Lumbosacral Spondylodiscitis- An Atypical Localisation of Salmonella Typhi Infection: A Case Report
Sruthi Vinayan1, Vimal Karnaker2, V Sreelatha3, Sanjana Nair4
1 Postgraduate, Department of Microbiology, KS Hegde Medical Academy (KSHEMA), Nitte (Deemed to be University), Mangalore, Karnataka, India.
2 Professor and Head, Department of Microbiology, KS Hegde Medical Academy (KSHEMA), Nitte (Deemed to be University), Mangalore, Karnataka, India.
3 Additional Professor, Department of Oral Pathology, AB Shetty Memorial Institute of Dental Sciences (ABSMIDS), Nitte (Deemed to be University), Mangalore, Karnataka, India.
4 MBBS Student, Srinivas Institute of Medical Sciences and Research Centre, Mangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vimal Karnaker, Professor and Head, Department of Microbiology, K S Hegde Medical Academy, Nithyanandanagar P.O, Deralakatte, Mangalore-575018, Karnataka, India.
E-mail: vimalkarnaker@yahoo.co.in
Salmonella belongs to the family Enterobacteriaceae. The various members of the genus cause diseases that are important public health problems. Apart from causing typhoid, Salmonella can cause an array of diseases ranging from osteomyelitis to meningitis, though rare. Herein, authors report one such uncommon scenario, in an otherwise healthy 40-year-old female who presented with lower back pain. Magnetic Resonance Imaging (MRI) was suggestive of lumbosacral spondylodiscitis and she underwent a spine stabilisation surgery. The pathogen was confirmed to be Salmonella Typhi by microbiological workup. She responded well to treatment with ceftriaxone. This case report implies the significance of culture studies in the early management of the patient. It is imperative for the diagnosis, as the symptoms of the aforementioned disease are usually non-specific and imaging studies are indiscernible from spine tuberculosis.
Low back pain, Lumbosacral spine, Lumbar vertebrae
Case Report
A 40-year-old lady presented with a one-month history of lower back pain radiating to the right lower limb. The pain was insidious in onset and gradually progressive. One week prior to her admission her symptoms aggravated with sharp shooting pain radiating to lower limb which worsened on walking, sitting, and relieved on lying down. These symptoms were not preceded by trauma. She disclosed a past history of high grade, intermittent fever (102°C) one month back with no gastrointestinal symptoms, and was diagnosed with urinary tract infection elsewhere. Widal test done then was negative along with other febrile illness tests such as malaria parasite fluorescent test, dengue IgM and leptospira IgM ELISA. She had no history of co-morbidities such as diabetes mellitus, hypertension, and immunosuppression. No history of similar complaints was noted among the family members.
She was afebrile, general and systemic examination was unremarkable. Physical examination revealed tenderness over the lower lumbar spinous process. No local temperature rise or palpable mass, bony deformities, or neurological deficits were noted. Laboratory investigations revealed an elevated Erythrocyte Sedimentation Rate (ESR) of 80 mm/h and elevated C-reactive protein of 61.81 mg/L. No leucocytosis was present. MRI of the lumbosacral spine showed enhancing altered marrow signal involving L5 and S1 vertebrae with enhancing intervening disc, anterior epidural collection, and paravertebral collection which was suggestive of infective spondylodiscitis L5-S1 [Table/Fig-1].
