The Pneumoperitoneum (PNP) is created by insufflation of a gas in the peritoneal cavity. Laparoscopy is a procedure performed in the abdomen or pelvis through small incisions with the aid of a camera. It can either be used to inspect and diagnose a condition or to perform surgery. Now operative laparoscopy has become the standard approach for most common surgeries, including cholecystectomy, tubal ligation, appendectomy, and ovarian cystectomy [1].
The procedure of laparoscopy essentially involves creation of an artificial PNP, usually using carbon dioxide (CO2) gas. A laparoscopic surgery always poses some challenges to its successful anaesthetic management, mainly due to significant alteration of haemodynamics. As in LC initial trendelenburg position, creation of PNP, systemic absorption of carbon dioxide and reverse Trendelenburg position cause pathophysiological changes in various systems of the body leading to increase in plasma level of nor-epinephrine, epinephrine and plasma renin activity. All these factors together contribute to increase in Heart Rate (HR), Mean Arterial Pressure (MAP) and increased systemic and pulmonary vascular resistance along with reduced cardiac output. These haemodynamic changes predispose the myocardium in vulnerable patients to ischemic changes [2].
Increase in HR and blood pressure in response to PNP during LC is a challenging situation for anaesthesiologist. Without adequate control of sympathetic response there are more chances of increase in morbidity. Various agents such as benzodiazepine, beta blockers, opioid analgesics, calcium channel blockers and vasodilators have been used with variable success [3].
None of the above agents has been proved to be ideal and these drugs have no role for induction, maintenance of anaesthesia and also cause dangerous complications. Hence, the search for an ideal agent to attenuate the haemodynamic responses is still continuing. Dexmedetomidine is a newer highly selective α2-adrenergic agonist, approved by FDA in December 1999 for sedation of patients in Intensive Care Units not longer than 24 hours. It has 10-fold greater α2/α1-receptor selectivity and a shorter duration of action. It possesses anxiolytic, hypnotic, sedative, sympatholytic and analgesic properties without producing significant respiratory depression [4].
Opioids can be used as sole or supplementary agent for induction of anaesthesia. Narcotics are very commonly used for intraoperative analgesia, therefore there is no additional cost involved. Fentanyl is a potent synthetic opioid agonist and phenylpiperidine derivative. It acts on μ receptors. Fentanyl is more potent than commonly used opioids, such as meperidine or morphine. The large safety margin, relatively short duration of action, peak effect at 5-7 minutes and minimal respiratory depression at analgesic doses made it the drug of choice for intravenous anaesthesia [5].
Various studies have done before to study the effects of various drugs on haemodynamic changes during laryngoscopy and intubation but there is paucity of literature on effects of various drugs on haemodynamic changes during PNP. Kataria AP et al., studied the efficacy of dexmedetomidine and fentanyl on pressor response and PNP in LC [2]. Joris Jean L et al., studied effects of clonidine on haemodynamic changes induced by laparoscopy and PNP [6]. Present study provides an aid for better management of haemodynamic changes during PNP in laparoscopic surgeries.
The primary outcome of study was to assess and compare the change in haemodynamic variables (HR, SBP, DBP, MAP) after PNP in both the study groups and secondary outcomes included to assess and compare the duration of postoperative analgesia, postoperative sedation level and incidence of side effects (if any) in both the study groups. Both drugs were used in infusion form.
Materials and Methods
A randomised, double-blind study was conducted at SMS Medical College and Hospital, Jaipur, Rajasthan, India for a period of five months (July-November 2019) after prior approval by the Institutional thesis and Ethics Committee {53/MC/EC/2019 dated 08/01/2019} {CTRI/2019/07/019958 registered on 01/07/2019}.
