Introduction
The disease caused by the novel corona virus emerged in December, 2019 and became major public health challenge all over the world. Official nomenclature of the virus is SARS-Cov-2. It was confirmed by the WHO that the virus spreads from human-to-human transmission and on 31st January declared this COVID-19 outbreak as public healthcare emergency throughout world [1]. The period of incubation for COVID-19 is from 2 to 14 days according to the Center for Disease Control and Prevention (CDC). The disease includes the symptoms of fatigue, myalgia, fever, cough, dyspnoea and diarrhoea. The disease may get complicated into acute respiratory distress syndrome, arrhythmia and shock [1-3]. The SARS CoV-2 is highly communicable disease and became global health threat within weeks. As of till 10th June, 2020, there were 7,452,809 confirmed cases involving more than 200 countries and 418,919 deaths according to WHO all over the globe. In India and as of on 10th June, total confirmed cases were 278,476 and total number of deaths were 8138 [4]. At the same time, there is sudden rise in the number of conjunctivitis cases from mid-December in India which was sporadic in nature throughout this year [5]. Most of them were in severe form associated with flu-like symptoms and ipsilateral preauricular gland enlargement. Most of them were having positive travelling history. A 90% of cases were from the urban population [5].
This rise in cases of conjunctivitis draws attention towards the point, if the cases of COVID-19 are being under reported? Do administration and Health Department need to establish new guidelines regarding the patients of conjunctivitis attending ophthalmology clinics? Do we need to undergo laboratory investigations in isolated case of conjunctivitis without other symptoms of SARS-CoV-2 in such pandemic situation of COVID-19?
The aim of this review article was to share knowledge and experiences about COVID-19 and its correlation with conjunctivitis and associated risk to the ophthalmologists and healthcare workers all over the world and to make them aware of necessary preventive and safety measures to minimise the transmission of SARS-CoV-2 infection amongst them and the patients.
Literature Search
Relevant articles were identified by searches from PubMed (1957 to 2020) with the terms “SARS-CoV-2, viral conjunctivitis,” or“eye and corona virus”. Additional relevant articles were identified by cross-referencing Google Scholar, PMC, references from relevant articles, and articles from AAO and Eurotime reports were also included. Articles were selected after review of titles, abstracts and references. English language articles were reviewed. Articles and meta-analyses that provided evidence-based information about the viral conjunctivitis, presence of SARS-CoV-2 in tears and conjunctiva, risk of spreading of infection to an ophthalmologist and preventable measures were selected.
SARS-CoV-2 and Ophthalmologists
Possible mode of conjunctival transmission
Respiratory viral infections are the most common cause of acute illness and a topic of concern for the physicians across the globe. SARS-CoV-2 which causes disease named COVID by WHO became a major global threat since January, 2020 [1]. These viruses have high transmissibility, global distribution, mucosal sites of infection, and several overlapping symptoms. Generally infections with these viruses involve upper respiratory tract, it can reach to lower respiratory tract especially among the immunocompromised individuals or other co-morbidities. SARS-CoV-2 are typically spread by inhalation of virus containing aerosols expelled by infected individuals or by direct or indirect contact with virus contaminated fomites on environmental surfaces [5,6]. Epithelial layer of the human eye is an additional mucosal surface which is similarly exposed to infectious aerosols and contaminated fomites [7-9]. The routes of transmission of SARS other than respiratory droplets are through stools and urine. The WHO reported tears to be one of the body fluids and might transmit the SARS corona virus through them [10]. Inspite of these viruses which are generally considered respiratory pathogens are capable of causing ocular complications in infected individuals and may cause respiratory infection following ocular exposure.
The possible mechanism which permit the eye to serve as both a potential site of virus replication as well as a gateway to spread of virus to extraocular sites to establish a respiratory infection is through primarily by the nasolacrimal system, which acts as an anatomical bridge between ocular and respiratory tissues [11,12].
The lacrimal duct collects tear fluid from the ocular surface and transports it to the inferior meatus of the nose. This tear fluid facilitates the transport of virus from ocular surface to respiratory tract tissues, thus serving as a path for virus containing tear fluids exchange between ocular surface and respiratory tract [13,14].
