements in management of chronic gynaecological complaints in advanced way and stop using hysterectomies as a one stand option for chronic gynaecological complaints.
Limitation(s)
Limitation of this study was that, since the study was cross-sectional in nature, follow-up of women and the consequences could not be studied and further study needs to be done focussing on follow-up.
Conclusion(s)
The indications for hysterectomies were frequently for benign conditions, yet the rate of panhysterectomy was higher. Menace of unnecessary hysterectomy is a complex problem which is a result of multiple deficiencies in healthcare, socioeconomic, individual loopholes. Though, it is an effective treatment option for various gynaecological problems it should be used judiciously after careful evaluation of the necessity. Regular audits to confirm the indications by histopathological support are a necessity.
Although hysterectomy is a good procedure in justified cases, in many benign cases, use of advanced alternate management can save the woman from the trouble of going under the knife and the many postoperative complications associated with the procedure.
PAH: Pan-abdominal hysterectomy; VH: Vaginal Hysterectomy; TAH: Total abdominal hysterectomy; TAH w ULSO: Total abdominal hysterectomy with unilateral salphingo oophorectomy