Bilateral Ovarian Mature Cystic Teratoma- A Rare Case Presentation
Kafil Akhtar1, Mohd Talha2, Saquib Alam3, Zehra Mohsin4
1 Professor, Department of Pathology, JNMC, AMU, Aligarh, Uttar Pradesh, India.
2 Resident, Department of Pathology, JNMC, AMU, Aligarh, Uttar Pradesh, India.
3 Resident, Department of Pathology, JNMC, AMU, Aligarh, Uttar Pradesh, India.
4 Professor, Department of Gynaecology, JNMC, AMU, Aligarh, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kafil Akhtar, Professor, Department of Pathology, JNMC, AMU, Aligarh, Uttar Pradesh, India.
E-mail: drkafilakhtar@gmail.com
The incidence of bilateral mature cystic teratoma of the ovary is only 10%. Ovarian mature cystic teratomas are common, benign, pelvic tumours and can be easily detected by ultrasonography. Recurrent ovarian teratomas are very rare, and cases of bilateral teratomas are even rarer. So, it is advisable to routinely check the ovary contralaterally during the surgical procedure along with careful pelvic sonographic examination of both the ovaries. Inadvertent extensive surgery should be avoided in this benign condition that might further compromise the fertility of young patients. We report a rare case of bilateral mature cystic teratoma of the ovary in a 28-year-old female, who presented to the gynaecologic outpatient department with complaints of intermittent dull aching, diffuse lower