Solitary Cysticercosis of Temporalis Muscle: A Rare and Challenging Diagnosis
Sweta Singh1, Uday Shanker Singh2
1 Senior Resident, Department of Microbiology, Sanjay Gandhi Post Graduate Institute of Medical Sciences (SGPGIMS), Lucknow, Uttar Pradesh, India.
2 Intervention Radiologist, Department of Radiodiagnosis, Advanced Diagnostic Centre, Lucknow, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sweta Singh, Senior Resident, Department of Microbiology, Sanjay Gandhi Post Graduate Institute of Medical Sciences (SGPGIMS), Lucknow, Uttar Pradesh, India.
E-mail: swetasinghkarn@gmail.com
Taeniasis is an endemic parasitic infection of developing countries, including India. It is caused by pork (Taenia solium), beef (Taenia saginata), and Asian (Taenia asiatica) tapeworms and the route of transmission is faeco-oral. It usually occurs due to ingestion of uncooked green leafy vegetables, undercooked meat or unsafe drinking water contaminated with faeces. The mode of presentation can be severe in the form of Neurocysticercosis (brain) or Solitary Muscular Cysticercosis. Neurocysticercosis can prove to be fatal and life-threatening condition in the form of seizures and focal neurological signs. Diagnosis of cysticercosis is usually based on direct stool examination for eggs on three consecutive days or proglottids of the tapeworm, serological tests such as Enzyme Linked Immunosorbent Assay (ELISA) and radiological imaging for confirmation. Here, a rare and very interesting case of cysticercosis was reported in temporalis muscle in a young female. The patient presented with only a solitary swelling in preauricular region. Both radiological and microbiological investigations played a very vital role in the diagnosis and the patient was finally diagnosed as a case of muscular cysticercosis. She was started on conservative treatment with albendazole and steroids for two weeks. Repeat radiological scans showed improvement in her swelling and complete resolution in about a month. Cysticercosis of temporalis muscle is in itself a very rare event and there are only a few reported cases in literature. The present case was also unique in terms of localisation of the cyst as it was inside the superficial fibers and fascia of the muscle and not intramuscularly.
Albendazole, Neurocysticercosis, Seizures, Taenia solium, Taeniasis, Tapeworm
Case Report
A 31-year-old female presented to the outpatient department of the hospital with a solitary swelling in preauricular region for the last two months. The patient was a daily wage worker working at a construction site and belonged to the lower socio-economic class. The pain was aggravated on opening the mouth and while chewing the food. She also complained of restricted mouth opening subsequent to the swelling from last one month. The patient also complained of mild epigastric discomfort and nausea from last two weeks. She had no previous history of any surgeries or long-term hospital stay and also no comorbidities like hypertension, diabetes, etc. Dietary history of the patient revealed frequent consumption of uncooked green leafy vegetables from the field near her house. This field was also subject to open defecation by the people nearby. Drinking water came from a small pond not very far from her house. She was a nonvegetarian and used to eat pork or meat at least twice in a month. There was no history of blurring of vision or jaw claudication. Local examination of the area revealed a solitary diffuse swelling with blended, imperceptible margins in the preauricular region over the right temporal area and extended over the right temple. The swelling was appreciated more on palpation than inspection. On palpation, the swelling was pitting in nature, slightly tender, and was fixed to the underlying subcutaneous tissue structures. Differential diagnoses consisted of lipoma, fibroma, haemangioma, and mucocele. Fundus examination revealed a normal optic disc with no other ophthalmic deficit. Neurological examination was also normal with no motor or sensory deficits. The patient was advised Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) namely, ibugesic plus 400 mg for five days for pain relief. However, no relief from such medication was reported.