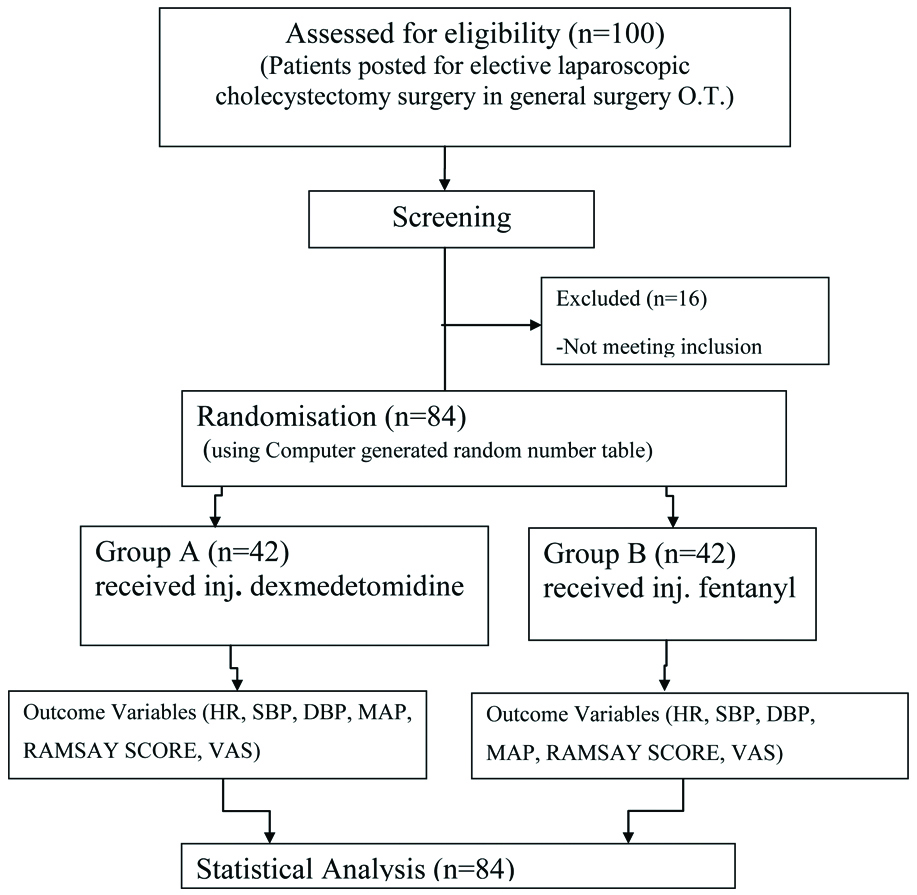
Total 84 ASA Class I and II patient’s aged 18-50 years and weighing 40 to 70 kg undergoing elective LC under general anaesthesia were included and patients who refused to participate in the study, having history of allergy to anaesthetic agents used in study, pre-existing cardiac disease, hypertension, asthma, renal or hepatic dysfunction and anticipated difficult intubation were excluded from the study. Patients intubated after more than one attempt or more than 45 seconds were also excluded from the study.
The patients were randomised into two groups using online random number generator software Random® and divided into two groups (each containing 42 patients): Group A (dexmedetomidine group) and Group B (fentanyl group) [Table/Fig-1].
On arrival of patient in the operation theatre fasting status, written informed consent and Pre-Anaesthetic Checkup (PAC) was checked. Routine noninvasive monitors {Non-Invasive Blood Pressure (NIBP), Electrocardiogram (ECG), Blood Oxygen Saturation (SpO2) probe} were attached and baseline parameters i.e., HR, Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DBP), MAP, and SpO2 were noted. Intravenous line (IV) was secured and IV fluid Ringer Lactate (RL) was started at ten mL/kg/hour. Patients were premedicated with inj. ranitidine 50 mg IV, inj. glycopyrrolate 0.2 mg IV and inj. midazolam 0.01 mg/kg IV 20 minutes prior to study drug. Loading infusion of study drugs was made by diluting dexmedetomidine (1 mcg/kg IV) or fentanyl (1 mcg/kg IV) with normal saline to make a total volume of ten mL and injected IV slowly over ten minutes. An independent anaesthetist gave study drug and didn’t participate in the study of data variable. Patients as well as assessor were blinded regarding group allocation of the study patient.
In group A, intravenous infusion of dexmedetomidine was started at a rate of as per guidelines 1 μg/kg over 10 min. followed by induction and then continuous infusion at the rate of 0.2 μg/kg/hr throughout the surgery was given. In Group B, fentanyl was given as loading infusion at the rate of 1 μg/kg over 10 min. followed by induction and then continuous infusion at the rate of 0.2 μg/kg/hr.
Induction was done 10 minutes after start of loading infusion. Patient was pre-oxygenated with 100% O2 for three minutes. Induction was done with inj. propofol 2 mg/kg IV followed by inj. atracurium 0.5 mg/kg IV and ventilated with 100% oxygen for three minutes. Direct laryngoscopy was done and patient was intubated with appropriate size endotracheal tube. Bilateral air entry was checked and tube fixed.
Intraoperative anaesthesia was maintained with 60%N2O+40% O2, inj. atracurium 0.1 mg/kg IV and isoflurane. PNP was created with peritoneal insufflation with CO2 (at the rate of two L/min). Intra-Abdominal Pressure (IAP) was maintained at 12-14 mmHg. End-tidal CO2 (EtCO2) was maintained between 35 and 40 mmHg by mechanical ventilation.
Data were recorded before induction, one minute after induction, one minute after intubation, five minutes after intubation, one, three, five minutes after PNP and at ten min interval during PNP throughout the surgery and after extubation. Intraoperative haemodynamic were managed by inhalational agent isoflurane.
