Case Report
A 37-year-old female patient presented to the Department of Dentistry with the chief complaint of pain in the region of the temporomandibular joints which was worsening for the last three years. The patient reported a sharp intermittent lancinating pain while swallowing and performing neck movements. She also reported discomfort while swallowing, talking, and opening her mouth and a sensation of something being stuck in the throat. She presented with clicking sounds while opening the mouth.
The patient denied having allergies, chronic and infectious diseases and controlled use medications. The patient reported having undergone previous dental treatments without complications. She also reported that she had previously sought treatment for the condition, which had been diagnosed as temporomandibular disorder.
On extraoral examination, the patient had a symmetrical face, pain-free and palpable condyles and mouth opening of approximately 40 mm. She had a hardened structure in the right carotid region associated with pain on palpation.
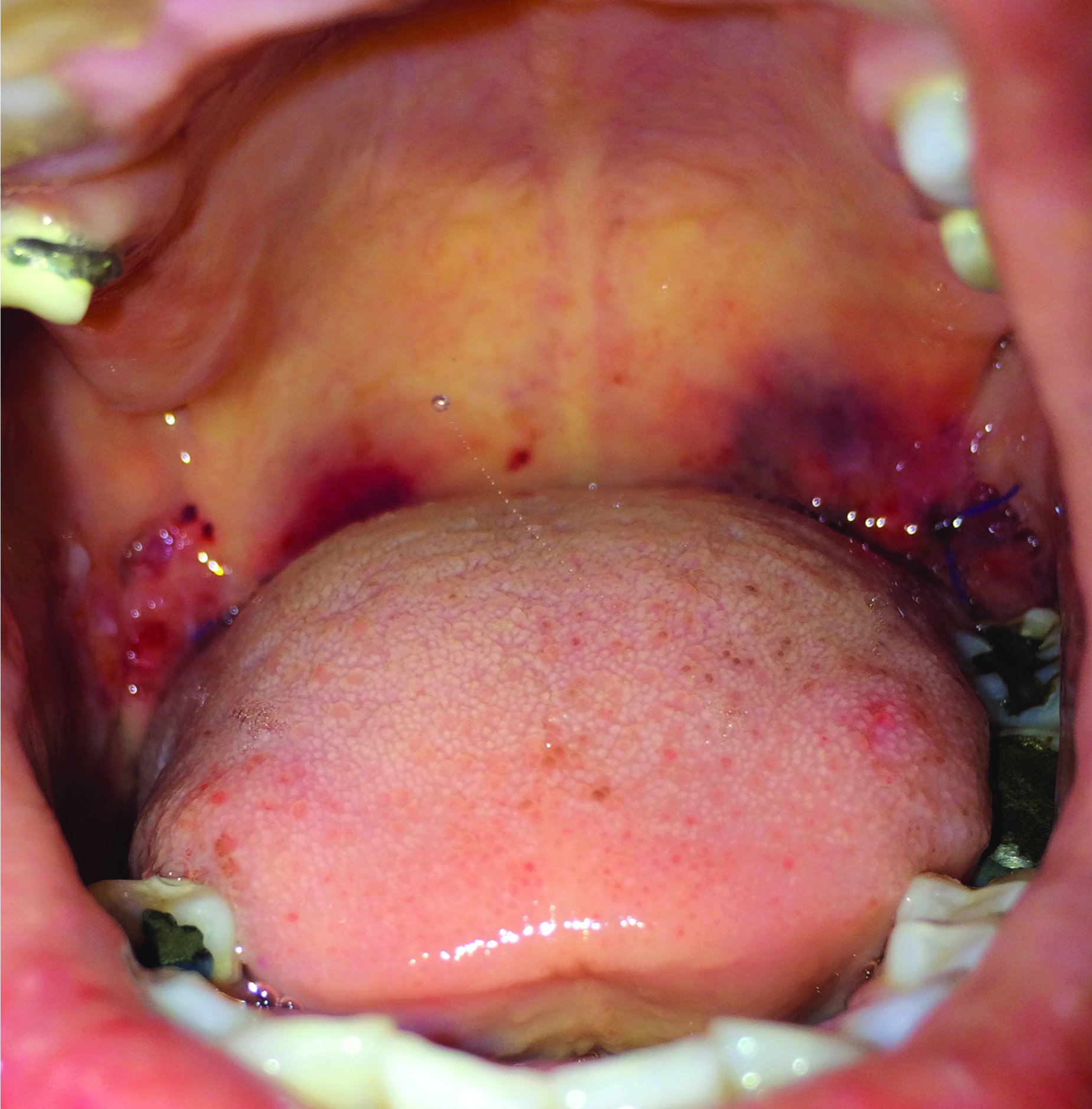
The intraoral physical examination presented healthy and normocorate mucous membranes, absence of several teeth in the maxilla and mandible, and the use of removable partial prosthesis in the maxilla. In the region of the tonsillar pillar, a solid and immobile structure was palpated bilaterally. The patient reported pain during palpation.