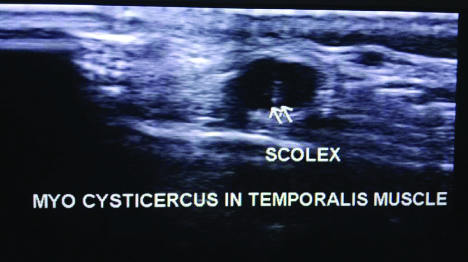
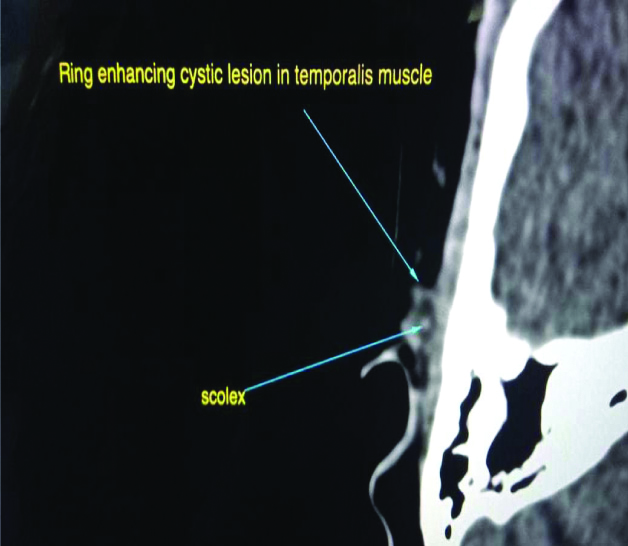
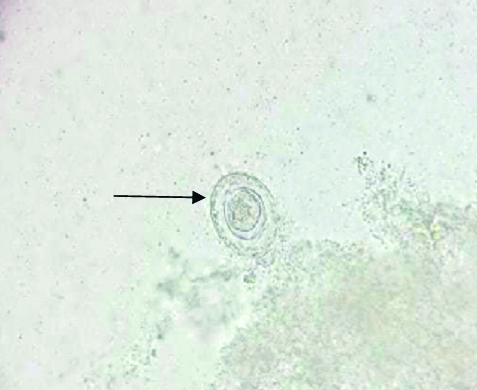
Further work-up and evaluation was planned with blood investigations and radiological imaging. Her blood reports were normal and did not reveal anything significant. High-resolution Ultrasonography (USG) revealed a well-defined, oval-shaped anechoic (cystic) lesion around 0.7×1×0.4 mm in relation to superficial fibers and fascia of right temporalis muscle [Table/Fig-1]. The Computed Tomography (CT) scan of the area revealed peripherally enhancing small cystic lesion adjacent to the right temporalis fascia [Table/Fig-2,3]. The radiological features on both high-resolution USG and CT scan were suggestive of cysticercosis involving the fascia of right temporalis muscle. The patient was referred to the Microbiology Laboratory for further confirmation of the diagnosis. Stool routine microscopy revealed eggs of Taenia spp. measuring 30-35 um in diameter, with radial striations and hooklets inside it [Table/Fig-4]. Serological test for Cysticercosis IgG by ELISA kit (California) was positive. No evidence of disseminated or intracranial cysticercosis was found. The patient was finally diagnosed as a case of muscular cysticercosis and was started on conservative treatment with 15 mg/kg/day of albendazole for 14 days, along with oral methyl prednisolone 2 mg/kg/day for first four days was given which was later tapered down over 14 days. Patient was also advised to have only properly cooked food, clean drinking water and avoid raw or undercooked meat. Follow-up was done with repeat USG scan after a month which showed complete resolution of the cysticercosis lesion and its symptoms.
High-resolution ultrasonography showing a well-defined, oval-shaped anechoic (cystic) lesion around 0.7×1×0.4 mm in relation to superficial fibers and fascia of right temporalis muscle Arrow indicates echogenic scolex of cysticercus.
The CT scan of the temporal region reveals peripherally enhancing small cystic lesion adjacent to the right temporalis fascia. Arrow in the figure indicates a central scolex appearing as a tiny dot.

The CT scan (closer and detailed view) of the area reveals peripherally enhancing small cystic lesion adjacent to the right temporalis fascia. Arrow in the figure indicates a central scolex appearing as a tiny dot.
Unstained wet mount of stool showing eggs of Taenia (marked with arrow) with hooklets.