At the end of the surgery infusion of study drug was stopped and patient was reversed with Inj. neostigmine (0.05 mg/kg IV) and Inj. glycopyrrolate (0.008 mg/kg IV) and extubation was done. Patient was shifted to recovery room. In recovery room, postoperative sedation level was measured by using Ramsay Sedation Score in every 30 minutes after extubation and postoperative analgesia evaluated by VAS in every 30 minutes. Rescue analgesia inj. Diclofenac 75 mg IV was given when VAS score is four or more and also observed for any side effects.
Statistical Analysis
Data collected were entered in Microsoft excel software and statistical analysis was performed with SPSS-21 statistical software package for windows (SPSS inc, Chicago, IL, USA). Sex and ASA grade of patients were presented as numbers and were compared among groups using Chi-square test. Age, weight, HR, systolic BP, diastolic BP, mean BP, SpO2 were summarised in form of Mean±SD. The difference in mean was analysed using the Student’s t-test. Significance level was taken as p-value <0.05.
Results
There was no statistically significant difference between the groups with regards to age, sex, weight and duration of surgery (p>0.05) [Table/Fig-2]. The mean baseline haemodynamic variables were also comparable between both groups.
In [Table/Fig-3] the mean HR increased one minute after intubation to 98.14±15.42 bpm in group A and 108.40±20.18 bpm in group B and the difference was statistically significant between the two groups (p<0.05). Results showed that intraoperatively, throughout the period of PNP, Group A showed HR comparable to baseline or slight fall from baseline, whereas in Group B the HR constantly remained above the baseline throughout the intraoperative period and the difference between two group was statistically significant (p<0.05) at all time points.
Demographic data and duration of surgery.
| Variables | Group A | Group B | p-value |
|---|
| Mean±SD | Mean±SD |
|---|
| Age (years) | 37.26±8.63 | 35.31±10.33 | 0.349 |
| Weight (kg) | 56.82±10.14 | 55.40±11.53 | 0.550 |
| Sex (Male/Female) | 10/32 | 9/33 | 0.797 |
| Duration of surgery (Min.) | 42.29±4.53 | 43.05±3.39 | 0.385 |
Chi-square test
Comparison of Heart rate (bpm) between study groups at different time intervals.
| Heart Rate | Group A | Group B | p-value |
|---|
| Mean | SD | Mean | SD |
|---|
| Baseline | 95.57 | 16.74 | 98.07 | 18.21 | 0.514 |
| Before induction | 92.57 | 15.41 | 95.55 | 19.10 | 0.434 |
| 1 min after induction | 91.62 | 15.60 | 93.31 | 18.43 | 0.651 |
| 1 min after intubation | 98.14 | 15.42 | 108.40 | 20.18 | 0.010 |
| 5 min after intubation | 95.69 | 15.25 | 108.48 | 19.15 | 0.001 |
| 1 min after PNP* | 96.86 | 13.91 | 110.21 | 18.18 | <0.001 |
| 3 min after PNP | 95.14 | 14.00 | 106.90 | 15.61 | <0.001 |
| 5 min after PNP | 94.81 | 14.08 | 108.21 | 15.20 | <0.001 |
| 10 min after PNP | 94.88 | 13.91 | 109.93 | 17.14 | <0.001 |
| 20 min after PNP | 93.90 | 13.14 | 110.81 | 17.64 | <0.001 |
| 30 min after PNP | 93.82 | 13.23 | 109.95 | 13.87 | <0.001 |
| 40 min after PNP | 84.50 | 15.81 | 107.00 | 18.72 | 0.035 |
| After extubation | 104.29 | 13.94 | 121.10 | 16.93 | <0.001 |
PNP: Pneumoperitonium; Student t-test
One minute after intubation the SBP increased to 123.76±10.18 mmHg in group A and 130.52±14.36 mmHg in group B. These findings continued till 5 minutes after intubation and showed that rise in SBP was statistically significant in group B [Table/Fig-4]. Results showed that throughout the PNP the rise in mean SBP was observed in both the groups but this rise was more in group B than group A which was statistically significant (p<0.05). The same trend continued throughout the surgery except 40 minutes after PNP creation [Table/Fig-4].
Systolic Blood Pressure (SBP) (mmHg) of study groups at different time intervals.
