The long time needed to finish orthodontic treatment is considered one of the reasons that prevent patients from seeking it; therefore, reducing the time of orthodontic treatment is one of the factors of successful orthodontic treatment thus overcoming many problems such as increased caries rate, gingival inflammation and root resorption [1].
Many flapless alternative techniques have been suggested to avoid the invasiveness of the corticotomy procedures thus producing less pain and discomfort with the possibility of initiating the Regional Acceleratory Phenomenon (RAP) [7]. Some of these alternatives are reinforced scalpels and mallets (corticision) [8], Micro-Osteoperforation (MOP) [9], piezopuncture [10] and piezocision [11-13].
As an alternative flapless technique, corticision is considered a promising tooth acceleration technique because of its various advantages on periodontal, health, simplicity, availability, and lower cost. This technique has been studied in animals only. Kim SJ et al., studied corticision effect on cats [14]. They noticed increased remodeling and dental movement by 3.5 times when corticision was applied and monitored for 28 days. In Gu Q et al., study on experimental animals, three levels were discussed: histological, cellular and molecular [15]. Increased bone demineralization, osteoclast cells and orthodontic dental movement were observed in the corticision group.
According to a recent review by Charavet C et al., there is no published randomised controlled clinical trial evaluating the original corticision method [7]. Therefore, the present randomised controlled clinical trial was carried out to compare the conventional orthodontic treatment to corticision-based orthodontic treatment in adult patients. The primary objective was to determine the overall leveling and alignment time in each group. The secondary objective was to compare periodontal parameters between the two groups.
Materials and Methods
Study Design
This study was a two-arm, parallel-group, Randomised Controlled Clinical Trial evaluating the effect of corticision in accelerating tooth movement in dental crowding cases. The CONSORT statement was used as a guide for this study [16]. The study was conducted in the Department of Orthodontics at the University of Damascus Dental School between March 2017 to September 2018. This study received approval from the Local Research Ethics Committee of the University of Damascus Dental School, Syria (UDDS-519-20160018/SRC-3070), and was registered at ClinicalTrails.gov (Identifier: NCT03310086) before the onset of patients’ recruitment. Funding was covered by the University of Damascus Dental School Postgraduate Research Budget (Ref no: 72043105672DEN).
Sample Size Estimation
The sample size was calculated using the G*power 3.1.3 software with an alpha level of 0.05, a power of 95%. The estimated sample of 60 patients was required for both groups (30 patients per each group).
Patients’ Recruitment
The sample was recruited from the Department of Orthodontics at the University of Damascus Dental School. A clinical examination was done on 145 patients by one of the author. One hundred and forty-five mild and moderate dental crowding patients were obtained, and their possible treatment plans were reviewed. The number of patients who met the inclusion criteria was 87, and the final number of patients who agreed to participate in this trial after reading the information sheet of the trial was 74. According to the prior sample size calculation, which indicated the need for 60 patients, a simple random sampling was applied to select 60 patients from this sampling frame.
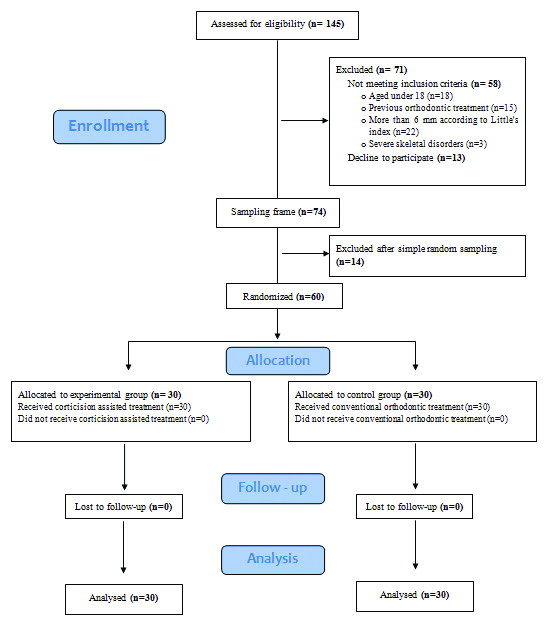
The purpose and methods of the study were explained to the patients and parents; informed consent was obtained from each patient. The patients’ flow diagram at the different stages is illustrated in [Table/Fig-1].