abdominal pain and dysmenorrhea for three months. Transvaginal ultrasonography revealed bilateral complex ovarian masses that raised suspicion of dermoid cysts with hypoechoic endometrial collections. Her Cancer Antigen 125 (CA-125) was normal. A bilateral ovarian cystectomy was performed and histopathology confirmed the diagnosis. This case highlights a rare occurrence of bilateral ovarian mature cystic teratoma, where cystectomy was performed to preserve the fertility in a young female.
Benign, Histopathology, Ovary, Tumour, Ultrasound
Case Report
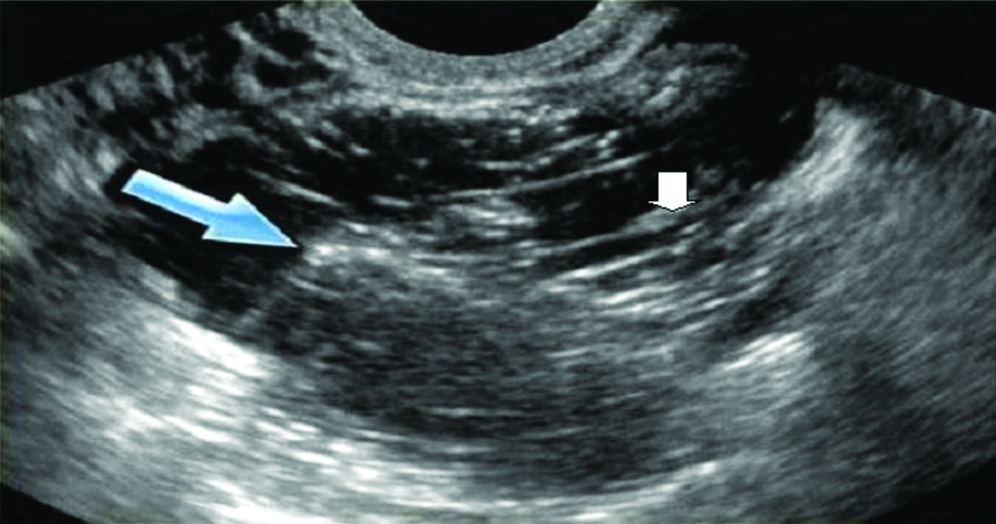
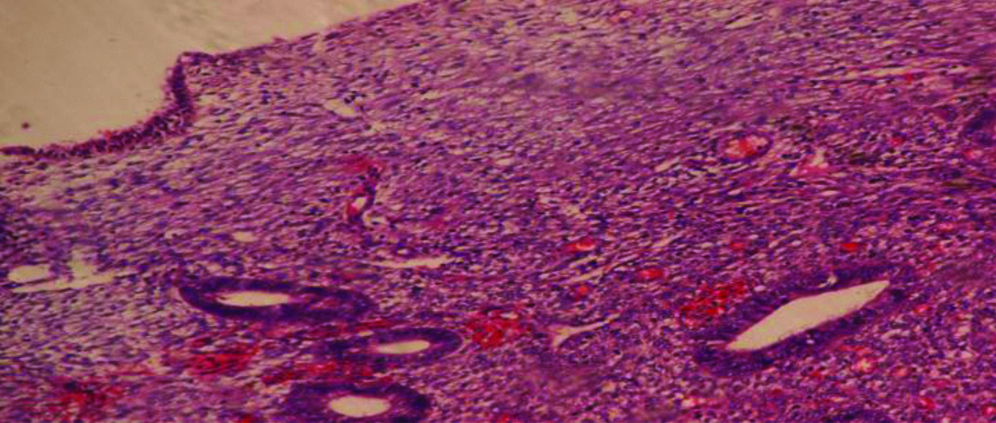
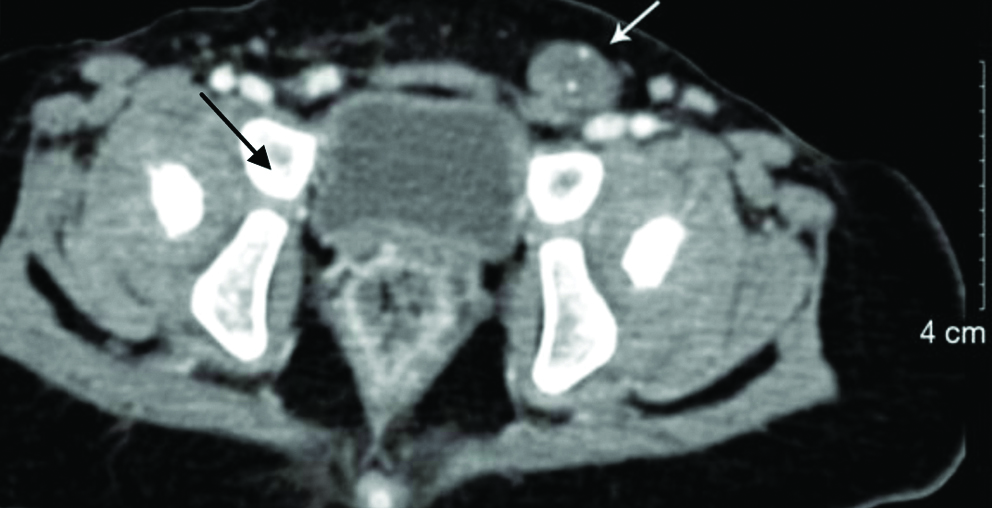
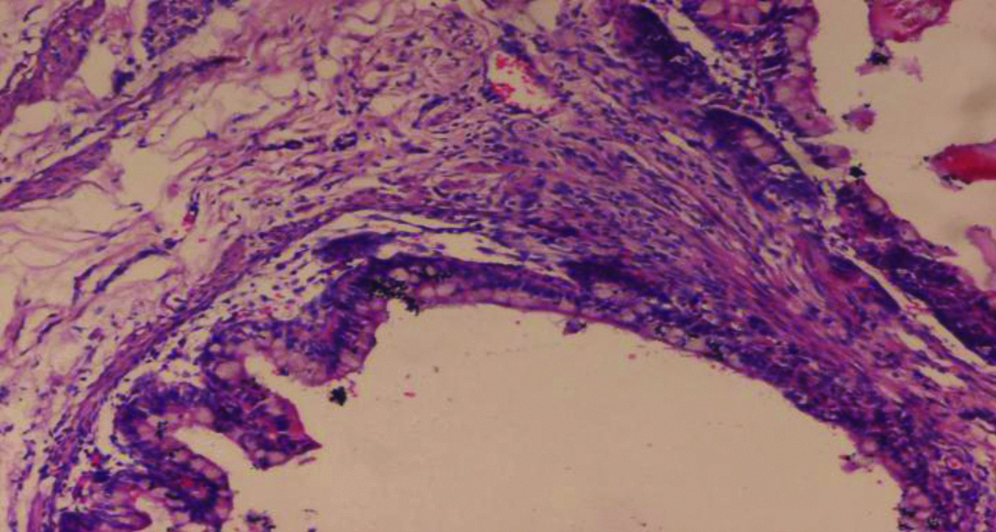
A 28-year-old female presented to the gynaecologic outpatient department with complaints of intermittent abdominal pain and dysmenorrhea for three months. There was no significant past or medical history. On examination, the patient was ill-looking, but her vital signs were stable. She had tenderness all over her abdomen, and a diffuse lump was felt in both adnexa. Her complete blood count was within the normal range. Transvaginal ultrasonography showed bilateral complex ovarian masses that raised suspicion of dermoid cysts with hypoechoic endometrial collection [Table/Fig-1]. Endometrial sampling showed inflammatory changes [Table/Fig-2] and her papanicolaou