Hypertension in adolescence is one of the most alarming public health issues now-a-days and is a potential risk factor for cardiovascular and cerebrovascular diseases. Primary or essential HTN was once thought to be rare but is presently showing an increasing trend in children and adolescents. The current prevalence of HTN among adolescents is estimated to be 1-5%, worldwide [1].
The HTN in childhood and adolescence is mainly asymptomatic and can be easily missed by healthcare professionals. Blood pressure measurement has not been included in elementary school children health examination schedule. Thus, HTN in adolescents if remain undiagnosed, persists into adulthood, resulting in considerable cardiovascular morbidity.
The HTN and its complications are one of the leading causes of death worldwide. About 1 billion adults had HTN around the world in the year 2000 and it is expected to rise to 1.56 billion by 2025 [2,3].
Prevalence of HTN among school going children and adolescents ranges between 4.5-6.4% in India [4,5].
Early detection of HTN and associated risk factors like obesity among adolescents is essential to prevent the long term adverse effects on individual health. Many studies have shown significant positive association between blood pressure and obesity/overweight [6-9].
In recent years, obesity in childhood and adolescence is also emerging as a common public health issue worldwide involving both developed and developing countries. Various studies reflect the prevalence of overweight and obesity among Indian adolescents as 9-27.5% and 1-12.9%, respectively [6-9]. Studies conducted in India from 2002-2012 showed an increasing trend in prevalence of overweight and obesity in children and adolescents [10].
Body Mass Index (BMI) has been used to measure general obesity. WC is used to measure central obesity. NC is a marker of upper body subcutaneous adipose tissue distribution [11,12]. Body fat percentages as an anthropometric indicator had been proven to be an effective approach in predicting HTN [13].
The increasing trends, specially in urban area, of consuming high energy dense ready to eat food and soft drinks along with low level of physical activity, increasing use of technological gadgets are the most common contributory factors of obesity among adolescents. Such unhealthy lifestyle leads to increasing trends of comorbidities with metabolic risk factors like HTN, type II diabetes mellitus, high blood cholesterol level, atherosclerosis and other non-communicable diseases [14,15].
Different studies show that there is a relationship between obesity and HTN. Weight gain leads to accumulation of fats like cholesterol in the body which may build-up plaque inside blood vessels and results in high blood pressure and other serious conditions like cardiovascular diseases [14,15].
Apart from BMI there are several anthropometric parameters like WC and NC, body fat percentage. If any significant relationship is found between these anthropometric measures with HTN, these anthropometric measures can be utilised for early screening of HTN. These measures can also be used in case where height or weight measurement is difficult [15,16].
Anthropometric measurements are simple for application and easy to interpret and thus, can be used as a screening method to detect the presence of HTN among adolescents. It can be implemented in school health set up for early detection of HTN. After that primordial preventive measure can be taken at this stage of adolescence period either by lifestyle modification or treatment. Thus, the detrimental consequences of HTN, which would affect subsequently at adulthood, can be prevented.
From the review of literature this is much clear that there is a close relationship between blood pressure and obesity among adults. However, such evidence among adolescence age group in the urban area in West Bengal is limited. So the present study was undertaken to find out the magnitude of HTN among adolescent school students and to find out the variation of blood pressure with different anthropometric parameters and its associated factors.
Materials and Methods
The present cross-sectional study was undertaken during the period of June to August 2019 in two Government Higher Secondary Schools of South Dumdum Municipality of North 24 Parganas.
Sample Size Calculation
Taking prevalence of HTN and pre HTN among adolescent school students as 30.3% from a previous study in Kolkata [17] in 2015, the formula of (Z)2×p×(1-p)/L2 where p=0.303, Z (95% CI)=1.96, 20% relative error (L), minimum sample size was calculated as 221. Taking design effect d=1.5, and 10% non-response rate, the final sample size was calculated as 364.6 i.e., 365.
Out of 16 Government Higher Secondary Schools of South Dumdum Municipality, two schools were selected conveniently. All the students of class VIII to class XII were included in this study. Each school has enrollment of 60 students in each class i.e., almost 300 students in five classes (VIII-XII) and absent rate is 20% on an average. Though the sample size was calculated as 365 but total 369 students were examined. This is because we could not ignore four more students, willing to take part in this study in the same set-up.