CONSORT flow diagram of patients’ recruitment, follow-up and entry into data analysis.
Patients were considered eligible for the study if they met the following inclusion criteria: 1. aged between 18 and 25 years; 2. mild to moderate crowding (less than 6 mm according to Little’s index); 3. no spaces on the dental arch; 4. no periodontal diseases; 5. permanent occlusion with existence of all permanent teeth in the mandibular arch (except for third molars).
The following exclusion criteria were applied: 1) the presence of a systemic health condition affecting dental movement; 2). bad oral hygiene or the presence of periodontal disease (PI more than 1), previous orthodontic treatment; 3) severe skeletal disorders; 4) craniofacial disorders, and 5) the inability to bond brackets on the anterior mandibular teeth.
Randomisation and Allocation Concealment
Simple randomisation was conducted by using computer-generated random numbers with an allocation ratio of 1:1. The allocation sequence was concealed using sequentially numbered, opaque, sealed envelopes, which were opened after patients’ completion of all baseline assessments and the intention to commence active treatment. Corticision group received corticision orthodontic treatment, whereas the control group received conventional orthodontic treatment. Patients were treated by the principal author (MRS) who was completely blinded. Periodontal indices were evaluated in both the groups before (three days before brackets bonding) and after the orthodontic treatment (seven days after brackets’ debonding) by the same principal author (MRS). Corticision and initial wire insertion were accomplished by one of the co-authors (MYH) who was also blinded to the study. Blinding of participants was not applicable. Additionally, blinding was applied for the outcomes’ assessor, who was one of the co-authors (ASB).
Pre-treatment Analyses
At baseline, all patients underwent a comprehensive clinical, functional examination, including alginate impression taking (Hydrogum, Zhermack Co, Polesine (RO), Italy). The tooth-size arch-length analysis was performed on study models (Lundström analysis [17]) using digital calipers (Insize, Insize Co., Suzhou New District, China), and the Little’s index or irregularity was calculated [18]. Periapical digital imaging for lower crowded anterior teeth (RVG 6100 sensor, Carestream, Kodak, USA) was performed.
Orthodontic Procedures
In both the groups, fixed orthodontic appliances with an MBT prescription and 0.022-inch slot height (Pinnacle bracket system®, Ortho technology”, Florida, USA) were bonded. The archwire sequence used was 0.014-inch Nitinol (NiTi) (American Orthodontics, Sheboygan, Wisc) followed by 0.016×0.016-inch NiTi and 0.017×0.025-inch NiTi, and finally 0.019×0.025-inch stainless steel (SS) (American Orthodontics, Sheboygan, Wisc) [19]. Patients were recalled every 14 days to move from one archwire to the following one depending on the amount of leveling and alignment achieved.
Changing from one wire to the next is done when the applied wire is neutral or near neutral, along with the ability to insert the next wire-totally within the brackets of all lower teeth [19]. The alignment and leveling process is considered to be done when the little index is less than 1 mm, with the ability to insert the last wire neutrally within all brackets [19].