smear was normal without any evidence of dysplasia or infection. Serum CA-125 level was 33 U/mL. A pelvic Computed Tomography (CT) scan revealed a 4.0×3.7 cm, complex, cystic tumour on the left adnexa and 3.1×2.9 cm, solid-cystic tumour on the right adnexa [Table/Fig-3]. Based on the investigations, bilateral serous cystadenoma, serous cystadenocarcinoma and germ cell tumour was considered in the differentials, with the provisional diagnosis of bilateral germ cell tumour.
Transvaginal ultrasonography showed bilateral complex ovarian masses (blue and white arrow) with hypoechoic endometrial collection.
Tissue section from the endometrial sample shows glands and stroma densely infiltrated by inflammatory cells (H&E,100X).
Pelvic Computed Tomography (CT) scan revealed a 4.0×3.7 cm, complex, cystic tumour on the left adnexa and 3.1×2.9 cm, solid-cystic tumour on the right adnexa (black and white arrow).
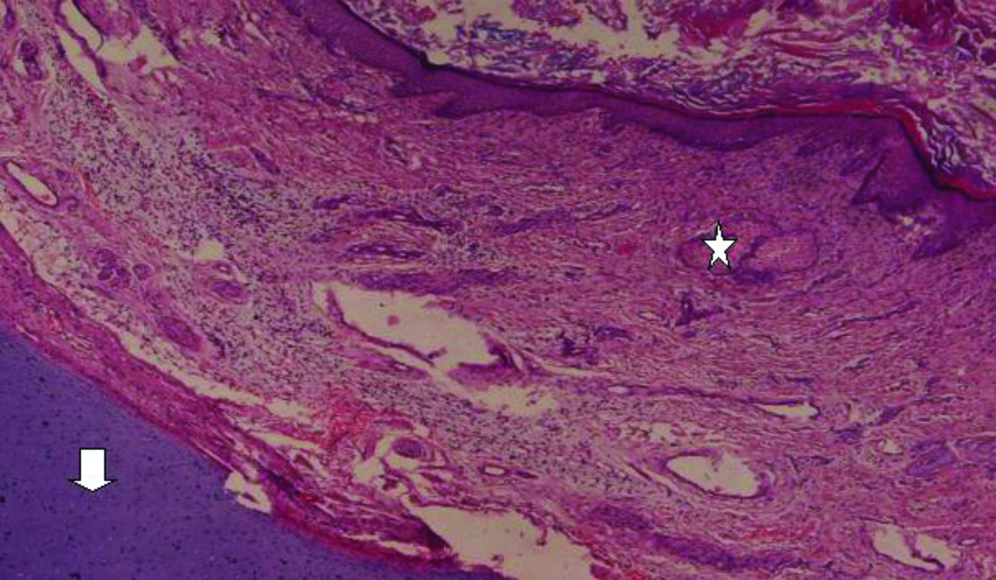
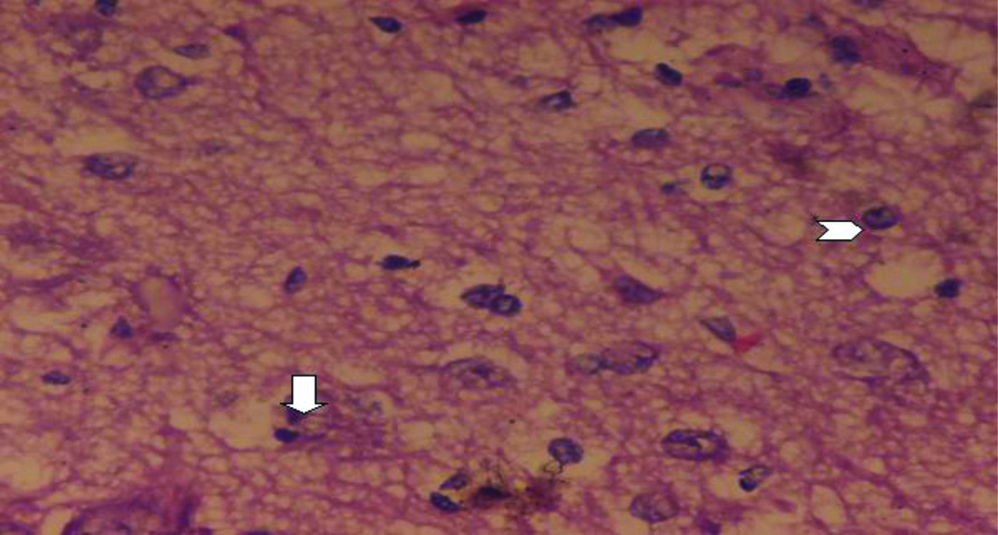
During exploratory laparotomy, bilateral dermoid cysts of 4×3 cm each, was detected with normal uterus. A bilateral ovarian cystectomy was performed. Grossly a capsulated, enlarged, 4.0×3.6 cm, left ovarian tumour with abundant sebaceous material and entangled hair was seen. The right ovarian mass was solid-cystic, with foci of necrosis, 3.1×2.7 cm in size [Table/Fig-4]. Histopathological