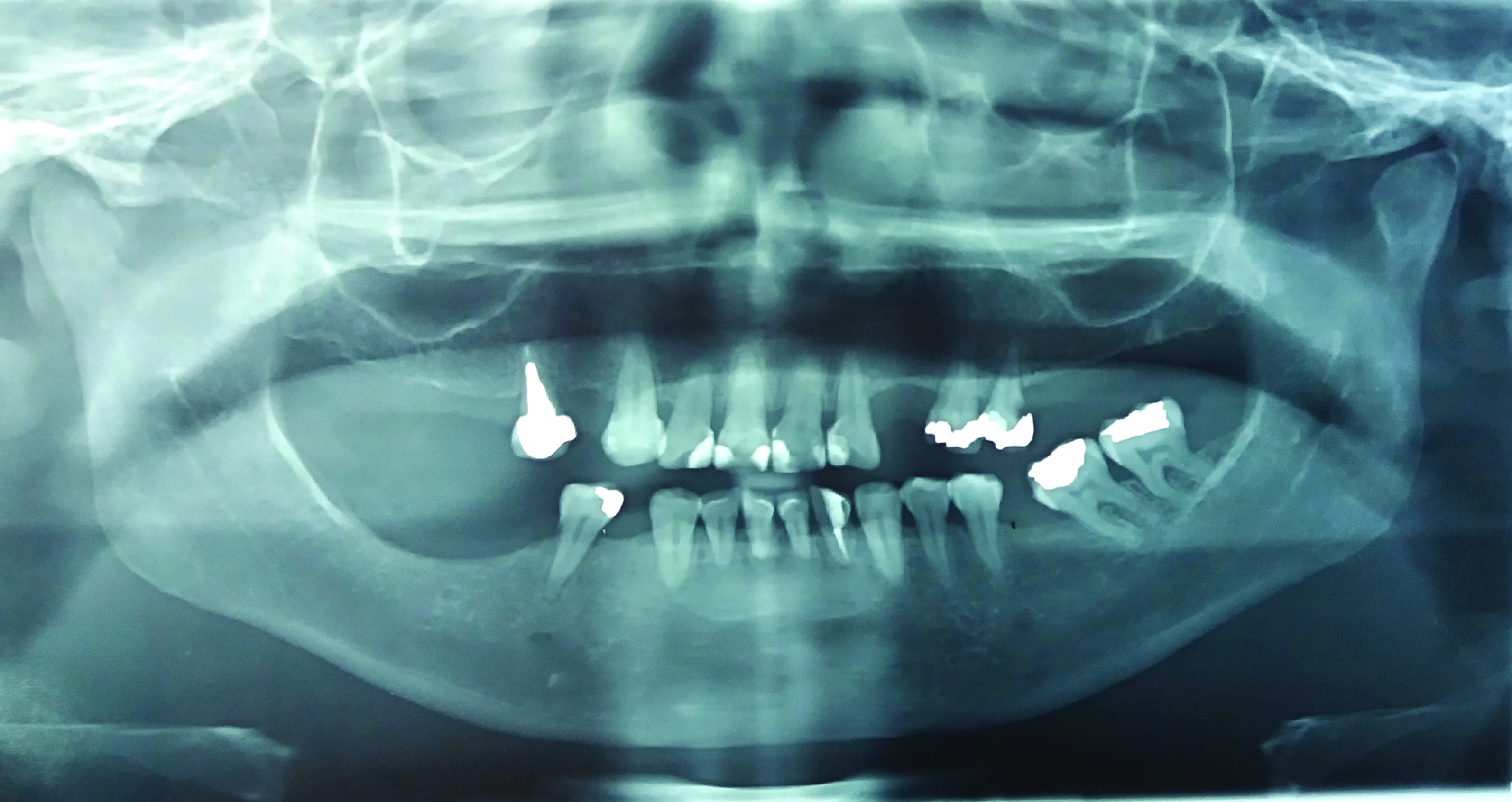
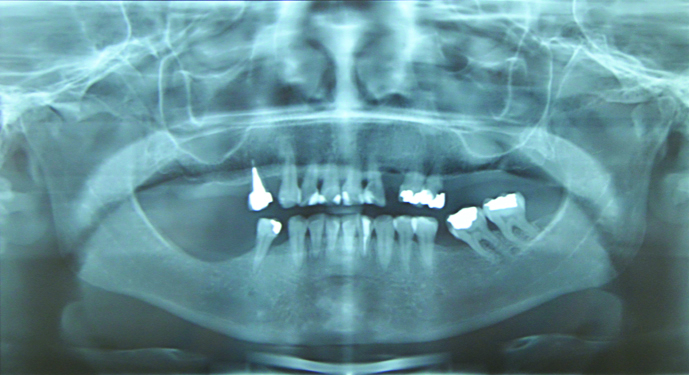
Panoramic radiographic examination revealed radiopaque structures in the region of the styloid processes of the temporal bones suggestive of elongation of the styloid process and completely mineralised styloid ligament forming a pseudoarticulation [Table/Fig-1].
Panoramic radiograph suggestive of elongated styloid processes.
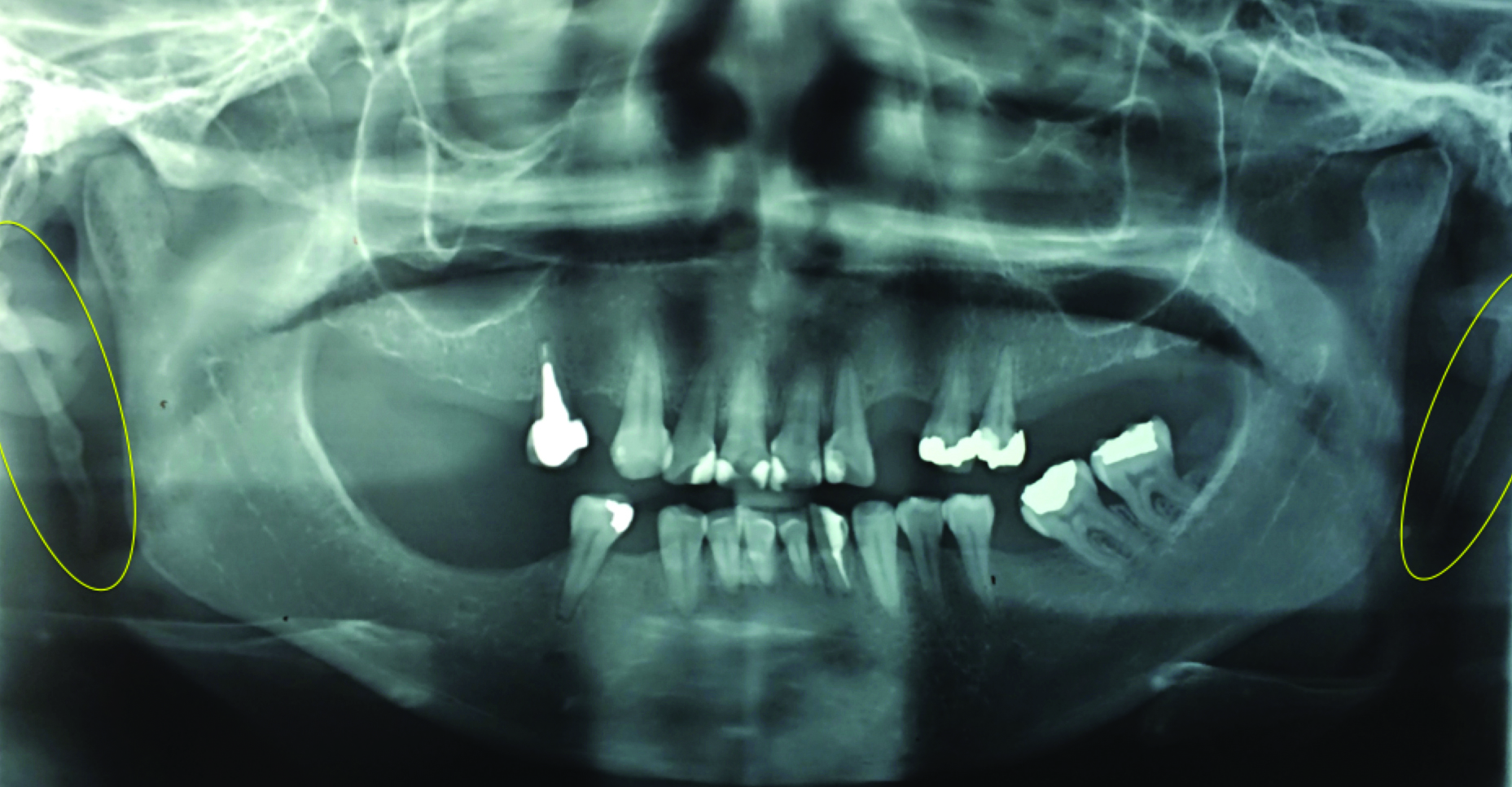
The symptoms reported by the patient could also have been due to trigeminal neuralgia or a tumour in the region of tonsillar fossa. However, the radiographic image of the bilateral elongated styloid processes and the hard fixed structures suggestive of styloid processes felt in intraoral and extraoral palpation, combined with the patient’s description of pain during swallowing and moving the neck, led to the diagnostic hypothesis of Eagle syndrome.