Corticision Group
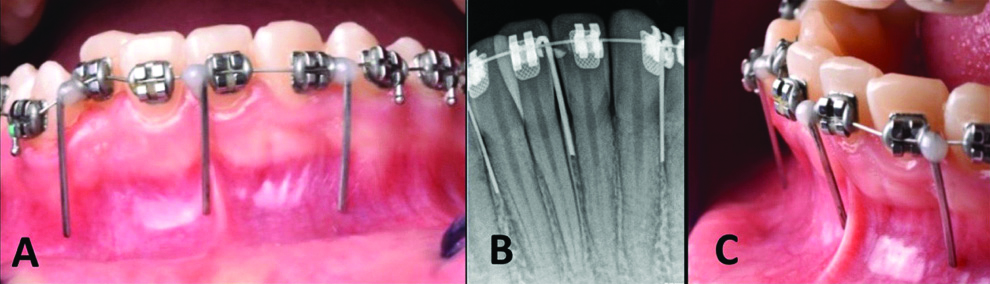
After bonding brackets, incision lines were located precisely depending on three radiological guides [19], 0.016×0.022 SS straight metal wires were used (American Orthodontics, Sheboygan, WI USA). The wires were designed- with a length ranging from 10 to 15 mm according to the location of the mucogingival junction, so they were placed in the approximate corticision areas (between mandibular canine and the lateral incisor roots on each side, and between the roots of the central incisors) and linked with a 0.014 stainless steel wire passing through the brackets neutrally using flowable composite (Crystal-Essence, Confi-Dental, Louisville, CO, USA). This was performed to determine the longitudinal axes of the lower anterior teeth and thus determine the axes of the cut with the surgical blade, which enabled the surgery to be performed with minimal trauma and without flap elevation [Table/Fig-2]. A periapical radiograph was obtained. Patients rinsed with Chlorhexidine Gluconate 0.12% (Oral-B, Gillette Group, Procter & Gamble Company, USA) for one minute before surgery, then received local infiltration anaesthesia (lidocaine hydrochloride 2% with epinephrine 1:80 000). Following that, the incision was made using a surgical blade No.15 by inserting it between the mandibular canine and the lateral incisor roots on each side, and between the roots of the central incisors, 4 mm apart from the gingival papilla. When reaching the alveolar bone, the surgical mallet (Atlas Surgical Company, Delhi, India) was used over surgical scalpels aiming to produce a fissure that was deeper than the cortical bone by 3-4 mm and 4-5 mm long [Table/Fig-3]. Corticision is applied only once at the three given areas for each patient at the beginning of the treatment and before applying the first wire. The orthodontic force (0.14 NiTi archwire) was applied immediately (in the same appointment) after the incisions were made. Patients were observed every 14 days to move from one archwire to the following one, depending on the amount of leveling and alignment achieved.
Three metallic guides were used before taking digital radiographs: Clinical appearance of the metallic guides from a frontal view (a); radiological appearance of these pins (b); lateral view of the metallic guides (c).
Three vertically oriented corticisions were performed using the surgical blade no 15: entry angle into the mucosa and alveolar bone (a); The surgical mallet was used over surgical scalpels (b); the clinical appearance following the minimally invasive intervention (c). Each corticision had a 4-5 mm length and 3-4 mm depth.

Wounds were left to heal by the second intention without suturing. The patient was informed to follow a soft diet and avoid mouth rinsing for 24 hours after the surgery; the patient was asked to start rinsing the day after the surgery with 0.12% Chlorhexidine solution two times a day for a week. No medication was prescribed after the surgery.
Primary and Secondary Outcome Measures Leveling and Alignment Time
The overall leveling and alignment time (days) required to complete anterior alignment of the mandibular dental arch was measured.
Periodontal Assessment
The six lower anterior teeth were examined for each patient, i.e., 360 lower anterior teeth were examined with 180 teeth in the corticision group and 180 teeth in the control group.
The following clinical parameters were measured at baseline (three days before brackets bonding) and after the orthodontic treatments: PI, GI, PD, the width of attached gingiva.
The PI assesses [20] only the thickness of the plaque at the gingival area of the tooth. It examines the following surfaces of the teeth: distobuccal, buccal, mesiobuccal, and lingual surfaces. A mouth mirror and a dental explorer are used after air drying the teeth to assess plaque, and the PI value for each area is obtained by calculating the mean of the values of the six teeth for each patient [20].