Corona Virus and Conjunctivitis
Human Corona Viruses (HCoV) are enveloped, single-stranded RNA viruses, which (with the exception of SARS) generally cause mild upper respiratory tract infections in humans [15]. Two types of corona viruses were found which have circulated in the human population, (HCoV-229E and HCoV-OC43), and two more (HCoV-HKU1 and HCoV-NL63) were identified recently [15-17]. These virus isolates are highly transmissible and are responsible to cause common colds frequently in all ages [14]. Similar to other human respiratory coronaviruses, HCoV-NL63 typically causes both upper and lower respiratory tract infections [16,18-21]. An association between HCoV-NL63 infection and Kawasaki disease has been reported where a systemic vasculitis of childhood for which bilateral conjunctivitis is one criterion to diagnosis. However, a definitive association of HCoV-NL63 as the causative agent of this disease has not been established [20,22]. It is therefore not clear if the conjunctivitis as a presenting feature in HCoV-NL63-infected patients is due to the coronavirus itself or represents a manifestation of disease caused by secondary pathogen or any other disease.
The SARS-associated coronavirus, which was identified in 2003 for the first time, was known for virus causing pneumonia with rapid progression to severe disease and death in contrast to other human coronaviruses [23,24]. Mode of transmission was primarily via direct or indirect contact with mucous membranes of the eyes, nose, or mouth [23-25]. Lack of wearing Personal Protective Equipments (PPEs) lead to increased risk of transmission of SARS coronavirus infection through mucous membrane including eye. The HCWs without mouth barrier and eye protection are associated with an increased risk of transmission from infected patients, as seen during the 2003 SARS outbreak in Toronto [26]. SARS coronavirus was detected by Reverse Transcription-Polymerase Chain Reaction (RT-PCR) though ocular symptoms have not been reported following virus infection, in tear samples from three infected cases obtained from conjunctival swabs collected during the early phase of symptom onset (within nine days) [27]. However, SARS coronavirus could not be detected in tears and conjunctival scraping samples obtained from confirmed SARS patients, and eyes of confirmed patients with SARS coronavirus did not show ocular manifestations of disease following ophthalmic examination in several other studies [28,29]. More research is required to give better explanations’ if this discrepancy is due to false-negative results or the timing of sample collection [30]. Despite not very conclusive evidence of SARS coronavirus replication in ocular samples, these studies still show the eye as a potential portal of entry for this virus [31].
Ocular manifestation in SARS-CoV-2 predominantly seen is conjunctivitis including conjunctival hyperemia, chemosis, epiphora, and increased secretions [28,32]. Conjunctivitis being the first presenting symptom of COVID-19 is shown by some of the reports [11,12]. Conjunctival congestion has been documented in 0.8% of patients with laboratory confirmed COVID 19 from 30 hospitals across China [25].
Role of Renin-Angiotensin System in Conjunctivitis in SARS-CoV-2
The SARS-CoV-2 has a similar receptor binding sites as SARS-CoV and they infect host cells via the angiotensin converting enzyme-2 (ACE2) [33] Renin-Angiotensin System (RAS) has the endocrine role in blood pressure regulation. It also plays role in complicated autocrine functions within specific tissues and the human eye is having its own intraocular RAS. Angiotensin Converting Enzyme 2 (ACE 2) has been found in the aqueous humor [34]. There is no knowledge about its expression in more anterior tissues such as the conjunctiva or cornea. Further studies have to be conducted to establish the hypothesis of SARS-CoV-2 ocular infection through ACE2.
Evidence of SARS-CoV-2 Virus in Tears and Conjunctiva
Reverse Transcription (RT)-PCR: SARS coronavirus can be detected in tear samples by RT-PCR by obtaining conjunctival swabs collected during the early phase of symptom onset that is within nine days. There are several interpretations for the negative findings of SARS-CoV viral genetic material or viable virus in the tear secretion or conjunctival cells of patients with serologically confirmed SARS cases. The RT-PCR testing or viral culture is having high specificity but they lack in sensitivity [35]. So, false-negative results do not exclude the chances of presence of the virus in the given sample. One can increase the sensitivity by testing multiple specimens at different time intervals as there is possibility that the samples are not collected at the right time and the virus and its genetic material are present for a short period of the disease in the body fluids and specimens.
Also, the quality of the examined kit may alter the PCR results for SARS-CoV-2. Novel coronavirus’s characteristics, sampling location, sampling volume, transportation, and storage, as well as laboratory test conditions and personnel operation play major role in PCR results [28]. Single sample of tear swab and conjunctival scraping may not be sufficient and cannot totally exclude the presence of virus in the tear secretion, and it is clear that only on the basis of conjunctival swabs and conjunctival scrapings, we cannot confirm or exclude the diagnosis [28].