findings of both the excised masses showed keratinised stratified squamous epithelium with keratinous debris and foci of sebaceous glands and hyaline cartilage [Table/Fig-5] mature neuroepithelium [Table/Fig-6] and glandular epithelium [Table/Fig-7] which confirmed the diagnosis of bilateral, mature cystic teratoma, as all mature germinative layer derivatives in the form of keratinised squamous epithelium, with sebaceous glands, mature hair and mature neural elements which were seen histologically. No evidence of malignancy was found. As it was a benign lesion, with curative surgery, no adjuvant therapy was advised. After 12 months of follow-up, the patient was fine with no complaints of abdominal pain or any signs of recurrence.
Grossly a capsulated, enlarged, 4.0×3.6 cm, left ovarian tumour with abundant sebaceous material and entangled hair was seen (L). The right ovarian mass was solid-cystic, with foci of necrosis, 3.1×2.7 cm in size (R).

Histopathological findings of both excised masses shows keratinised stratified squamous epithelium with keratinous debris with foci of sebaceous gland (star) and hyaline cartilage (white arrow). Haematoxylin and Eosin x 100.
Tissue section shows mature neuroepithelium with neurons (white arrow) and neuroglial cells (arrow head, H&E, 400X).
Histopathologic sections shows glandular epithelium with mature glands with mucin (H&E,100X).
