Management of Peripartum Cardiomyopathy with Secondary Large Left Ventricular Apical Clot using Novel Oral Anticoagulants: A Case Report
Mrigakshi Aggarwal1, Manav Aggarwal2, Prem Aggarwal3
1 Consultant Physician, Department of Cardiology, Sanjeevan Medical Research Centre (P) Ltd., New Delhi, India.
2 Cardiologist, Department of Cardiology, Sanjeevan Medical Research Centre (P) Ltd., New Delhi, India.
3 Consultant, Department of Cardiology, Sanjeevan Medical Research Centre (P) Ltd., New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Manav Aggarwal, Cardiologist, Department of Cardiology, Sanjeevan Medical Research Centre (P) Ltd., New Delhi, India.
E-mail: manav19@gmail.com
Peripartum Cardiomyopathy (PPCM) is a major life-threatening complication of pregnancy, as only half of them or slightly more patients show improvement of Left Ventricular (LV) dysfunction. A 28-year-old woman with a history of gestational hypertension and diabetes during pregnancy, underwent full-term normal vaginal delivery. She started developing dyspnea, Class II which progressed to Class IV postpartum. Kidney and liver functions were found to be grossly deranged along with thrombocytopenia. Provisional diagnosis of Haemolysis, Elevated Liver Enzymes and Low Platelets (HELLP) was made. Electrocardiography (ECG) revealed the left anterior fascicular block. Eventually, bedside echocardiogram revealed severe LV dysfunction and the presence of a large soft LV apical clot with an Ejection Fraction (EF) of 30%. Adequate anticoagulation was achieved using Novel Oral Anticoagulants (NOAC). After six days and a 3-month follow-up, an echocardiogram demonstrated a significant improvement of LV function (EF-45%) and a complete resolution of LV apical clot, respectively.
Complication of pregnancy, Gestational hypertension, Ventricle thrombus
Case Presentation
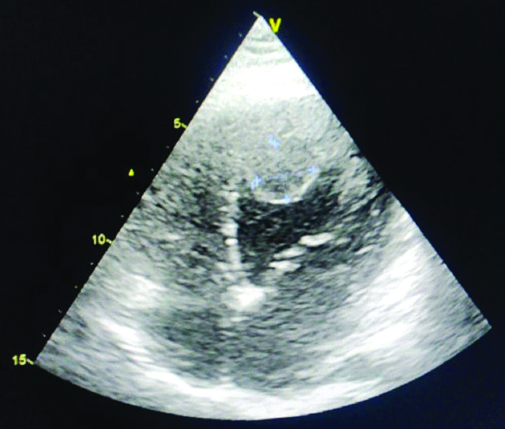
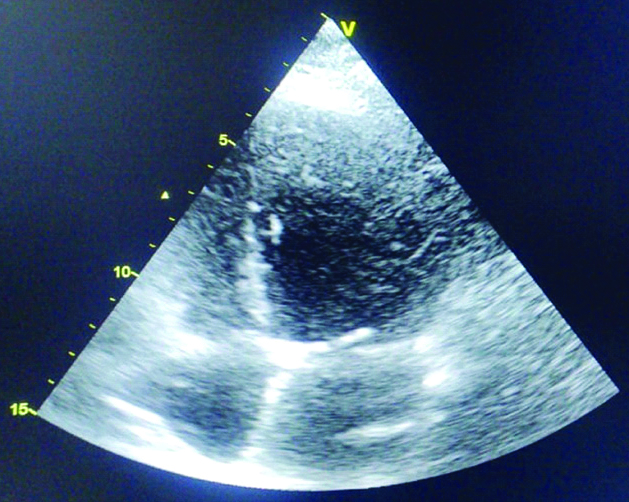
A 28-year-old woman, G2P1L1 full-term normal vaginal delivery, 8-month previously presented with a history of gestational hypertension and diabetes during pregnancy. Patient underwent full-term normal vaginal delivery on 30th August 2019. On 26th August patient started by developing dyspnea, Class II which progressed to Class IV [1] within the next four days. After discharge, her dyspnoea got worsened, diabetes and hypertension were not normalised as the patient was noncompliant with no significant medical history. The patient presented again on 4th October with epistaxis, nasal congestion and complaints of orthopnea, paroxysmal nocturnal dyspnea which were progressively increasing. Routine blood investigations were done and are represented in [Table/Fig-1]. The kidney and liver function found to be grossly deranged. Haemogram showed thrombocytopenia. HELLP syndrome was suspected. However, ECG showed left anterior fascicular block and T-wave abnormality in leads I, II, aVL, V1, V4, V5 and V6. Bedside echocardiogram was done which revealed severe LV dysfunction and presence of large soft LV apical clot (measuring 2.2×2.1 cm), with EF 30% [Table/Fig-2]. The patient was given platelet transfusion and started on heparin injections but the activated partial thromboplastin time was suboptimal within the next four days after treatment. Higher doses of heparin were avoided, in view of thrombocytopenia and risk of postpartum haemorrhage. It was then decided to start the NOAC and the patient was started on Dabigatran (150 mg BD), along with Angiontensin Receptor-Neprilysin Inhibitor (ARNI-Sacubutril/Velsartain 50 mg BD) and Beta-blocker (Carvidelol 3.125 mg BD) for heart failure. The patient was discharged on 15th October with the same prescribed medication for six days. After six days, review echocardiogram was done again on an OPD basis which revealed significant improvement of LV function (EF-45%) and complete resolution of LV apical clot [Table/Fig-3]. Her follow-up echocardiogram three months later revealed the same findings (EF-53%) and the patient is doing well and is advised to continue Dabigatran for at least six months. There was no adverse event observed at follow-up.