In Wu P et al., study, amongst 38 patients of COVID-19, 28 patients (73.7%) had positive findings for COVID-19 confirmed by RT-PCR from nasopharyngeal swabs, and amongst these two patients (5.2%) had positive findings for SARS-CoV-2 in their conjunctival specimens too. Total 31.6% patients presented with ocular manifestations included with conjunctivitis, conjunctival hyperemia, chemosis, epiphora, or increased secretions [32].
There are other diagnostic tests having more sensitivity than RT-PCR after one week of onset of symptoms but their reports in ocular tissue and tears are not available in the literature and may not be studied [Table/Fig-1] [36].
Diagnostic tests sensitivity in the days after symptom for SARS-CoV-2 [36].
| Diagnostic test | Days after symptoms onset |
|---|
| SARS CoV2 test | 1-7 | 8-14 | 15-39 |
| RNA by RT-PCR | 67% | 54% | 45% |
| Total antibody | 38% | 90% | 100% |
| IgM | 29% | 73% | 94% |
| IgG | 19% | 54% | 80% |
COVID-19: Risk to the Ophthalmologists and Patients
The spread of the virus is through small respiratory droplets produced by an infected person, also by touching the contaminated object with the virus and then touching to mouth, eyes or nose. There are reports suggested that the virus can lead to conjunctivitis and be transmitted by aerosol contact with the conjunctiva [37,38]. Therefore, if the patient visit the ophthalmologist for the treatment of conjunctivitis with other respiratory symptoms and positive travelling history to the areas with known outbreaks or contact with COVID-19 patient or suspected COVID-19, could be suspected of carrying the virus [39-41]. Though the reliability not known, few reports suggested that when no eye protection was worn, the virus could also possibly be transmitted by aerosol contact with conjunctiva [42-44].
As of on 30th March, 2020 more than 3000 healthcare workers in China were infected with COVID-19 and six of them died [6]. Keng JL, an ophthalmologist at Wuhan Central Hospital reported that in early January he suffered from COVID-19 from one of his asymptomatic glaucoma patient [40].
Ophthalmologists may thus be the first healthcare providers to evaluate patients potentially infected with COVID. Hence, the proximity between ophthalmologists and patients during the slit-lamp examination and most of the ophthalmic evaluation and treatment procedures (which are much within the range of aerosol transmission) may pose a direct risk [45]. An ophthalmic practice involves multiple procedures and investigations including slit-lamp biomicroscopy, tonometry, retina examination which needs pupillary dilatation which increases stay of a patient for a longer duration in the hospital and increases the risk of cross infection to other patients and to HCWs as well. This risk increases with asymptomatic and unsuspected patients with subclinical infections [46].
Action Plan for the Ophthalmic Set ups and Clinics
Though conjunctivitis is not one of the most common symptoms of COVID-19, it may be a first presenting symptoms or a patient reporting to eye clinic may have a subclinical infection with the virus. In context to this, ophthalmologists may be the first specialists to evaluate patients possibly infected. Three level hierarchy of control measures should be set up in all ophthalmic set ups at the level of administration, environmental and use of PPEs [47].
Role of Hospital Administration
Role of an administration must intend towards the reduction of the risk of exposure of uninfected people from the COVID-19 patients.
Measures to be taken should be intended toward reducing the number of patients attending clinics. Planning of elective work and surgeries with restrictions should be done.
Use of electronic media to send the information related to hospital strategies in the situation of pandemic, providing them phone numbers for taking prior appointments and postponing them [47,48].
Standard Operating Protocol (SOP)
All the hospital personnel should wear a mask on the face as the commonest mode of transmission is through droplets. Sign boards displaying the information related to hand hygiene and cough etiquette should be displayed. Sitting arrangements in the waiting area should maintain an ideal distancing criterion by WHO [10].