Discussion
Bilateral mature cystic teratoma of the ovaries is a rare incidental finding [1]. In the present case, the patient had a history of bilateral mature cystic ovarian teratomas. To our knowledge, this is a rare case of bilateral mature cystic teratomas of the ovary. Mature cystic teratomas account for approximately 10-20% of the total cases of ovarian tumours [2,3]. The disease occurs from childhood to postmenopause but the peak incidence is seen between 20-40 years [3,4]. Mature cystic teratomas are benign tumours but may undergo malignant transformation in 0.1-0.2% cases [5,6]. They are slow-growing tumours, are unilateral however 8-12% cases are bilateral [7,8]. Also known as dermoid cysts, they comprise of only well-differentiated tissues. These are benign germ cell tumours and known to arise from any of the three germ cell layers [9]. The word “teratoma” is derived from the Greek word “teraton” meaning a monster. Virchow first described it in 1863, but Leblanc in 1831 coined the term “dermoid cyst.” The increasing hormonal levels of oestrogen and progesterone leads to an increase in size of mature cystic teratomas after puberty and decline in growth after menopause [8]. Mature cystic teratomas are an incidental finding during routine imaging or during lower abdominal surgeries [9,10]. These ovarian tumours show varied clinical features like abdominal pain with distension due to torsion of the tumour in children and adolescents [11].
Ultrasonography is an excellent, non-invasive, investigative procedure to detect any ovarian lump in women of any age [12,13]. Tumour markers such as CA-125, CA19-9 and alpha-fetoprotein aid in the early detection and characterisation of ovarian masses. Of all the tumour makers, serum CA19-9 is the most reliable biomarker of ovarian mature cystic teratomas [14]. Clinically serum CA-125 is still used to distinguish between benign and malignant pelvic masses with high CA-125 levels pointing towards a grave prognosis [15]. In the present case of bilateral ovarian involvement, CA-125 levels were normal. The CT is also helpful in the diagnosis of these tumours and shows a heterogeneous tumour mass arising from both the adnexa [13]. A definitive diagnosis of bilateral mature cystic teratomas can be confirmed after histopathologic biopsy examination of the laparoscopic surgical excised mass [16]. Laparoscopic surgery is a better and fertility-saving procedure for young females [13]. The incidence of tumour recurrence on the same ovary is 3-4% [17]. To avoid missing a tumour in the contralateral ovary, a biopsy from both ovaries during surgery is recommended [17]. Deligeoroglou E et al., have reported that young age (<30 years), large cyst size of diameter >8 cm and bilateral disease are predictors for recurrence with a high risk of recurrence, if more than one of these factors are present [18]. In the present case after 12 months of follow-up period, there was no sign of recurrence.
Conclusion(s)
Preoperative pelvic sonographic examinations of both ovaries are necessary in patients to avoid missing bilateral tumour. Clinicians must do incision biopsy in these ovarian tumours that may minimise an extensive surgery and might compromise the fertility of young patients.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 08, 2020
Manual Googling: Jul 29, 2020
iThenticate Software: Sep 23, 2020 (20%)
[1]. Krishna D, Kriti A, Savita S, Bilateral mature cystic teratomas of the ovary with endometrial cancer: A rare case presentationJ Gynaecol Surg 2017 33(3):117-20.10.1089/gyn.2016.0120 [Google Scholar] [CrossRef]
[2]. Chang CF, Lin CK, A case of recurrent, bilateral ovarian mature teratoma in a young womanBMC Women’s Health 2014 14:57-61.10.1186/1472-6874-14-5724726009 [Google Scholar] [CrossRef] [PubMed]