The GI [21] assesses the severity of gingivitis and its location in four possible areas: the distobuccal papilla, the buccal margin, the mesiobuccal papilla, and the entire lingual gingival margin.
The GI value for each area is obtained by calculating the mean of the values of the six teeth for each patient [21]. The PD is the distance to which an instrument (probe) penetrates into the pocket. In the present study, the periodontal pocket depth was measured with a millimeter-calibrated periodontal probe (Williams probe) on the following surfaces of the teeth: distobuccal, buccal, mesiobuccal and lingual surfaces. The probe was inserted with firm, gentle pressure to the bottom of the pocket. The shank should be aligned with the long axis of the tooth surface to be probed. The criterion for the (PD) was as follows: normal=(<3 mm), abnormal=(>3 mm) [21,22]. When a PD value is equal or less than 3 mm, the gingival sulcus is normal, whereas a PD value greater than 3 mm indicates a gingival pocket. The width of the attached gingiva was calculated as a difference of the PD from the width of the keratinised tissue, and the measurement was done from the buccal region only. The criterion for the width of the attached gingiva was as follows: normal=(≥3 mm), abnormal=(<3 mm) [23].
STATISTICAL ANALYSIS
Statistical analysis of the data was performed using Statistical Package for Social Sciences (SPSS) software, version 22.0, IBM Corporation, Australia. The Kolmogorov-Smirnov test was used to test the normality of data distribution. If the data was normally distributed, parametric test was applied and if the data distribution was not normal, non parametric test was applied. Mean comparisons were performed by two-sample t-tests. Mann–Whitney U tests were used for ordinal variables (PI and GI). The results were considered significant if p≤0.05.
Error of the Method and Assessment of Reliability:
To assess measurement reliability, 20 dental casts (were randomly chosen, and Little’s index was remeasured one month after the first measurement by the first author. Reliability was evaluated using Intraclass Correlation (ICC), which gave strong intra-examiner reliability (ICC=0.991). Periodontal indices were re-evaluated for twenty patients (randomly chosen) half an hour before brackets bonding by the first author. Reliability was evaluated using the ICC, which revealed a strong intra-examiner reliability (ICC=0.999).
Results
Patient Characteristics
Basic sample characteristics are presented in [Table/Fig-4,5]. Sixty patients {19 males (10 in control group/9 in corticision group) and 41 females (20 in control group/21 in corticision group)} were recruited in this study. Space analysis of the study models revealed a mean crowding of 4.58±0.069 mm in the mandible in control group. Corticision and control groups were apparently homogeneous in terms of age, crowding level, and all periodontal parameters [Table/Fig-4,6], since no significant differences were observed between the two groups. All patients attended their appointments, and there were no dropouts during the study.
Baseline sample characteristic.
| Variables | Control group (N=30) | Corticision group (N=30) | p-value |
|---|
| Mean | SD | Mean | SD |
|---|
| Age (years) | 21.40 | 1.63 | 21.13 | 1.30 | 0.812* |
| Space analyses (mm) | 4.58 | 0.069 | 4.22 | 0.079 | 0.262* |
N: Number of patients; SD: Standard deviation; *Employing two-sample t-test
Descriptive statistics of the periodontal parameters recorded before and after treatment in the corticision and control groups (Mean±SD).