Questionnaire
A questionnaire was prepared and then translated to Bengali language and translated back again in English language. Semantic equivalence was seen with final English version. The face validity of all questions and content validity of all domains were conducted by experts. Then, it was pretested on 30 students in a separate Government Higher Secondary School. The test of reliability was found as cronbach’s α which was 0.52.
After taking IEC approval from Institutional Ethical Committee, permission was taken from the head of the institute of the two Government Higher Secondary Schools for conducting this research. Informed written consent from the willing students of class VIII to class XII and from the parents of the participants were taken before conducting this research. Each school was visited for three days by our team of researchers and all students were examined in presence of their teachers. Students, those were absent during the days of visit, those were not willing to participate and those who were prediagnosed as hypertensive or had any illness that could lead to secondary HTN were excluded from this study.
Data Collection
Data was collected by face to face interview, blood pressure recording and anthropometric measurements of all participants was done by a team of researchers. A predesigned pretested structured schedule including socio-demographic information, family history of HTN, food habit, physical activity status was used.
Anthropometric measurement was done using standard calibrated equipment. A portable weighing machine was used to measure weight to the nearest 100 gm. Participants were weighed with light clothing and standing without footwear. Height was measured with an anthropometric height board to the nearest 0.1 cm. Students were asked to stand upright without footwear with their back of heels and occiput against the equipment while measuring height.
The BMI was calculated with weight and height; and plotted into World Health Organisation (WHO) BMI chart adjusted with age and sex to categorise as underweight, normal, overweight, and obese.
A non-stretchable measuring tape was used to measure WC and NC. WC was measured at the midpoint between the last rib and iliac crest with minimal clothing. The participants were asked to relax their abdomen and stand upright. The cut-off value for WC for screening adolescent obesity in boys and girls were 70.75 cm and 69.25 cm, respectively (Indian Paediatrics) [18].
The NC was measured in horizontal plane at the level of thyroid cartilage while participants were asked to stand with head upright and look forward. Cut-off value for NC for screening adolescent obesity in boys and girls were 30.75 cm and 29.75 cm, respectively (Indian Paediatrics) [19].
Body fat percentage was measured using Standardised electronic body fat/hydrating scalar EEF2003A machine (Eagle). Students were asked to stand on the machine with light clothing and without footwear and body fat percentage were recorded after adjusting their age, sex and height.
Mean of two consecutive reading was noted for height, weight, WC, NC, body fat percentage.
Blood pressure was measured in the left arm by auscultatory method using a standard aneroid sphygmomanometer, (calibrated with a mercury sphygmomanometer) with appropriate cuff size for arm circumference in sitting position after taking rest for five minutes. The first and fifth Korotkoff sounds were recorded as SBP and DBP, respectively. Blood pressure measurements were taken twice with an interval of one minute. The final measurement was noted as the average of both records. Subjects with SBP and/or DBP equal to or greater than the 95th percentile for gender, age and height were considered to be hypertensive, and subjects with SBP and/or DBP levels equal to or greater than the 90th percentile but less than the 95th percentile for that gender, age and height were considered to be prehypertensive [20-24].
Regular physical activity was assessed according to WHO criteria, which is defined as- “Children and youth aged 5-17 years should accumulate at least 60 minutes of moderate to vigorous-intensity physical activity daily” [25].
Statistical Analysis
Statistical analyses were done using IBM Statistical Package for Social Sciences (SPSS) version 16.0. Descriptive and inferential statistical analysis was performed with confidence interval of 95% and p-value of less than 0.05 was regarded as level of significance. For inferential analysis, pre HTN is regrouped into HTN, to achieve dichotomous dependent variables, normotensive and hypertensive. Spearman correlation test was done to find out the correlation between blood pressure and different anthropometric measurements. Univariate and multivariable logistic regression model were used to find out any associated factors of HTN.
Results
Out of total 369 students examined, 189 (51.2%) were boys and 180 (48.8%) were girls. Their age ranged between 13 to 17 years with mean age of 14.8 (±1.2) and median (IQR) of 15 (14,15).
A total of 41.5% of all participants had positive family history of HTN. A 33.6% of participants took extra salt sometimes and 9.8% took it regularly along with meals. Out of total, 45.3% participants took junk food 1-2 days a week, 14.4% took it 3-4 days a week and 1.4% took junk food more than five days a week. A 76.4% of study subjects did not perform physical activity regularly.