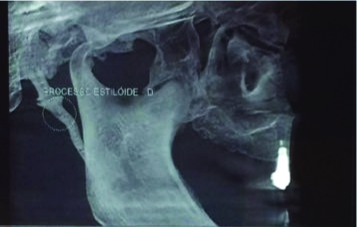
Computed tomography showed hyperdense bilateral areas in the styloid processes’ regions [Table/Fig-2].
Tomographic reconstruction suggestive of an elongated styloid process on the right side.
Thus, correlating clinical symptoms and imaging, the conclusive diagnosis of Eagle syndrome was established.
Due to the severity of symptoms reported by the patient, the treatment option was surgical excision of the styloid processes. The chosen access was the bilateral intraoral approach since it causes less postoperative morbidity and prevents the occurrence of visible scars.
The patient underwent general anaesthesia with nasotracheal intubation. With the patient’s mouth at the range of maximum opening, the region of the tonsillar pillar was palpated, indicating the location for incision with the electrocautery. The incision began lateral to the maxillary tuberosity, passing by the anterior border of the mandibular ramus, to the oblique line.
Tissue dissection was performed and the styloid processes were located. The tissue was dissected till the most proximal portion of the styloid processes. With a Kelly forceps the styloid processes were fractured and removed [Table/Fig-3,4] and then incisions were closed with simple continuous 4-0 vicryl sutures. The styloid process removed from the right side was about 4cm in length whereas left styloid process measured 3 cm [Table/Fig-5].
The distal part of right styloid process was exposed in the oral cavity before removal.