Laboratory Investigation.
| Parameters | Values |
|---|
| Platelet count | 38000 μL |
| Haemoglobin | 13.6 g/dL |
| Urea | 120 mg/dL |
| Creatinine | 2.0 mg/dL |
| Uric acid | 10.0 mg/dL |
| Calcium | 8.1 mg/dL |
| Phosphate | 4.0 mg/dL |
| Sodium | 136.0 mequiv./l |
| Potassium | 4.9 mequiv./l |
| Chloride | 103.0 mequiv./l |
| Bilirubin total | 2.93 mg/dL |
| Bilirubin direct | 1.51 mg/dL |
| Bilirubin indirect | 1.42 mg/dL |
| Serum glutamicoxaloacetic transaminase | 3228 IU/L |
| Serum glutamic pyruvic transaminase | 4139 IU/L |
| Alkaline phosphatase | 161.0 IU/L |
| Protein | 5.1g/dL |
| Albumin | 2.4 g/dL |
| Globulin | 2.7 g/dL |
| Albumin to globulin ratio | 0.8 |
| Gamma-glutamyltransferase | 189.0 IU/L |
Echocardiography revealed severe LV dysfunction and presented large soft LV apical clot.
Echocardiography revealed significant improvement of LV function and complete resolution of LV apical clot.
Discussion
The PPCM is an atypical condition of pregnancy-related myocardial disease in which the heart muscle is structurally and functionally weak, characterised by LV systolic dysfunction. The risk factors include multiple pregnancies, multiparity, advanced maternal age, gestational and pregnancy co-morbidities such as pulmonary embolism and eclampsia [2]. Although, PPCM which includes dyspnea and tachycardia, are common symptoms among these patients, other symptoms such as fatigue, oedema and palpitation may also be observed [3]. Thus, diagnosis is often delayed and under-recognised with disturbing consequences. However, more than half of the cases accomplish spontaneous and complete recovery of LV dysfunction after gestation. The other cases show a much more progressive disorder, for which intensive management and even heart transplantation may be needed [4]. The prevalence of LV thrombus is associated with potentially severe complications and high rates of thromboembolic events such as stroke [5,6]. NOAC therapy is useful in the prevention of systemic embolism and stroke [7].
The PPCM is a life-threatening cardiovascular disorder which usually develops during the peripartum period [8]. The PPCM includes the following diagnostic criteria: development of cardiac failure occurring within five months after delivery or last month during pregnancy; no certain cardiovascular disease before the last month of pregnancy; no identifiable cause for the cardiac failure; and LV dysfunction and EF≤45% [4]. The present case met all the diagnostic criteria. The diagnosis of PPCM related to its presentation and recovery of ventricular dysfunction. The outcome is based on the LV end-diastolic volume and EF at diagnosis, normalisation of LV function during the six months of pregnancy [3]. PPCM is a particular form of cardiac failure with undetermined pathogenesis, and a wide spectrum of different clinical manifestations. The most PPCM cases are detected and treated by cardiologists for cardiac arrhythmia or failure at postpartum. Moreover, the LV function rate of full recovery is lower in patients with more progressive cardiac failure, thus emphasising the importance of the impact of timely diagnosis [9].
The HELLP syndrome occurs in less than 1% of pregnancies during the initial days after delivery or third trimester. The syndrome is related to microangiopathic haemolytic anaemia secondary to general activation of the coagulation cascade. The present case was an association between HELLP syndrome, diagnosed with PPCM during the last stage, and G2P1L1 full-term normal vaginal delivery.
Therapy for the cardiac disorder include angiotensin and beta-receptor blockers, which can be considered for PPCM treatment after delivery [3]. Patients with considerably depressed LV function and EF less than or equal to 35% may benefit from NOAC therapy to reduce coagulation of blood and emboli. LV functions in 78% of women fully recovers and have a normal outcome.