Discussion
Taeniasis is a tapeworm infection, generally caused by pork (Taenia solium), beef (Taenia saginata), and Asian (Taenia asiatica) tapeworms found in undercooked meat [1]. It is usually endemic in developing countries such as India and South-East Asia [1,2]. Consumption of raw or undercooked fish, including contaminated sushi, can also result in infection from the fish tapeworm (Diphyllobothrium latum). Tapeworms are flatworms (cestodes) with multiple body segments and a head called a ‘scolex’ that attaches to the intestinal wall. They can become quite large, reaching 4 to 8 meters long. Tapeworms attached to the intestinal wall produce eggs that are excreted in faeces. After ingestion by animals, the eggs hatch and the larvae emerge. They may take up residence in the intestine, but can sometimes move to other tissues, especially muscle or brain tissue. When T. solium larvae form cysts in tissue, the condition is called cysticercosis. This occurs through ingestion of eggs via the faeco-oral route, not through consumption of undercooked meat. It can develop in the muscles, eye (ophthalmic cysticercosis), or brain (neurocysticercosis) [3]. Four different stages of muscular cysticercosis have been reported [4]. The first stage is cysticercus cyst with an inflammatory mass around it, as a result of the death of the larva. The second stage is an irregular cyst with very minimal fluid on one side, indicating a leakage of fluid. The eccentric echogenic protrusion from the wall due to the scolex is not seen within the cyst. The third stage consists of an eccentrically situated cysticercus cyst within the muscle surrounded by a large irregular collection of exudative fluid. This appearance is similar to an intramuscular abscess. The fourth stage of sonographic appearance is that of calcified cysticercosis [4]. In this case report, the high-resolution USG appearance is similar to the fourth stage type as an anechoic area in the right temporal muscle is seen which is clinically very similar to intramuscular abscess causing diagnostic dilemma.
Neurocysticercosis is a severe, life-threatening condition and often results in headache, focal signs, seizures and epilepsy. Cysts in the ventricular and subarachnoid area present as Space Occupying Lesions (SOL) with or without hydrocephalus and with headache and intracranial hypertension as the most frequently associated symptoms. On the other hand, muscular cysticercosis is milder and may altogether be asymptomatic in most cases [4,5]. Clinical features of cysticercosis ranges from being asymptomatic to mild gastrointestinal symptoms such as epigastric discomfort, nausea, diarrhea, flatulence, or hunger pains [5,6].
Diagnosis of cysticercosis is usually based on direct stool examination for eggs or proglottids of the tapeworm, serological tests such as ELISA and radiological imaging for confirmation. The serological assays include indirect haemagglutination, immunoelectrophoresis, double immunodiffusion, precipitation, indirect immunofluorescence, and skin reaction. The serological test employed should not only be high in sensitivity and specificity but should also be able to differentiate between living and dead parsites. It should also aid in patient follow-up with quantitation of parasite load [7,8]. The ELISA is a quite simple technique, is sensitive, quantitative and can process many samples at the same time, thus it is the most frequently used antibody detection assay [8]. The sensitivity of serum ELISA varies from 50% to 87% with a specificity of 63%-95% [7-9].
In the present case, there was a solitary lesion in the preauricular region involving only the superficial fibers and fascia of temporalis muscle which is extremely rare and caused diagnostic dilemma to the clinician. Literature search of muscular cysticercosis cases involving temporalis muscle has been enlisted below in [Table/Fig-5] [6-9]. A rare case of cysticercosis of upper lip has also been reported by Deshmukh A et al., [10].
Cases of cysticercosis of temporalis muscle [6-9].
| Author/year of study | No. of reported cases |
|---|
| Sethi PK et al., 2007 [6] | 1 |
| Kumar V et al., 2011 [7] | 1 |
| Singh S et al., 2013 [8] | 2 |
| Giri KY et al., 2016 [9] | 1 |
| Present case, 2020 | 1 |
The various treatment options currently available to treat cysticercosis include: 1) larvicidal agents; 2) corticosteroids or immunosuppressants to counteract the inflammation; 3) antiseizure medications; 4) surgical removal of cysts [11]. In this case, conservative management in the patient was done with albendazole and prednisolone to stop inflammatory reaction. Cysticidal drugs may be associated with severe adverse reactions, like local tissue swelling and generalised anaphylactic reaction as a result of massive release of antigens. These reactions are taken care of by instituting corticosteroids in the treatment regimen [11]. Prognosis usually depends on the site and number of cysts. It is usually favourable in the maxillofacial region with no recurrence. Grave consequences are seen in the cerebral, ocular, or cardiac sites [9-11].