Overall, 13.8% of participants were prehypertensive and 7.0% of total participants were hypertensive [Table/Fig-1]. Mean SBP among boys were 110.2 mmHg (±14.9) and among girls it was 113.1 mmHg (±14.3). The mean DBP among boys was 68 mmHg (±9.3) and among girls was 71.2 mmHg (±9.0) [Table/Fig-2].
Blood pressure status among study subjects (n=369).
| Blood pressure | Boys (n=189) Number (%) | Girls (n=180) Number (%) | Total (n=369) Number (%) |
|---|
| Normotensive | 154 (81.5) | 138 (76.6) | 292 (79.2) |
| Prehypertensive | 23 (12.2) | 28 (15.6) | 51 (13.8) |
| Hypertensive | 12 (6.3) | 14 (7.8) | 26 (7.0) |
Distribution of study participants according to presence of Systolic and Diastolic Blood Pressure (SBP and DBP) and Age group (N=369).
| Sex | Age in years | Number | SBP (Mean) | SBP (SD) | DBP (Mean) | DBP (SD) |
|---|
| Boys | 13 | 61 | 101.2 | 14.6 | 64.9 | 9.5 |
| 14 | 44 | 109.8 | 11.0 | 67.7 | 8.2 |
| 15 | 51 | 116.9 | 13.6 | 69.8 | 8.6 |
| 16 | 31 | 118.9 | 14.5 | 71.4 | 9.8 |
| 17 | 2 | 119 | 12.7 | 72 | 8.2 |
| Girls | 14 | 65 | 114.9 | 14.9 | 71.6 | 8.7 |
| 15 | 23 | 112.5 | 14.1 | 70.4 | 8.2 |
| 16 | 48 | 111.8 | 14.5 | 71.2 | 9.54 |
| 17 | 44 | 112.9 | 13.8 | 71.1 | 9.54 |
According to BMI, 24.9% boys were overweight and 19% were obese whereas 25% girls were overweight and 10% were obese. According to WC, 40.3% of boys were found to be obese {Mean (SD)=78.9(±11.9)} and 43.9% girls were found to be obese {Mean (SD)=77.4(±10.5)}. As per NC, 29.6% boys {Mean (SD)=32.9(±2.8)} and 31.7% girl were obese {Mean (SD)=30.6(±2.4)}. The readings of body fat percentage showed that 24.9% of boys {Mean (SD)=17.6(±7.8)} and 37.8% girls were obese {Mean (SD)=25(±9.5)}.
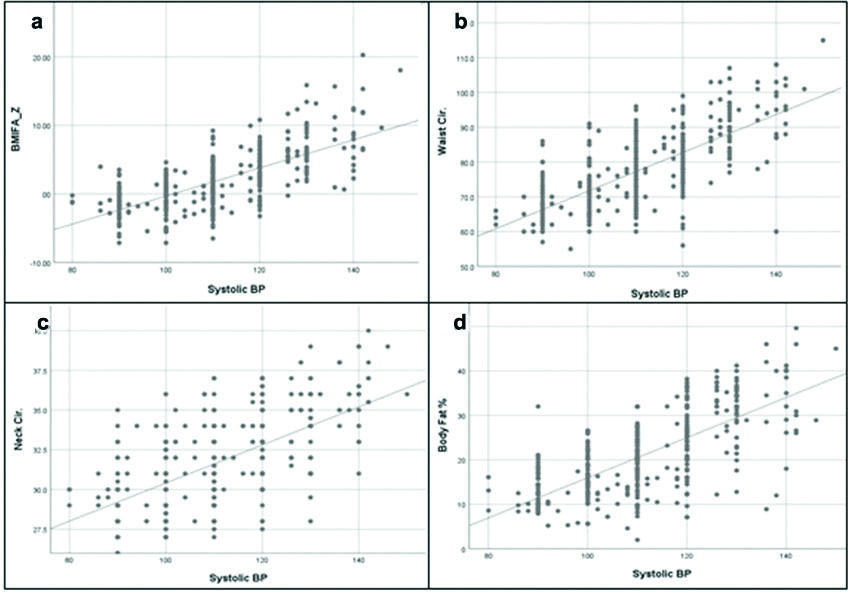
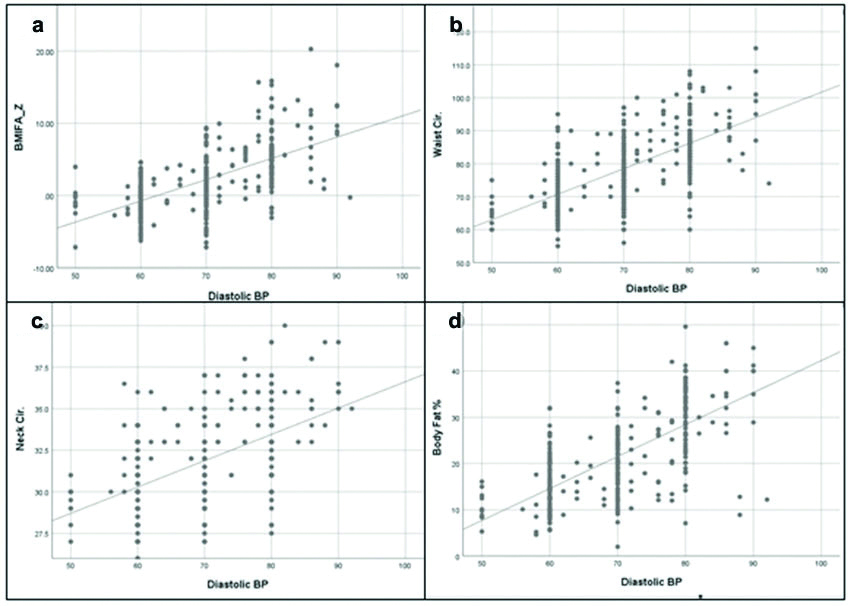
The Spearman correlation showed that there were significant (p<0.01) positive correlation of SBP with BMI-Z score, body fat percentage, WC, NC. This test also showed significant (<0.01) positive correlation of DBP with BMI-Z, body fat percentage, WC, NC [Table/Fig-3,4a-d,5a-d].
Spearman Correlation of SBP and DBP with Anthropometric Parameters (N=369).
| Variables | BMI-Z | Body fat percentage | WC | NC |
|---|