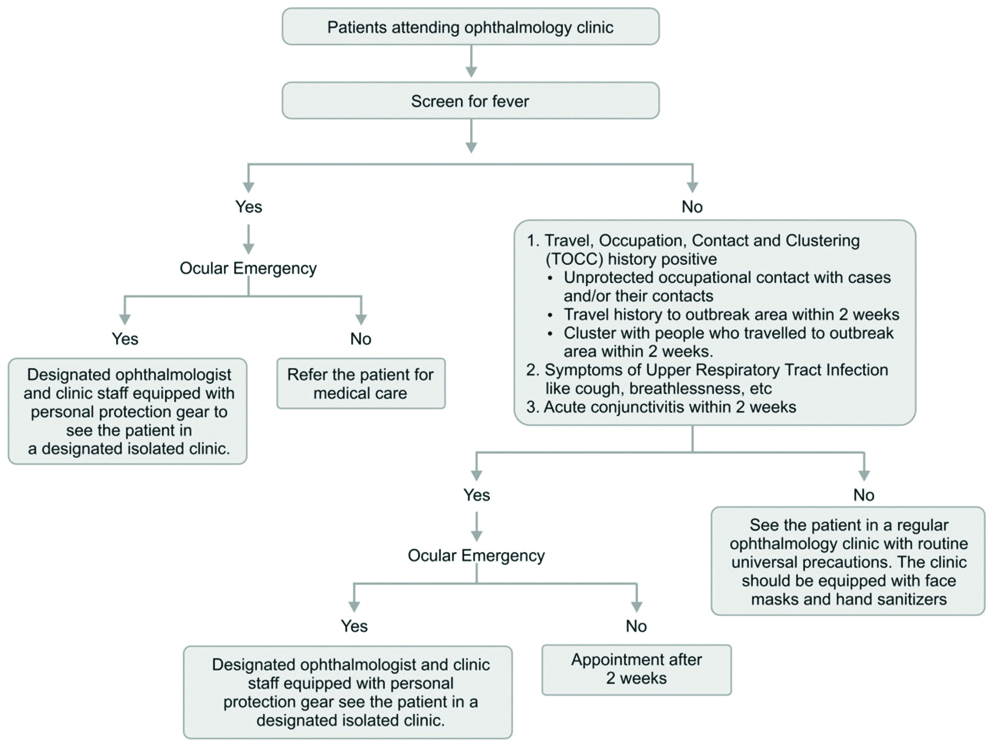
Patients with the fever should be identified before the entry in clinical area. For that, hospital should have a special screening station with the paramedical staff that can identify such cases with infrared thermometers. They can also screen the patients for COVID by asking history about illness, travelling or contact with such patients or persons. Any patient attaining these criteria requiring urgent ophthalmic evaluation should be dealt in separate room with separate instruments which are not shared in other consultation rooms. Patients with fever should be advised to seek medical advice and postpone the eye check up if not urgent. Patients with fever and ocular emergencies should be attended with proper PPEs on [48].
Deferring Aerosol Generating Procedures
Defering the procedures like noncontact tonometry as it is potential source of microaerosol [49]. The Goldmann applanation tonometer (not only the tip but the black housing) can touch the patient mask and mouth and can transmit the virus to the examiner, so care should be taken not to touch the applanator housing and sterilise it every time after its use.
Avoidance or postponement of the procedures like endoscopic dacryocystorhinostomy is advocated as it carries infectious risk to the surgeon and if unavoidable, then use of appropriate PPEs should be done [45]. General anaesthesia should be avoided as endotracheal intubation is of aerosol generating medium [45].
If the surgery under general anaesthesia is inevitable then (e.g., macula sparing retinal detachment, ocular trauma, etc.,), ophthalmologists should ensure if COVID-19 test is done for fever and TOCC (travel, occupation, contact and clustering) criteria should be ensured [46].
Those who tested positive and who tested negative but are clinically suspected, or cases in need of urgent intervention, making it infeasible to wait for the test result, the surgery would be performed in a separate operating theatre and all staff should wear isolation gowns, N95 respirators and protective eye glasses [Table/Fig-2] [47,48,50].
Suggested patient triage in an ophthalmology clinic [47,48,50].
Training and Staff Monitoring
All staff should be properly briefed to familiarise themselves with the steps of hand hygiene and donning and doffing of PPEs. All clinical staff should measure and report their own body temperatures before work and inform if symptoms like fever, chills, myalgia, sore throat, runny nose, cough, vomiting, diarrhoea or pneumonia to the hospital administration. Staff should be encouraged not to hide their travel histories [48,51].
Maintaining a Hospital Environment
The aim of environmental control is to prevent the spread and reduce the concentration of infectious droplet in the air. Waiting areas should be properly ventilated and be enhanced via opening of the fresh air dampers in the air handling equipment to get a fresh air at higher rate. Mobile High Efficiency Particulate Air (HEPA) units can be augmented in waiting areas where necessary [48,51,52].
As there is close proximity between ophthalmologists and patients during slit-lamp examination, it increases the risk of infection to the ophthalmologist, as droplets from a cough or sneeze can travel up to six feet [42]. Protective shields (made of plastic) can be installed on slit-lamps to lower the risk of transmission via droplets. These shields create barriers to droplets and they can be cleaned and disinfected after every OPD session [48].