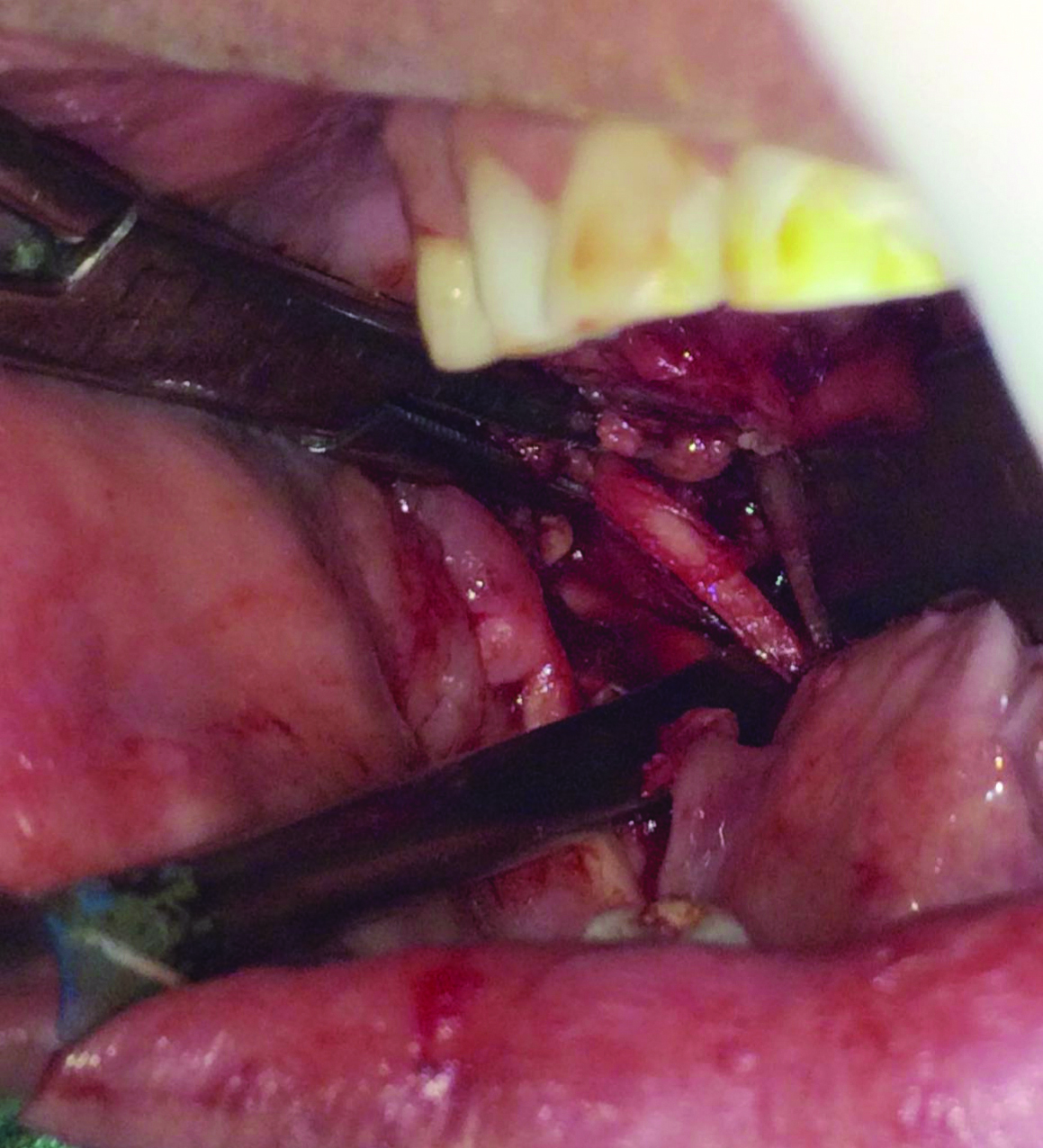
The distal part of left styloid process was exposed in the oral cavity before removal.

Left (above) and right (below) styloid processes.

Postoperative prescription included Cephalexin 500 mg every 6 hours for seven days, Cetroprofen 100 mg every 12 hours for three days, Dexamethasone 4 mg every 8 hours for three days (due to its antiinflammatory effects), Dipyrone 1g every 6 hours in case of pain. All medications were to be taken orally.
The patient was also instructed to rinse with 0.12% chlorhexidine mouthwash twice a day for seven days and to maintain proper oral hygiene. She was advised to have liquid/semisolid diet for the first week after the surgery and preferably avoid taking hot food for the first 3 days.
On the sixth postoperative day, the patient reported no pain when moving her neck. There was some pain in the operated areas while eating but patient did not report any paresthesia. Clinically, the surgical wound showed good signs of healing [Table/Fig-6].
Postoperative clinical appearance after 6 days.