| SBP | 0.692* | 0.686* | 0.705* | 0.593* |
| DBP | 0.673* | 0.676* | 0.640* | 0.509* |
*Significant at level of <0.01
Scattered Diagram showing correlation between Systolic BP (SBP) and anthropometric measurements. a) Showing correlation between SBP and BMI-Z score; b) Showing correlation between Systolic BP (SBP) and Waist Circumference (WC); c) Showing correlation between Systolic BP (SBP) and Neck Circumference (NC); d) Showing correlation between Systolic BP (SBP) and Body Fat Percentage
Scattered Diagram showing correlation between Diastolic BP (DBP) and anthropometric measurements. a) Showing correlation between DBP and BMI-Z score; b) Showing correlation between Diastolic BP (DBP) and Waist Circumference (WC); c) Showing correlation between DBP and Neck Circumference (NC); d) Showing correlation between Diastolic BP (DBP) and Body Fat Percentage.
In multivariable logistic regression, regular salt intake had 3.04 times higher chance of having HTN when adjusted with other risk factors and obese had 1.65 times higher chance of having HTN when adjusted with other risk factors. No regular physical activity also had 3.19 times higher chance of having HTN from those who perform regular physical activity. Though obesity can be assessed by BMI, WC, NC, body fat percentage; only BMI-Z score was taken while performing logistic regression [Table/Fig-6].
Factors Associated with Hypertension (HTN): Univariate, Multivariable Logistic Regression (N=369).
| Variable | Subgroup (%) | OR | CI | AOR | CI |
|---|
| Sex | Female (23.4) | 1.33* | 0.8-2.2 | - | - |
| Extra Salt intake | Regular (61.1) | 3.82* | 2.5-5.6 | 3.04* | 1.8-5.0 |
| Physical activity | No (23.8) | 3.19* | 1.4-6.9 | - | - |
| BMI-Z score | - | 1.67* | 1.4-1.8 | 1.65* | 1.4-1.8 |
Nagel Karke =0.57 and Cox-Snell R2=0.38. *significant at the level <0.05
Discussion
Current study showed that the prevalence of HTN and pre HTN was 7.0% and 13.8%, respectively, whereas Maiti M and Bandyopadhyay L, in their study conducted among adolescent students in Kolkata showed that prevalence of HTN (10.1%) and pre HTN (20.2%) were higher. This higher prevalence may be because the previous study was conducted in a school of slum area [17].