Equipment’s in the clinics such as slit-lamps, indirect ophthalmoscopes, goniolenses, etc., and hospital environmental surfaces, those get touched frequently by healthcare workers and patients (such as doorknobs, chair handles, table tops, phones, and computer keyboards) should be disinfected according to CDC and AIOS guidelines [48,51].
Academic meetings should be conducted by using video conferencing and using apps like Zoom and Google Meet via personal mobile devices to avoid staff and student gatherings. Appropriate distancing between the two staffs on working stations, food courts and canteens should be practiced. Telemedicine can be practiced in certain cases as in new government resolution in epidemic except for patient meeting a COVID-19 criterion especially in minor complaints, medicine refilling and conjunctivitis without other symptoms of COVID-19. It can reduce the number of OPD patients [48].
Personal Protective Equipment (PPE)
Use of PPEs by ophthalmologists is always a big controversial topic. But recent reports of deaths of ophthalmologist and otolaryngologist in China and Italy, with new environmental virus contamination data and raised awareness of asymptomatic and subclinical spread of infections propel to protect mouth, nose, and eye. Setting of SOP in hospitals and maintaining a hospital environment and hygiene reduce the risk of exposure to SARS-CoV-2 but do not eliminate the risk of getting exposed to the virus as in treatment rooms where aerosol generating procedures are performed or isolation rooms where COVID-19 patients are kept [40,48,51].
The use of PPEs in these situations reduces the risk of exposure of healthcare workers to infectious droplets of COVID-19 disease. Protection including N95 masks for all physically close ophthalmic procedures and universal precautions for all patients should be practiced.
Whenever attending higher risk patients, ophthalmologist should take extra precautions and wear full PPEs including isolation gown, gloves, cap, eye protection, and N95 mask or respirator. Hand hygiene is of utmost importance and should be practised using the WHO formula alcohol hand rub or hand washing after examining every patient. If gloves need to be worn, they should be removed followed by hand hygiene between the cases [10,48,50,51].
While Attending Conjunctivitis Patients in Eye OPD
Though every patient in the current scenario can be a potential source of COVID-19, patients with conjunctivitis should be treated with greater risk, as the possibility of conjunctivitis being a presenting symptom of COVID-19 and second, the probable risk of transmission from tears from these patients [13,14]. Proper triage should be given to every conjunctivitis patient. Even if there is no fever, treat the patient as COVID suspect and examine with wearing at least N95 mask, protective eyewear and gloves if not full PPEs, with minimal slit-lamp examination with slit-lamp barrier. If patient comes with fever and upper respiratory tract infection then after giving proper treatment refer to COVID center. Emergency follow-up can be done on tele medicine and if symptomatically better then can continue the same treatment and ask to re-visit after two, weeks and if systemic symptoms of respiratory tract infections are worsening then should be referred to physician or COVID center. All the touched surfaces and slit-lamp should be cleaned with >70% alcohol [40,48,50].
Conclusion(s)
Corona virus can be transmitted through eyes and viral conjunctivitis may be one of the presenting symptoms of COVID-19, possibility of transmission by aerosol is yet to be confirmed. In context to this and close proximity of an ophthalmologist with the patient and the nature of work, standard infection protection measures should be followed by every ophthalmologist. There are anecdotal nature of reviews and literature regarding SARS-CoV-2 transmission through ocular tissue. To date, isolating the viral genomes from tears and conjunctiva was done only by RT-PCR which has high specificity but low sensitivity. As the current epidemic continues, more research on the relationship between human CoVs and the eye should be done with other modalities of more sensitive tests. This will not only help to guide infection control measures but can also provide insights on the feasibility of using ocular tissue or even tears as a medium of diagnosis. Emergence of more number of conjunctivitis cases should draw attention of health care administration and provide special guidelines for these patients as they may be COVID-19 patients.