Yamamoto T et al., reported that LV thrombus formation resolved by Dabigatran (220 mg/day) treatment [10]. Ohashi N et al., reported that Dabigatran may be a therapeutic option in a patient with LV thrombus [11]. Kolekar S et al., also demonstrated the probable thrombolytic property of Dabigatran in LV thrombus [6]. However, this case also showed that LV thrombi can be successfully treated with NOAC. In this case, significant improvements in LV function with EF-53% were present at the follow-up. This finding supports the thrombolytic action of NOAC i.e., dabigatran due to its particular binding to both free and clot-bound active thrombin molecules [6]. A previous study reported that dabigatran was highly effective in LV clot patients [12]. Additionally, no clot recurrence or new clot formation at follow-up were found.
Conclusion(s)
NOAC might be effective in improving LV dysfunction and results in rapid LV clot resolution in PPCM. It can be safely used without increased risk of bleeding.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 02, 2020
Manual Googling: Aug 22, 2020
iThenticate Software: Sep 28, 2020 (2%)
[1]. Ballo P, Betti I, Mangialavori G, Chiodi L, Rapisardi G, Zuppiroli A, Peripartum cardiomyopathy presenting with predominant left ventricular diastolic dysfunction: Efficacy of bromocriptineCase Reports in Medicine 2012 2012:47690310.1155/2012/47690323251175 [Google Scholar] [CrossRef] [PubMed]
[2]. Huang Y, Chen T, Zhang M, Yang X, Ding G, Yang L, Successful management of fatal peripartum cardiomyopathy in a young pregnant woman: A case reportMedicine 2018 97(15):e040810.1097/MD.000000000001040829642207 [Google Scholar] [CrossRef] [PubMed]
[3]. Chaudhari S, Gupta P, Bal H, Bhikane DB, A rare case of peripartum cardiomyopathyMedical Journal of Dr DY Patil University 2014 7(6):77710.4103/0975-2870.144880 [Google Scholar] [CrossRef]
[4]. Roche-Kelly E, Nelson-Piercy C, Managing cardiovascular disease during pregnancy: Best practice to optimize outcomesFuture Cardiology 2014 10(3):421-33.10.2217/fca.14.2124976478 [Google Scholar] [CrossRef] [PubMed]
[5]. McCarthy C, Murphy S, Venkateswaran RV, Singh A, Chang LL, Joice MG, Left Ventricular Thrombus. Contemporary Etiologies, Treatment Strategies, and OutcomesJ Am Coll Cardiol 2019 73(15):2007-09.10.1016/j.jacc.2019.01.03130846340 [Google Scholar] [CrossRef] [PubMed]
[6]. Kolekar S, Munjewar C, Sharma S, Dabigatran for left ventricular thrombusIndian Heart Journal 2015 67(5):49510.1016/j.ihj.2015.06.01026432747 [Google Scholar] [CrossRef] [PubMed]
[7]. Mekaj YH, Mekaj AY, Duci SB, Miftari EI, New oral anticoagulants: Their advantages and disadvantages compared with vitamin K antagonists in the prevention and treatment of patients with thromboembolic eventsTherapeutics and Clinical Risk Management 2015 11:967-77.10.2147/TCRM.S8421026150723 [Google Scholar] [CrossRef] [PubMed]
[8]. Arany Z, Elkayam U, Peripartum cardiomyopathyCirculation 2016 133(14):1397-409.10.1161/CIRCULATIONAHA.115.02049127045128 [Google Scholar] [CrossRef] [PubMed]
[9]. Loyaga-Rendon RY, Pamboukian SV, Tallaj JA, Acharya D, Cantor R, Starling RC, Outcomes of patients with peripartum cardiomyopathy who received mechanical circulatory support: Data from the interagency registry for mechanically assisted circulatory supportCirculation: Heart Failure 2014 7(2):300-09.10.1161/CIRCHEARTFAILURE.113.00072124443515 [Google Scholar] [CrossRef] [PubMed]
[10]. Yamamoto T, Konishi T, Funayama N, Kikuchi B, Hotta D, Ohori K, Resolution of left ventricular thrombus after dabigatran therapy in two patients with old anteroseptal myocardial infarctionCardiol Pharmacol 2015 4:15210.4172/2329-6607.1000152 [Google Scholar] [CrossRef]
[11]. Ohashi N, Okada T, Uchida M, Amioka M, Fujiwara M, Kaseda S, Effects of dabigatran on the resolution of left ventricular thrombus after acute myocardial infarctionInternal Medicine 2015 54(14):1761-63.10.2169/internalmedicine.54.419126179532 [Google Scholar] [CrossRef] [PubMed]
[12]. Verma B, Singh A, Kumar M, Use of dabigatran for treatment of left ventricular thrombus: A tertiary care center experienceJ Family Med Prim Care 2019 8(8):2656-660.10.4103/jfmpc.jfmpc_98_1931041219 [Google Scholar] [CrossRef] [PubMed]