| Variables | Before treatment | After treatment |
|---|
| Control group (N=30) | Corticision group (N=30) | Control group (N=30) | Corticision group (N=30) |
|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD |
|---|
| Plaque index | Buccal | 0.25 | 0.26 | 0.30 | 0.26 | 0.86 | 0.35 | 1.08 | 0.42 |
| Lingual | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Mesial | 0.45 | 0.29 | 0.63 | 0.38 | 1.36 | 0.52 | 1.63 | 0.39 |
| Distal | 0.60 | 0.39 | 0.45 | 0.32 | 1.30 | 0.50 | 1.13 | 0.55 |
| Probing depth | Buccal | 1.38 | 0.26 | 1.45 | 0.31 | 2.03 | 0.35 | 2.08 | 0.33 |
| Lingual | 1.36 | 0.27 | 1.26 | 0.23 | 1.45 | 0.31 | 1.40 | 0.22 |
| Mesial | 2.31 | 0.27 | 2.25 | 0.16 | 2.45 | 0.31 | 2.31 | 0.17 |
| Distal | 2.23 | 0.23 | 2.28 | 0.26 | 2.58 | 0.27 | 2.66 | 0.33 |
| Gingival Inde | Buccal | 0.40 | 0.35 | 0.56 | 0.40 | 0.56 | 0.42 | 0.80 | 0.41 |
| Lingual | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Mesial | 0.45 | 0.34 | 0.51 | 0.42 | 0.63 | 0.38 | 0.76 | 0.30 |
| Distal | 0.60 | 0.38 | 0.73 | 0.31 | 0.80 | 0.32 | 0.97 | 0.42 |
| WAG | Buccal | 4.03 | 0.57 | 4.23 | 0.56 | 3.85 | 0.46 | 3.90 | 0.55 |
N: Number of patients; WAG: Width of the attached gingiva; SD: Standard deviation. Both the probing depth and the WAG are mentioned in mm
Descriptive statistics of the periodontal parameters at the first assessment time in both the corticision and control groups as well as the p-values of significance tests.
| Variables | Mean difference | 95% CI for difference | p-value |
|---|
| Plaque index | Buccal | 0.05 | (-0.08, 0.18) | 0.467* |
| Lingual | 0 | 0 | 1.000* |
| Mesial | 0.18 | (0.00, 0.36) | 0.042* |
| Distal | -0.15 | (-0.33, 0.03) | 0.112* |
| Probing depth | Buccal | 0.06 | (-0.08, 0.21) | 0.372† |
| Lingual | 0.10 | (-0.23, 0.03) | 0.138† |
| Mesial | -0.06 | (-0.18, 0.04) | 0.251† |
| Distal | 0.05 | (-0.07, 0.17) | 0.439† |
| Gingival index | Buccal | 0.15 | (-0.04, 0.35) | 0.116* |
| Lingual | 0 | 0 | 1.000* |
| Mesial | 0.05 | (-0.14, 0.25) | 0.560* |
| Distal | 0.13 | (-0.04, 0.31) | 0.145* |
| WAG | Buccal | 0.20 | (-0.09, 0.49) | 0.173† |
*: Mann-Whitney test; †: Two-sample t-test; SD: Standard deviation; WAG: Width of the attached gingiva; Both the probing depth and the WAG are mentioned in mm.
Primary Outcome
There was a statistically significant difference in the leveling and alignment duration between the corticision and control groups. The mean leveling and alignment duration in the corticision group was 116.46±.15.97 days, compared to 159.69±13.76 days in the control group (p-value <0.001), i.e., a statistically significant reduction in the leveling and alignment duration of about 27% in the corticision group [Table/Fig-7].
Statistical analysis of leveling and alignment time (Mean±SD).
| Variable | Group | Number of patients | Mean | Standard deviation | Mean difference | t value | p-value* |
|---|
| Treatment duration | Corticision | 30 | 116.46 | 15.97 | -37.23 | -6.367 | <0.001 |
| Control | 30 | 159.69 | 13.76 | |
*: Employing Two-sample t-test.
Secondary Outcomes
The differences between the two groups regarding the observed changes in the periodontal indexes after treatment were statistically insignificant. The probing depth on the buccal side (p=0.887) and the width of the attached gingiva (p=0.075) [Table/Fig-8]. In each group, the observed clinical changes were {(1)} the increase in the PI on the buccal surface in the corticision and the control groups (PI=1.08±0.42 and 0.86±0.35, respectively) and {(2)} the increase in the PD on the buccal surface in the corticision and control groups (PD=2.08±0.33 mm and 2.03±0.35 mm, respectively). However, these changes did not reach statistical significance.