[1]. Khan S, Siddique R, Ali A, Xue M, Nabi G, Novel coronavirus, poor quarantine, and the risk of pandemicJ Hosp Infect 2020 104(4):449-50.10.1016/j.jhin.2020.02.00232057788 [Google Scholar] [CrossRef] [PubMed]
[2]. Coronavirus (COVID-19). Available from: https://www.cdc.gov/coronavirus/2019-ncov/index.html. [Last accessed on 2020 Mar 16] [Google Scholar]
[3]. Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumoniaN Engl J Med 2020 382(13):1199-207.10.1056/NEJMoa200131631995857 [Google Scholar] [CrossRef] [PubMed]
[4]. Report on the basis of information published by WHO daily situation report, Ministry of Health Family Welfare mohfw.gov.in on 8 April 2020 at 9 am [Google Scholar]
[5]. Rao S, Conjunctivitis could also be a symptom of COVID 19, Says doctorhttps://timesofindia.indiatimes.com/toireporter/author- -R-479212689.cms [Google Scholar]
[6]. Hayden FG, Ison MG, Respiratory viral infection. In Dale DC, Federman DD. (ed)ACP Medicine 2006 2:01-17. [Google Scholar]
[7]. Belser JA, Maines TR, Tumpey TM, Katz JM, Influenza A virus transmission: Contributing factors and clinical implicationsExpert Rev Mol 2010 12:e3910.1017/S146239941000170521144091 [Google Scholar] [CrossRef] [PubMed]
[8]. Kumlin U, Olofsson S, Dimock K, Arnberg N, Sialic acid tissue distribution and influenza virus tropismInfluenza Other Respir Viruses 2008 2(5):147-54.10.1111/j.1750-2659.2008.00051.x19453419 [Google Scholar] [CrossRef] [PubMed]
[9]. Paulsen F, Functional anatomy and immunological interactions of ocular surface and adnexaDevOphthalmol 2008 41:21-35.10.1159/00013106818453759 [Google Scholar] [CrossRef] [PubMed]
[10]. What we know about transmission of the Ebola virus among humans. World Health Organisation. Media Centre. Ebola situation assessment. 6 October 2014 [Google Scholar]
[11]. Holland EJ, Mannis MJ, Lee WB, Ocular Surface Disease: Cornea, Conjunctiva and Tear Film 2013 Elsevier Inc.:452https://doi.org/10.1016/B978-1-4557-2876-3.00055-910.1016/B978-1-4557-2876-3.00055-9 [Google Scholar] [CrossRef]
[12]. Knop E, Knop N, Anatomy and immunology of the ocular surfaceChemImmunol Allergy 2007 92:36-49.10.1159/00009925217264481 [Google Scholar] [CrossRef] [PubMed]
[13]. Olofsson S, Kumlin U, Dimock K, Arnberg N, Avian influenza and sialic acid receptors: More than meets the eye?Lancet Infect Dis 2005 5(3):184-88.10.1016/S1473-3099(05)70026-8 [Google Scholar] [CrossRef]
[14]. Belser JA, Gustin KG, Maines TR, Pantin-Jackwood M, Katz JM, Tumpey TM, Influenza virus respiratory infection and transmission following ocular inoculation in ferretsJournal of Virology 2014 88(17):9647-54.10.1128/JVI.01067-1424920819 [Google Scholar] [CrossRef] [PubMed]
[15]. VanderHoek L, Human coronaviruses: What do they cause?AntivirTher 2007 12:651-58. [Google Scholar]
[16]. Van der Hoek L, Pyrc K, Jebbink MF, Vermeulen-Oost W, Berkhout RJ, Wolthers KC, Identification of a new human coronavirusNat Med 2004 10(4):368-73.10.1038/nm102415034574 [Google Scholar] [CrossRef] [PubMed]
[17]. Woo PC, Lau SK, Chu CM, Chan KH, Tsoi HW, Huang Y, Characterization and complete genome sequence of a novel coronavirus, coronavirus HKU1, from patients with pneumoniaJ Virol 2005 79(2):884-95.10.1128/JVI.79.2.884-895.200515613317 [Google Scholar] [CrossRef] [PubMed]
[18]. Isaacs D, Flowers D, Clarke JR, Epidemiology of coronavirus respiratory infectionsArch Dis Child 1983 58(7):500-03.10.1136/adc.58.7.5006307189 [Google Scholar] [CrossRef] [PubMed]
[19]. Vabret A, Mourez T, Dina J, van der Hoek L, Gouarin S, Petitjean J, Human coronavirus NL63, FranceEmergInfect Dis 2005 11(8):1225-29.10.3201/eid1108.05011016102311 [Google Scholar] [CrossRef] [PubMed]