Conclusion(s)
Cysticercosis of temporalis muscle is in itself a rare event and if seen is usually present intramuscularly. On the contrary in the present case, the cysts were localised inside the superficial fibers and fascia of the muscle. This is an extremely rare finding. Both radiological and microbiological work-up should go hand in hand to get excellent results in patient’s diagnosis, treatment as well as follow-up.
Author’s contribution: SS performed literature search, data analysis, and first draft of the manuscript and figures. USS contributed with the clinical radiograph images of the patient, literature search and final draft of the manuscript.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jul 10, 2020
Manual Googling: Aug 04, 2020
iThenticate Software: Sep 23, 2020 (4%)
[1]. Akhtar MN, Agarwal S, Disseminated cysticercosis incidentally diagnosed in a patient of low backache: A case report and concise review of literatureAsian Pac J Trop Med 2012 5(7):582-86.10.1016/S1995-7645(12)60103-5 [Google Scholar] [CrossRef]
[2]. Park SY, Kong MH, Kim JH, Song KY, Disseminated cysticercosisJ Korean Neurosurg Soc 2011 9:190-93.10.3340/jkns.2011.49.3.19021556243 [Google Scholar] [CrossRef] [PubMed]
[3]. Rao SC, Sharma H, Vinay KN, Vidya KC, Oral cysticercosis a case reportInt J Clin Dent Sci 2011 2(4):36-39. [Google Scholar]
[4]. Vijayaraghavan SB, Sonographic appearances in cysticercosisJ Ultrasound Med 2007 23:423-27.10.7863/jum.2004.23.3.42315055791 [Google Scholar] [CrossRef] [PubMed]
[5]. Sidhu R, Nada R, Palt A, Mohan H, Suri S, Maxillofacial cysticercosis: Uncommon appearance of a common diseaseJ Ultrasound Med 2002 21(2):199-202.10.7863/jum.2002.21.2.19911833875 [Google Scholar] [PubMed] [PubMed]
[6]. Sethi PK, Sethi NK, Torgovnick J, Arsura E, Cysticercosis of temporalis muscle: An unusual cause of temporal headaches. A case reportJ Headache and Pain 2007 8(5):315-16.0.1007/s10194-007-0410-y17955174 [Google Scholar] [CrossRef] [PubMed]
[7]. Kumar V, Gulati A, Mehra B, Cysticercosis of the temporalis muscle causing temporal headache in a pregnant womanInt J Gynecology and Obstetrics 2011 114(1):7910.1016/j.ijgo.2011.01.02221529806 [Google Scholar] [CrossRef] [PubMed]
[8]. Singh S, Sreenivasan V, Garg K, Wazir ND, Rajput JS, Virk PS, Cysticercosis involving muscle of mastication: A review and report of two casesCase Rep Dent 2013 2013:81412610.1155/2013/81412624396612 [Google Scholar] [CrossRef] [PubMed]
[9]. Giri KY, Alam S, Dandriyal R, Natu SS, Solitary cysticercosis of the temporalis muscle: Report of a rare caseJ Maxillofac Oral Surg 2016 15(Suppl 2):S240-44.10.1007/s12663-015-0754-927408444 [Google Scholar] [CrossRef] [PubMed]
[10]. Deshmukh A, Avadhani A, Tupkari JV, Sardar M, Cysticercosis of the upper lipJ Oral Maxillofac Pathol 2011 15(2):219-22.10.4103/0973-029X.8450922529585 [Google Scholar] [CrossRef] [PubMed]
[11]. Nash TE, Human case management and treatment of cysticercosisActa Trop 2003 87:61-69.10.1016/S0001-706X(03)00056-1 [Google Scholar] [CrossRef]