Descriptive statistics of the differences between the two groups regarding the observed changes as well as the p-values of significance tests.
| Variables | Mean difference | 95% CI for difference | p-value |
|---|
| Plaque index | Buccal | 0.16 | (-0.00, 0.33) | 0.054* |
| Lingual | 0 | 0 | 1.000* |
| Mesial | 0.08 | (-0.10, 0.27) | 0.373* |
| Distal | -0.01 | (-0.2, 0.20) | 0.878* |
| Probing depth | Buccal | -0.01 | (-0.25, 0.21) | 0.887† |
| Lingual | 0.05 | (-0.04, 0.14) | 0.287† |
| Mesial | -0.06 | (-0.15, 0.02) | 0.154† |
| Distal | 0.03 | (-0.09, 0.15) | 0.597† |
| Gingival index | Buccal | 0.08 | (-0.02, 0.18) | 0.117* |
| Lingual | 0 | 0 | 1.000* |
| Mesial | 0.07 | (-0.03, 0.18) | 0.180* |
| Distal | 0.04 | (-0.09, 0.17) | 0.534* |
| WAG | Buccal | 0.15- | (-0.32, 0.01) | 0.075† |
*: Mann-Whitney test; †: Two-sample t-test; SD: Standard deviation; WAG: Width of the attached gingiva; Both the probing depth and the WAG are mentioned in mm.
Discussion
This is the first RCT to assess the effect of corticision on accelerating leveling and alignment in the decrowding orthodontic treatments. Mild and moderate dental malocclusion cases were chosen with no overcrowding cases to see the effect of this technique on non extraction cases.
Corticision showed effectiveness in decreasing the treatment time required for completing leveling and alignment of crowded lower incisors, which took an average of 116.46 (±15.97) days in the corticision group compared to 159.69 (±13.76) days in the control group. Corticision reduced the time needed to complete the alignment process by approximately 27%. This effectiveness may be due to the ability of corticision to activate the RAP, stimulate bone remodeling and reinforce blood circulation in the alveolar bone, which leads to acceleration of the orthodontic movement of teeth [8,24].
There have been no published clinical trials on ‘corticision’ using the manual method of a surgical blade and a hammer in the medical literature until now. Acceleration of leveling and alignment has been evaluated recently by only a few studies [11,19]. All of these studies depended on piezosurgery in performing corticotomy and initiating the RAP effect. Charavet C et al., evaluated 24 patients and found a decrease of 43% in the time required to complete alignment with piezosurgery [11], whereas Gibreal O et al., evaluated 36 patients and found a reduction of about 59% in the alignment stage of the piezosurgery-assisted group [19]. In the current trial, a decrease of 27% was found in the time required to complete the alignment with the aid of coriticison.
It should be noted that there are three differences between these three trials; the first one is the degree of crowding, Charavet C et al., study evaluated mild to moderate crowding, whereas Gibreal O et al., study focused on severe crowding requiring extraction, but the current study was conducted on mild to moderate crowding in non extraction cases. The second difference is related to the characteristics of surgical incisions; Gibreal O et al., used five different 3-mm-depth and 5-8-mm-length incisions [19], whereas Charavet C et al., employed incisions using the same depth however shorter lengths [11], but the current trial employed three incisions with a depth of 3 to 4 mm and a length of 4 to 5 mm, and it was the least invasive. The third difference was the instrument used to perform the surgery. Gibreal O et al., and Charavet C et al., used piezoelectric surgery [11,19], while the current trial used a surgical blade and a hammer. Therefore, it was not surprising that the rate of acceleration obtained in the present trial was relatively the lowest among the three studies.