On one month follow-up, the patient reported of not feeling any pain, but informed about paraesthesia in the right anterior portion of the tongue. The clinical image showed good healing but the position of the tongue suggested a lesion of the hypoglossal nerve [Table/Fig-7]. Citoneurim 5000 mcg once a day for 30 days was prescribed for the paraesthesia. Radiographically, the absence of the elongated styloid processes was evident [Table/Fig-8].
Clinical aspect of the patient after 30 days. The position of the tongue suggests a lesion of the hypoglossal nerve.

Panoramic radiograph six days after surgery.
On two and three months follow-up, the patient reported complete regression of pain but no improvement in tongue paraesthesia.
After two years of follow-up, the patient did not report painful symptoms, but paresthesia on the right side of the tongue still persisted [Table/Fig-9]. The radiographic examination did not present elongated styloid processes [Table/Fig-10].
Clinical aspect of the patient after 2 years.

Radiographic appearance after 2 years.
Informed consent was taken from the patient for publishing the case, including photos and radiographs.
Discussion
Eagle Syndrome is a rare condition caused by symptomatic elongation of the styloid process and/or calcification of the stylohyoid ligament [1] with higher incidence after 30 years [1,2]. The condition is more common in women [2] with a ratio of occurrence in females: males of 3:1 [3], the presented case was that of a female. Although a study by Ilgüy M et al., showed a higher frequency of the length of the ossified portion of the stylohyoid complex in females [3], another study by Ledesma-Montes C et al., showed no difference of length of the stylohyoid complex between genders [4].
In the case reported, the patient presented classic symptoms of Eagle syndrome, such as pain when swallowing, speaking and opening the mouth; foreign body sensation that could not be swallowed and pain in the temporomandibular joint region [5].
Eagle syndrome is diagnosed by radiography and physical examination. Pain during palpation of the tonsillar fossa could alert clinicians to this possible diagnosis [6]. A 17-year-old male reported odynophagia and a foreign body sensation in the throat after choking on a chicken wing. On the neck radiograph, was observed a 4.6-cm linear object in the vallecula suggested as a chicken bone due to the patient’s history. A nasopharyngeal laryngoscopy was performed but was unremarkable. Only after that, the palpation of the tonsillar fossa was performed, and the patient reported tenderness. On radiographic review, the right stylohyoid ligament was noted to be elongated and calcified and the patient was diagnosed with Eagle syndrome [6]. In the present case, Eagle syndrome was the main diagnostic hypothesis after physical and radiographic examination.
The symptomatic management of Eagle syndrome with conservative medical treatment, such as antiinflammatory medications, anticonvulsants, antipsychotics, or other analgesics is usually reserved for patients unable to undergo surgical procedure [1]. Surgical treatment presents remission of symptoms without the need for continuous drug use [4] even in patients with long-lasting, chronic pain disorders [7] and it is indicated for all patients due to it being the definitive treatment for this condition [2]. The option for the surgical treatment in this case was taken, considering the worsening of the symptoms reported by the patient and the definitive character of the intervention.
The surgical management of the Eagle syndrome may be accomplished by either an intraoral or extraoral approach [1,7,8]. Intraoral approach results in no external scar, can be accomplished in a relatively shorter time than the extraoral approach [1,9], with the possibility of being performed under local anaesthesia and faster postoperative recovery [9]. Hardin FM et al., reported the surgical treatment of 21 patients diagnosed with Eagle syndrome [9]. Twelve patients were treated by a transcervical approach; the time spent in the procedure was 103 minutes and 10 patients stayed in the hospital for at least one night. Nine patients were treated by transoral approach, with the median time of 74 minutes, and no patient needed to stay overnight in the hospital. Four of the 21 patients reported paraesthesia [9]. The study showed an advantage for the transoral approach in terms of surgical length and hospital internment. In the presented case, the intraoral approach for the styloid processes’ excision was performed under general anaesthesia.
However, the intraoral approach can be limited by poor exposure and lighting thus, increasing risk of injury to critical neurovascular structures within the parapharyngeal space [1,7]. That may be a possible explanation for the occurrence of paraesthesia on the right side of the tongue of the patient which persisted after two years of monitoring. The condition differs from those reported previously in which the elongated styloid process was also removed by intraoral approach; general anaesthesia and the paresthesia presented spontaneous resolution [8].