Sagittal magnetic resonance image of the lumbar spine showing altered signal intensity of L5/S1 intervertebral disc level with end plate irregularities of inferior end plate of L5 and superior end plate of S1. There was associated soft tissue component/collection at this level extending inferiorly to S1/S2 level causing narrowing of neural foramen and compressing on the nerve roots at these levels. Displaying hypointense signal intensity on T2/STIR. Features consistent with infective aetiology-Spondylodiscitis

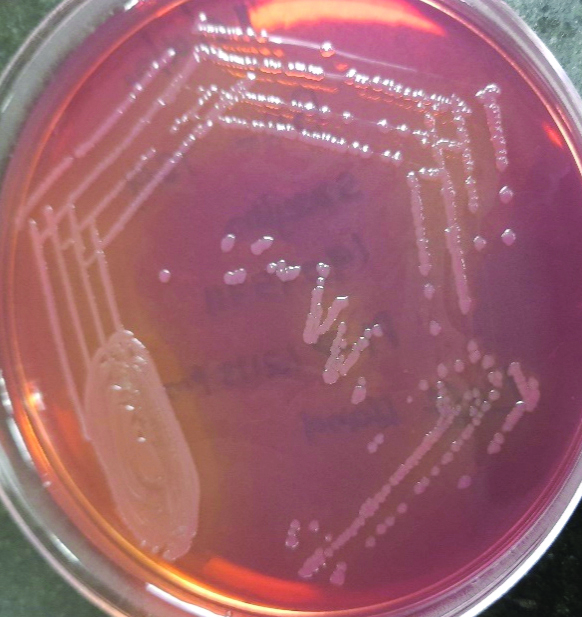
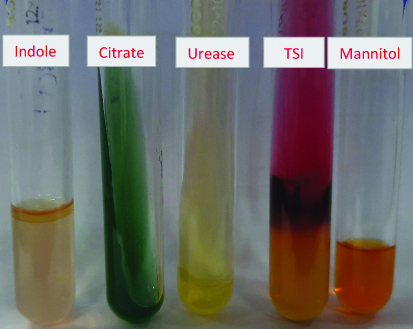
Surgery was done for the stabilisation of the spine. Microbiological examination was done on the tissue sample after processing and culturing it onto 5% Sheep Blood Agar (SBA) and MacConkey agar (MAC). After 24 hours of incubation, the colony morphology on SBA showed moist non-haemolytic colonies and on MAC, translucent non-lactose fermenting colonies appeared [Table/Fig-2]. The growth was identified as Salmonella Typhi by Vitek 2- compact system (BioMérieux) followed by antimicrobial susceptibility testing using the same. Biochemical reactions [Table/Fig-3] and slide agglutination test (agglutination with O9 and Hd antigen) corroborated the identification. The organism was sensitive to ceftriaxone, ampicillin, carbapenems, co-trimoxazole, ciprofloxacin. The tissue sample was negative for acid fast bacilli. The aforementioned bacteriological workup deduced a diagnosis of Salmonella lumbosacral spondylodiscitis L5-S1.
Translucent non-lactose fermenting colonies on MAC.
Biochemical reactions of the isolate showing Indole negative, Citrate not utilised, Urea is not hydrolysed, TSI K/A+H2S, Mannitol fermented with motility seen.
Antibiotic therapy with Inj.Ceftriaxone 2 gm intravenously twice daily was given for three weeks and full weight-bearing mobilisation was started. She subsequently became symptomatically better and was discharged with advice to follow-up. Follow-up in outpatient clinic at four weeks showed substantial reduction of back pain and retaining good function.
Discussion
Spondylodiscitis is an infectious inflammation of the vertebral body, intervertebral discs, and adjacent structures. The aetiology can be bacterial, fungal, and parasitic with the commonest pathogen being Staphylococcus aureus [1,2]. Strains of Salmonella spp. are categorised as typhoidal and non-typhoidal corresponding to the associated disease. Salmonella spp. can cause infection at unusual sites with diverse manifestations [3]. Of which, bone and joint infections contribute to less than 1% [4]. Spine infections are rare and mostly involves the lumbar and lower thoracic vertebrae [5]. Infective spondylodiscitis in itself is a relatively rare disease and is associated with significant morbidity. Lumbar region is the most common site of infection. Back pain is the most common presenting symptom which is seen in about 97% of patients, followed by fever [2]. Fever can also appear prior to the back pain and later wane [6]. Salmonella spondylodiscitis may occur without an active form of disease in the gastrointestinal tract and manifestations can appear later on [7]. ESR elevation is considered to be non-specific even though seen in most cases. Leukocytosis is often absent in infective spondylodiscitis hence, it does not provide any considerable diagnostic value [2]. Lack of specific symptoms, often results in delay of the diagnosis [1]. Studies in the past have suggested that imaging techniques such as radiograph, MRI, and histopathological examination alone could not reliably differentiate Salmonella and tuberculous infections [8]. The conclusive element to diagnose Salmonella spondylodiscitis is the culture identification of the organism, from a bone specimen obtained by needle or open biopsy, aspirate of an adjacent fluid collection, pus. Therefore, culture studies remain the imperative means to reach a definitive diagnosis and provide efficacious treatment [6,8]. Salmonella infection usually responds well to antibiotic therapy, hence, aetiological diagnosis and determination of the antibiotic susceptibility pattern are paramount. Surgical intervention to stabilise or decompress the spine is also essential for management of the patient [8].