The time required for the correction of crowding in the current trial was less than that reported in Charavet C et al., trial, and this can be explained by the fact that last assessment point in the current trial was at the completion of leveling and alignment, whereas in Charavet C et al., trial it was at the completion of the whole treatment [12]. However, it should be stressed that the benefits of increasing the number and the depth of the surgical incisions to gain extra acceleration are opposed because of the complications that may occur, for example: gingival recession or alveolar dehiscence. Therefore, the original idea of this research work was to make surgical intervention as minimal as possible. Corticision technique by using a surgical blade and a mallet can be considered as a less invasive method, and is characterised by low cost, ease of use, and the possibility to be available in any dental clinic [8] when compared to the piezocision technique whose cost is higher, adverse effects are much more expected and there is a need to purchase the device. The availability of this device in the orthodontic clinic is not straightforward [25-27]. Corticision technique is simply another alternative to promote the RAP effect without additional burden on the orthodontists.
Periodontal Effect
The effect of surgical interventions on periodontal indexes has been evaluated in previous papers using including corticotomy, piezocision [11,12,28], and discision [29], but the evaluation has been performed briefly and superficially.
Periodontal indexes were studied in the current study with great accuracy, and there were no clinically significant differences between the two groups after treatment. This indicated that the corticision procedure was very safe on the periodontal tissue.
The PI increased in buccal, mesial, and distal sides after leveling and alignment, and this increase reflects the effect of the fixed orthodontic appliance on the plaque accumulation. In general, PI values for both groups after leveling and alignment were alignment within clinically acceptable limits, i.e., the minimum value was 0.8, and the greatest value was 1.6 [Table/Fig-5]. There was no change in PI in the lingual side, possibly due to the physiologic cleanings effect of the tongue.
GI increased in the mesial and distal sides after leveling and alignment for both study groups [Table/Fig-5], due to the accumulation of plaque in these areas and the difficulty of maintaining oral hygiene during orthodontic treatment. The values of the GI for both groups after leveling and alignment were within clinically acceptable limits, i.e., the lowest recorded value was 0.5, and the greatest recorded value was 0.9 [Table/Fig-5]. This is related to the fact that PI values after orthodontic treatment were within the clinical acceptable limits. There were no inflammatory signs on the lingual side, as it was an area free from the accumulation of plaque.
There were no statistically significant differences in the PD after leveling and alignment despite the increase in PD on the buccal, mesial, distal side of each of the two groups.
With regard to the gingival recession, the interventional group did not show any clinically significant differences from the control group. This could be attributed to the similar results obtained in the periodontal indices between both groups that laid within the normal range. The point of application was far from the gingival margin (i.e., 3 mm away), and the number of incisions being made were three only.
Limitation(s)
One of the limitations of the current trial is its evaluation of the correction speed in one jaw only instead of both jaws. Secondly, levels of pain, discomfort, and acceptability were not studied in this trial. Regarding hard-tissue changes, there was a need to evaluate possible root resorption or alveolar bony untoward effects using CBCT images. The blinding of patients was not possible in this trial. However, this could not be a source of bias, since no patient-centered self-assessed outcomes were evaluated. Additionally, some periodontal complications that may occur, such as the formation of soft tissue scars in areas of surgical intervention, were not covered in the current trial.
Conclusion(s)
The corticision technique is an effective method to accelerate orthodontic tooth movement in mild to moderate crowding cases in young adult patients. Conventional corticision did not cause negative results on periodontal tissues, especially PD and width of the attached gingiva.
Declaration: This work has been registered at ClinicalTrails.gov; however during the study period of the research project, many deviations from actual study protocol occurred due to logistic reasons. The following changes occurred during the course of the study:
The authors decided to increase the number of patients to be included in the trial, because a further sample size estimation revealed the need for extra patients to arrive at a statistical results with enough power. Therefore, the sample size in this paper is larger than the primary calculated sample size.
According to the previous changes regarding sample size, the research project required longer time to be correctly accomplished. Data analysis and writing up the final report have taken more time than the the originally expected one.
A decision was taken to change the secondary outcome to periodontal indices. This was because the captured CBCT images were found to have some problems regarding size standardisation, resolution, and clarity. The authors have applied and are trying to update the submitted protocol.