To minimise such complications, minimally invasive techniques have been presented as safe options that provide symptomatic improvement with little blood loss, decreased operative time, shorter postoperative length of stay and lower complication [1,8]. The transoral robotic surgery is one of those techniques. As it is performed via a transoral approach it does not lead to scar formation and can be done with a minimum incision for the introduction of the robotic arms. This technique permits excellent view and safe manipulation avoiding iatrogenic damage to neurovascular structures [10]. Robotic surgery could have avoided the hypoglossal nerve injury occurred in our patient, but the use of robotic surgery is not easily accessible in many hospitals and may increase the cost of the surgical procedure.
Conclusion(s)
The surgical treatment with intraoral approach provided a definitive treatment of Eagle syndrome in the presented case over a two years follow-up period. It was performed quickly, did not cause scarring and patient had a quick recovery and high satisfaction besides the hypoglossal nerve palsy. It can be considered as a potential treatment option because of its advantages over the extraoral approach.
[1]. Fitzpatrick IV TH, Lovin BD, Magister MJ, Waltonen JD, Browne JD, Sullivan CA, Surgical management of Eagle syndrome: A 17-year experience with open and transoral robotic styloidectomyAm J Otolaryngol 2020 41(2):10232410.1016/j.amjoto.2019.10232431767138 [Google Scholar] [CrossRef] [PubMed]
[2]. Demirtaş H, Kayan M, Koyuncuoğlu HR, Çelik AO, Kara M, Şengeze N, Eagle syndrome causing vascular compression with cervical rotation: Case reportPol J Radiol 2016 81:277-80.10.12659/PJR.89674127354882 [Google Scholar] [CrossRef] [PubMed]
[3]. Ilgüy M, Ilgüy D, Güler N, Bayirli G, Incidence of the type and calcification patterns in patients with elongated styloid processJ Int Med Res 2005 33(1):96-102.10.1177/14732300050330011015651721 [Google Scholar] [CrossRef] [PubMed]
[4]. Ledesma-Montes C, Hernández-Guerrero JC, Jiménez-Farfán MD, Length of the ossified stylohyoid complex and Eagle syndromeEur Arch Otorhinolaryngol 2018 275(8):2095-100.10.1007/s00405-018-5031-329948265 [Google Scholar] [CrossRef] [PubMed]
[5]. Kamal A, Nazir R, Usman M, Salam BU, Sana F, Eagle syndrome; radiological evaluation and managementJ Pak Med Assoc 2014 64(11):1315-17. [Google Scholar]
[6]. Cohn JE, Othman S, Sajadi-Ernazarova K, Eagle syndrome masquerading as a chicken boneInt J Emerg Med 2020 13(1):110.1186/s12245-020-0262-731931721 [Google Scholar] [CrossRef] [PubMed]
[7]. Czajka M, Szuta M, Zapała J, Janecka I, Assessment of surgical treatment of Eagle’s syndromeOtolaryngol Pol 2019 73(5):18-24.10.5604/01.3001.0013.153331701903 [Google Scholar] [CrossRef] [PubMed]
[8]. Terenzi V, Giovannetti F, Barbera G, Raponi I, Valentini V, Endoscopy-Assisted Intraoral Removal of Elongated Styloid Process: Mini-Invasive Surgical Treatment of Eagle SyndromeJ Craniofac Surg 2019 30(8):e775-76.10.1097/SCS.000000000000576731592840 [Google Scholar] [CrossRef] [PubMed]
[9]. Hardin FM, Xiao R, Burkey BB, Surgical management of patients with Eagle syndromeAm J Otolaryngol 2018 39(5):481-84.10.1016/j.amjoto.2018.05.00329764674 [Google Scholar] [CrossRef] [PubMed]
[10]. Montevecchi F, Caranti A, Cammaroto G, Meccariello G, Vicini C, Transoral Robotic Surgery (TORS) for Bilateral Eagle SyndromeORL J Otorhinolaryngol Relat Spec 2019 81(1):36-40.10.1159/00049373630537726 [Google Scholar] [CrossRef] [PubMed]