Conclusion(s)
Suspected spondylodiscitis case approach begins with a thorough history to assess the course of illness, predisposing conditions, and physical examination. Neurologic examination is vital, to rule out neurological deficits. MRI is highly sensitive and specific imaging modality which is preferred for the diagnosis of infective spondylodiscitis. Microbiological workup is a sensitive measure, and, isolation of the aetiological agent is a necessity in ruling out tubercular aetiology and formulating the antimicrobial therapy.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? No
For any images presented appropriate consent has been obtained from the subjects. No
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 20, 2020
Manual Googling: Aug 25, 2020
iThenticate Software: Sep 29, 2020 (1%)
[1]. Homagk L, Marmelstein D, Homagk N, Hofmann GO, SponDT (Spondylodiscitis Diagnosis and Treatment): Spondylodiscitis scoring systemJournal of Orthopaedic Surgery and Research 2019 14(1):10010.1186/s13018-019-1134-930971277 [Google Scholar] [CrossRef] [PubMed]
[2]. Jose N, Ralph R, Mani T, Zachariah A, Infective Spondylodiscitis-An Indian perspectiveWorldwide Journals 2020 6(8):54-60.[cited 4 March 2020]. Available from: https://www.worldwidejournals.com/indian-journal-of-applied-research-(IJAR)/article/infective-spondylodiscitis-an-indian-perspective/OTgxNA==/?is=1 [Google Scholar]
[3]. Marzel A, Desai PT, Nissan I, Schorr YI, Suez J, Valinsky L, Integrative analysis of salmonellosis in Israel reveals association of Salmonella enterica Serovar 9,12:l,v:- with extraintestinal infections, dissemination of endemic S. enterica serovar Typhimurium DT104 biotypes, and severe underreporting of outbreaksJ Clin Microbiol 2014 52(6):2078-88.10.1128/JCM.00399-1424719441 [Google Scholar] [CrossRef] [PubMed]
[4]. Farrar H, Abbey A, Patel V, Nair R, Osteomyelitis, discitis, epidural and psoas abscess secondary to Salmonella enterica in a man with diabetes mellitus and newly diagnosed α-thalassaemia traitCase Reports 2015 2015:bcr201420700810.1136/bcr-2014-20700825608980 [Google Scholar] [CrossRef] [PubMed]
[5]. Huang DB, DuPont HL, Problem pathogens: Extra-intestinal complications of Salmonella enterica serotype Typhi infectionThe Lancet Infectious Diseases 2005 5(6):341-48.10.1016/S1473-3099(05)70138-9 [Google Scholar] [CrossRef]
[6]. Banerjee B, Madiyal M, Madhava PK, Agarwal M, Mukhopadhyay C, Typhoid spondylodiscitis mimicking tuberculosis in a teenage girlJournal of Infection and Public Health 2018 11(1):136-37.10.1016/j.jiph.2017.04.00428602673 [Google Scholar] [CrossRef] [PubMed]
[7]. Shrestha P, Mohan S, Roy S, Bug on the back: Vertebral osteomyelitis secondary to fluoroquinolone resistant Salmonella typhi in an immunocompetent patientCase Reports 2015 2015:bcr201521250310.1136/bcr-2015-21250326621865 [Google Scholar] [CrossRef] [PubMed]
[8]. Effendi FM, Ibrahim MI, Miswan MFM, Salmonella spondylodiscitis of the thoracic vertebrae mimicking spine tuberculosisCase Reports 2016 2016:bcr201621590910.1136/bcr-2016-21590927381996 [Google Scholar] [CrossRef] [PubMed]