Kumar P et al., showed that prevalence of HTN among school going adolescents was 4.5% in north India and Charan J et al., showed that prevalence of HTN among school going adolescents was 6.48% in western India which was in concordance with present study [4,5].
Another study conducted by Ujunwa FA et al., showed that prevalence of HTN and pre HTN was 5.4% and 17.3%, respectively where the prevalence of HTN was lower than the present study but in case of pre HTN it was higher [26].
Fan Z et al., also showed that prevalence of HTN and pre HTN was 10.6% and 6.0%, respectively. Here, the prevalence of HTN was higher but the prevalence of pre HTN was much lower than the present study [27].
The present study showed that the mean SBP and DBP among boys were 110.2 mm Hg (±14.9) and 68 mm Hg (±9.3), respectively and in case of girls, these were 113.1 mm Hg (±14.3) and 71.2 mm Hg (±9.0), respectively. Similar results were found by Ujunwa FA et al., where the mean SBP and DBP among boys was 106.6 mmHg (±11.8) and 70.25 mm Hg (±7.34) and for girls it was 109.8 mm Hg (±11.6) and 72.2 mm Hg (±8.2), respectively [26].
Mahajan A and Negi PC, in his study conducted in Shimla, showed that prevalence of HTN was higher in females (13.1%) than in males (9.5%) and prevalence of pre HTN was almost same in both the groups i.e.,11.0% in females and 11.3% in males. In the present study, prevalence of HTN was higher in females (7.8%) than in males (6.3%) and prevalence of pre HTN was also higher in females (15.6%) than in males (12.2%) [28].
The present study showed that there was significant positive correlation between HTN with BMI, body fat percentage, WC, NC. Okpokowuruk FS et al., showed significant positive correlation between HTN and age, BMI, WC [29]. Mahajan A and Negi PC, also showed there was significant association of HTN and BMI for age in both the genders [28].
According to Cheah WL et al., the best anthropometric indicators for predicting HTN for boys were WC, BMI, and Waist To Height Ratio (WHtR) and for girls, BMI was the best indicator followed by WHtR and WC [30].
Kundu RN and Biswas S, showed a significant positive correlation (r=0.404) between BMI and Mean Arterial Pressure. Significant difference was showed between Mean Arterial Pressure of obese and non-obese persons. The study suggests that, the effect of obesity is present on blood pressure. However, the study was conducted among adult males in rural area of North 24 Parganas [14].
Limitation(s)
The present study was cross-sectional in nature and so it could not establish the directionality of the causality. There might be socially desirable response in questions related to behavioural aspect like diet and physical activity.
Conclusion(s)
The Prevalence of pre HTN and HTN was high among adolescents. There are significant positive correlation of SBP and DBP with BMI, NC, WC and body fat percentage. HTN was also significantly associated with physical inactivity and salt intake. Anthropometric measurements are simple, easy to implement and interpret in school health setup and thus can be used as a screening method to detect the presence of HTN among adolescents at an early stage.
Strengthening of school health set up for early detection of HTN and its modifiable risk factors is the need of the hour. Adolescence period is the appropriate stage of life to provide them primordial prevention and protect them from suffering from various noncommunicable diseases in adulthood. Lifestyle modification like encouraging them on healthy diet, not to take extra salt with meal, to avoid junk foods, to perform regular physical activity along with early detection and treatment of HTN must be implemented in school health policy.
As there was significant correlation of blood pressure with anthropometric measurements, the students who have high BMI, NC, WC, body fat percentage should be referred to medical personal from school level for further measurement of blood pressure and should be advised for lifestyle modification as early as possible.
Early detection of HTN in adolescents’ age in school set up will help to prevent HTN and its detrimental consequences in their adulthood either by lifestyle modification or with medication. It will enable the people to lead a healthy life.
*Significant at level of <0.01
Nagel Karke =0.57 and Cox-Snell R2=0.38. *significant at the level <0.05