[3]. Srikanth S, Anandam G, Bilateral dermoid cyst of ovaryMed J DY Patil Univ 2014 7:492-93.10.4103/0975-2870.135281 [Google Scholar] [CrossRef]
[4]. Shi XX, Shen H, Chen T, Pan ZY, Wu XF, Zou ZN, Mature cystic teratoma of the ovary with three kinds of entire gastrointestinal wall and complete bronchial structure in a pregnant womanInt J Surg Pathol 2016 24(5):428-30.10.1177/106689691662828027098586 [Google Scholar] [CrossRef] [PubMed]
[5]. Sinha R, Sethi S, Mahajan C, Bindra V, Multiple and bilateral dermoids: A case reportJ Minim Invasive Gynaecol 2010 17(2):235-38.10.1016/j.jmig.2009.11.00520226415 [Google Scholar] [CrossRef] [PubMed]
[6]. Baek J, Synchronous occurrence of mature cystic teratoma of the fallopian tube and ovary: A case reportOncol let 2016 12(2):911-14.10.3892/ol.2016.474727446368 [Google Scholar] [CrossRef] [PubMed]
[7]. Ozgur T, Atik E, Silfeler DB, Toprak S, Mature cystic teratomas in our series with review of the literature and retrospective analysisArch Gynaecol Obstet 2012 285(4):1099-1101.10.1007/s00404-011-2171-822167448 [Google Scholar] [CrossRef] [PubMed]
[8]. Kim MJ, Kim NY, Lee DY, Yoon BK, Choi D, Clinical characteristics of ovarian teratoma: Age-focused retrospective analysis of 580 casesAm J Obstet Gynaecol 2011 205:01-32.10.1016/j.ajog.2011.02.04421507373 [Google Scholar] [CrossRef] [PubMed]
[9]. Kahraman K, Cetinkaya SE, Kankaya D, Dunder I, Soylemez F, Squamous cell carcinoma arising from mature cystic teratoma of the ovary with synchronous endometrial adenocarcinomaJ Obstet Gynaecol Res 2011 37:146-50.10.1111/j.1447-0756.2010.01323.x21083842 [Google Scholar] [CrossRef] [PubMed]
[10]. Alotaibi MO, Navarro OM, Imaging of ovarian teratomas in children: A 9-year reviewCan Assoc Radiol J 2010 61(1):23-28.10.1016/j.carj.2009.07.00119931379 [Google Scholar] [CrossRef] [PubMed]
[11]. El-Agwany AS, Moneim AS, Multiple bilateral huge synchronous ovarian mature cystic teratomas: A rarely encountered condition in practiceEgyptian J Radiol Nuclear Med 2015 46(1):195-97.10.1016/j.ejrnm.2014.11.001 [Google Scholar] [CrossRef]
[12]. Iman F, Bose K, Tarek A, Reema O, Mayed AD, Multiple bilateral ovarian mature cystic teratomas with ovarian torsion: A case reportOMJ 2018 32(2):163-66.10.5001/omj.2018.3029657687 [Google Scholar] [CrossRef] [PubMed]
[13]. Al Jama FE, Al Ghamdi AA, Gasim T, Al Dakhiel SA, Rahman J, Rahman MS, Ovarian tumours in children and adolescents-A clinical study of 52 patients in a university hospitalJ Pediatr Adolesc Gynaecol 2011 24:25-28.10.1016/j.jpag.2010.06.00520709583 [Google Scholar] [CrossRef] [PubMed]
[14]. Bast RC Jr, Badgwell D, Lu Z, Marquez R, Rosen D, Liu J, New tumour markers: CA125 and beyondInt J Gynaecol Cancer 2005 15:274-81.10.1111/j.1525-1438.2005.00441.x16343244 [Google Scholar] [CrossRef] [PubMed]
[15]. Emin U, Tayfun G, Cantekin I, Ozlem UB, Umit B, Leyla M, Tumour markers in mature cystic teratomas of the ovaryArch Gynaecol Obstet 2009 279:145-47.10.1007/s00404-008-0688-218506458 [Google Scholar] [CrossRef] [PubMed]
[16]. Lee KH, Song MJ, Jung IC, Lee YS, Park EK, Autoamputation of an ovarian mature cystic teratoma: A case report and a review of the literatureWorld J Surg Oncol 2016 14(1):217-19.10.1186/s12957-016-0981-727535361 [Google Scholar] [CrossRef] [PubMed]
[17]. Abha S, Ayman AE, Ovarian mature cystic teratoma: Challenges of surgical managementObst Gynae Int 2016 23:01-08. [Google Scholar]
[18]. Deligeoroglou E, Eleftheriades M, Shiadoes V, Botsis D, Hasiakos D, Kontoravdis A, Ovarian masses during adolescence: Clinical, ultrasonographic and pathologic findings, serum tumour markers and endocrinological profileGynaecol Endocrinol 2004 19:01-08.10.1080/0951359041000171289515625766 [Google Scholar] [CrossRef] [PubMed]