[20]. Fielding BC, Human coronavirus NL63: A clinically important virus?Future Microbiol 2011 6(2):153-59.10.2217/fmb.10.16621366416 [Google Scholar] [CrossRef] [PubMed]
[21]. Fouchier RA, Hartwig NG, Bestebroer TM, Niemeyer B, de Jong JC, Simon JH, A previously undescribed coronavirus associated with respiratory disease in humansProcNatlAcadSci USA 2004 101(16):6212-16.10.1073/pnas.040076210115073334 [Google Scholar] [CrossRef] [PubMed]
[22]. Esper F, Shapiro ED, Weibel C, Ferguson D, Landry ML, Kahn JS, Association between a novel human coronavirus and Kawasaki diseaseJ Infect Dis 2005 191(4):499-502.10.1086/42829115655771 [Google Scholar] [CrossRef] [PubMed]
[23]. Peiris JS, Yuen KY, Osterhaus AD, Stohr K, The severe acute respiratory syndromeN Engl J Med 2003 349(25):2431-41.10.1056/NEJMra03249814681510 [Google Scholar] [CrossRef] [PubMed]
[24]. Drosten C, Gunther S, Preiser W, van der Werf S, Brodt HR, Becker S, Identification of a novel coronavirus in patients with severe acute respiratory syndromeN Engl J Med 2003 348(10):1967-76.10.1056/NEJMoa03074712690091 [Google Scholar] [CrossRef] [PubMed]
[25]. Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive studyLancet (London, England) 2020 395(5):507-13.10.1016/S0140-6736(20)30211-7 [Google Scholar] [CrossRef]
[26]. Raboud J, Shigayeva A, McGeer A, Bontovics E, Chapman M, Gravel D, Risk factors for SARS transmission from patients requiring intubation: A multicentre investigation in Toronto, CanadaPLoS One 2010 5:e1071710.1371/journal.pone.001071720502660 [Google Scholar] [CrossRef] [PubMed]
[27]. Loon SC, Teoh SC, Oon LL, Se-Thoe SY, Ling AE, Leo YS, Leong HN, The severe acute respiratory syndrome coronavirus in tearsBr J Ophthalmol 2004 88(7):861-63.10.1136/bjo.2003.03593115205225 [Google Scholar] [CrossRef] [PubMed]
[28]. Chan WM, Yuen KSC, Fan DSP, Lam DSC, Chan PKS, Sung JJY, Tears and conjunctival scrapings for coronavirus in patients with SARSBr J Ophthalmol 2004 88(7):968-69.10.1136/bjo.2003.03946115205249 [Google Scholar] [CrossRef] [PubMed]
[29]. Yuen KS, Chan WM, Fan DS, Chong KK, Sung JJ, Lam DS, Ocular screening in severe acute respiratory syndromeAm J Ophthalmol 2004 137(4):773-74.10.1016/S0002-9394(03)01148-6 [Google Scholar] [CrossRef]
[30]. Bonn D, SARS virus in tears?Lancet Infect Dis 2004 4:48010.1016/S1473-3099(04)01093-X [Google Scholar] [CrossRef]
[31]. Tong T, Lai TS, The severe acute respiratory syndrome coronavirus in tearsBr J Ophthalmol 2005 8(3):39210.1136/bjo.2004.05413015722333 [Google Scholar] [CrossRef] [PubMed]
[32]. Wu P, Duan F, Luo C, Liu Q, Qu X, Liang L, Characteristics of ocular findings of patients with Coronavirus Disease 2019 (COVID-19) in Hubei Province, ChinaJAMA Ophthalmol 2020 138(5):575-78.10.1001/jamaophthalmol.2020.129132232433 [Google Scholar] [CrossRef] [PubMed]
[33]. Wan Y, Shang J, Graham R, Baric RS, Li F, Receptor recognition by novel coronavirus from Wuhan: An analysis based on decade-long structural studies of SARSJ Virol 2020 94(7):e.00127-20.10.1128/JVI.00127-20 [Google Scholar] [CrossRef]
[34]. Holappa M, Vapaatalo H, Vaajanen A, Many faces of renin-angiotensin system- Focus on eyeOpen Ophthalmol J 2017 11(1):122-42.10.2174/187436410171101012228761566 [Google Scholar] [CrossRef] [PubMed]
[35]. Peiris JS, Lai ST, Poon LL, Guan Y, Yam LYC, Lim W, Coronavirus as a possible cause of severe acute respiratory syndromeLancet 2003 361:1319-25.10.1016/S0140-6736(03)13077-2 [Google Scholar] [CrossRef]
[36]. Zhao J, Yuan Q, Wang H, Liu W, Liao X, Su Y, Antibody responses to SARS-CoV-2 in patients of novel corona virus disease 2019Clin Infect Dis 2020 Mar 28 10.1093/cid/ciaa34432221519 [Google Scholar] [CrossRef] [PubMed]
[37]. Seah I, Su X, Lingam G, Revisiting the dangers of the coronavirus in the ophthalmology practiceEye (Lond) 2020 34:1155-57.10.1038/s41433-020-0790-732029919 [Google Scholar] [CrossRef] [PubMed]
[38]. Yu Jun IS, Anderson DE, Zheng Kang AE, Wang LF, Rao P, Young BE, Assessing viral shedding and infectivity of tears in coronavirus disease 2019 (COVID-19) PatientsOphthalmology 2020 127(7):977-79.10.1016/j.ophtha.2020.03.02632291098 [Google Scholar] [CrossRef] [PubMed]
[39]. WHO Director-General’s remarks at the media briefing on COVID-2019 outbreak on 14 February 2020.(2020) World Health Organization. https://www.who.int/dg/speeches/detail/whodirector-general-s-remarks-at-the-media-briefing-on-covid-2019- outbreak-on-14-february-2020. Accessed 15 Feb 2020 [Google Scholar]
[40]. Keng JL, Coronavirus kills Chinese whistle blower ophthalmologistAmerican Academy of Ophthalmology 15 Feb. 2020 https://www.aao.org/ headline/coronavirus-kills-chinese-whistleblower-ophthalmol [Google Scholar]
[41]. Chang D, Xu H, Rebaza A, Sharma L, Dela Cruz CS, Protecting health-care workers from subclinical coronavirus infectionLancet Respir Med 2020 8(3):e1310.1016/S2213-2600(20)30066-7 [Google Scholar] [CrossRef]
[42]. Zhou Y, Zeng Y, Tong Y, Chen C, Ophthalmologic evidence against the interpersonal transmission of 2019 novel coronavirus through conjunctivamedRxiv 12 Feb 2020 DOI: 10.1101/2020.02.11.20021956. https://doi.org/10.1101/2020.02.11.2002195610.1101/2020.02.11.20021956 [Google Scholar] [CrossRef]
[43]. Lu CW, Liu XF, Jia ZF, 2019-nCoV transmission through the ocular surface must not be ignoredLancet 2020 395(10224):e3910.1016/S0140-6736(20)30313-5 [Google Scholar] [CrossRef]
[44]. Alert: Important coronavirus context for ophthalmologists. American Academy of Ophthalmology. 2020. https://www.aao.org/ headline/alert-important-coronavirus-context. Accessed 18 Feb 2020 [Google Scholar]
[45]. Tran K, Cimon K, Severn M, Pessoa-Silva CL, Conly J, Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: A systematic reviewPLoS One 2012 7(4):e3579710.1371/journal.pone.003579722563403 [Google Scholar] [CrossRef] [PubMed]
[46]. CDC Tests for COVID-19. Centers for Disease Control and Prevention. 2020. https://www.cdc.gov/coronavirus/2019-ncov/about/ testing.html. Accessed 16 Feb 2020 [Google Scholar]
[47]. Lai THT, Tang EWH, Chau SKY, Fung KSC, Li KKW, Stepping up infection control measures in ophthalmology during the novel coronavirus outbreak: An experience from Hong KongGraefes Arch Clin Exp Ophthalmol 2020 doi: 10.1007/ s00417-020-04641-8 [Google Scholar]
[48]. AIOS Operational guidelines for ophthalmic practice during COVID 19 outbreak.www.aios.org/article 212-covid19-php [Google Scholar]
[49]. Britt JM, Clifton BC, Barnebey HS, Mills RP, Microaerosol formation in noncontact ‘air-puff’ tonometryArch Ophthalmol 1991 109(2):225-28.10.1001/archopht.1991.010800200710461993032 [Google Scholar] [CrossRef] [PubMed]
[50]. Shetty R, D’souza S, Lalgudi VG, All eyes on Coronavirus- What do we need to know as ophthalmologistsIndian Journal of Ophthalmology 2020 68(4):683-87.10.4103/ijo.IJO_516_2032174565 [Google Scholar] [CrossRef] [PubMed]
[51]. How Flu Spreads. (2020) Centers for Disease Control and Prevention. https://www.cdc.gov/flu/about/disease/spread.htm. Accessed 15 Feb 2020 [Google Scholar]
[52]. Christopherson DA, Yao WC, Lu M, Vijayakumar R, Sedaghat AR, High-efficiency particulate air (HEPA) filters in the era of COVID-19: Function and efficacyOtolaryngology- Head and Neck Surgery 2020 https://doi.org/10.1177/019459982094183810.1177/019459982094183832662746 [Google Scholar] [CrossRef] [PubMed]