| Systolic BloodPressure | Group A | Group B | p-value |
|---|
| Mean | SD | Mean | SD |
|---|
| Baseline | 126.23 | 8.83 | 122.73 | 9.74 | 0.150 |
| Before induction | 121.29 | 8.33 | 118.17 | 12.26 | 0.176 |
| 1 min after induction | 114.95 | 12.84 | 117.86 | 14.56 | 0.334 |
| 1 min after intubation | 123.76 | 10.18 | 130.52 | 14.36 | 0.014 |
| 5 min after intubation | 124.17 | 11.65 | 133.07 | 12.98 | 0.001 |
| 1 min after PNP* | 126.86 | 7.73 | 134.29 | 9.40 | <0.001 |
| 3 min after Pnp | 126.31 | 7.54 | 138.40 | 8.14 | <0.001 |
| 5 min after PNP | 127.17 | 7.32 | 138.98 | 7.86 | <0.001 |
| 10 min after PNP | 129.86 | 7.52 | 136.43 | 8.37 | <0.001 |
| 20 min after PNP | 127.45 | 7.80 | 138.69 | 8.76 | <0.001 |
| 30 min after PNP | 129.76 | 7.84 | 138.33 | 8.29 | <0.001 |
| 40 min after PNP | 127.67 | 10.65 | 138.50 | 13.08 | 0.124 |
| After extubation | 134.88 | 9.57 | 145.74 | 8.14 | <0.001 |
*PNP: Pneumoperitonium; Student t-test
One minute after intubation the DBP increased to 82.5±9.24 mmHg in group A and 85.38±11.99 mmHg in group B but the difference was statistically insignificant (p=0.232). The findings after 5 minutes of intubation showed that rise in DBP was statistically significant in group B. (p=0.014). After creating PNP rise in mean DBP was observed in both the groups but this rise was more in group B which was statistically significant (p<0.05) at 3, 20 and 30 minutes post CO2 insufflation [Table/Fig-5].
Diastolic Blood Pressure (DBP) (mmHg).
| Diastolic Blood Pressure | Group A | Group B | p-value |
|---|
| Mean | SD | Mean | SD |
|---|
| Baseline | 83.27 | 8.36 | 81.77 | 8.54 | 0.494 |
| Before induction | 80.60 | 8.25 | 79.67 | 12.14 | 0.682 |
| 1 min after induction | 75.74 | 10.66 | 77.00 | 12.40 | 0.618 |
| 1 min after intubation | 82.57 | 9.24 | 85.38 | 11.99 | 0.232 |
| 5 min after intubation | 82.55 | 9.09 | 87.90 | 10.61 | 0.014 |
| 1 min after PNP* | 85.33 | 7.83 | 88.69 | 10.28 | 0.096 |
| 3 min after PNP | 86.60 | 6.58 | 90.38 | 7.80 | 0.018 |
| 5 min after PNP | 85.36 | 7.80 | 88.86 | 9.27 | 0.064 |
| 10 min after PNP | 86.74 | 6.81 | 88.93 | 9.28 | 0.221 |
| 20 min after PNP | 85.45 | 6.11 | 91.19 | 8.57 | <0.001 |
| 30 min after PNP | 86.76 | 6.15 | 90.49 | 7.59 | 0.020 |
| 40 min after PNP | 86.83 | 8.16 | 87.13 | 15.18 | 0.966 |
| After extubation | 88.50 | 6.87 | 95.02 | 8.90 | <0.001 |
*PNP: Pneumoperitonium; Student t-test
After creating PNP, rise in MAP was observed in both group A and group B, 99.38±6.32 and 103.43±9.81, respectively but this rise was more in group B which was statistically significant (p<0.05) throughout the surgery except 40 minutes after PNP creation [Table/Fig-6].
Mean Arterial Blood Pressure (MAP) (mmHg) of study groups at different time intervals.
| Mean ArterialPressure | Group A | Group B | p-value |
| Mean | SD | Mean | SD |
| Baseline | 97.50 | 8.14 | 94.10 | 7.24 | 0.092 |
| Before induction | 94.10 | 8.62 | 92.10 | 10.61 | 0.345 |
| 1 min after induction | 88.76 | 11.30 | 90.83 | 13.17 | 0.441 |
| 1 min after intubation | 96.12 | 9.18 | 100.83 | 12.93 | 0.057 |
| 5 min after intubation | 96.31 | 9.58 | 103.38 | 11.74 | 0.003 |
| 1 min after PNP* | 99.38 | 6.32 | 103.43 | 9.81 | 0.027 |
| 3 min after PNP | 99.21 | 6.21 | 106.95 | 7.72 | <0.001 |
| 5 min after PNP | 98.74 | 7.18 | 105.45 | 7.59 | <0.001 |
| 10 min after PNP | 101.21 | 6.21 | 104.88 | 8.89 | 0.031 |
| 20 min after PNP | 100.19 | 6.33 | 106.90 | 8.74 | <0.001 |
| 30 min after PNP | 100.95 | 6.44 | 106.64 | 7.20 | <0.001 |
| 40 min after PNP | 99.00 | 9.17 | 103.63 | 11.12 | 0.424 |
| After extubation | 103.79 | 7.97 | 111.24 | 9.64 | <0.001 |
*PNP: Pneumoperitonium; Student t-test
In the present study, time to first rescue analgesia or mean duration of postoperative. Analgesia (VAS>3) was significantly longer in dexmedetomidine group (102.14±32.50 minutes) than fentanyl group (42.86±15.03 minutes) with p-value <0.001.
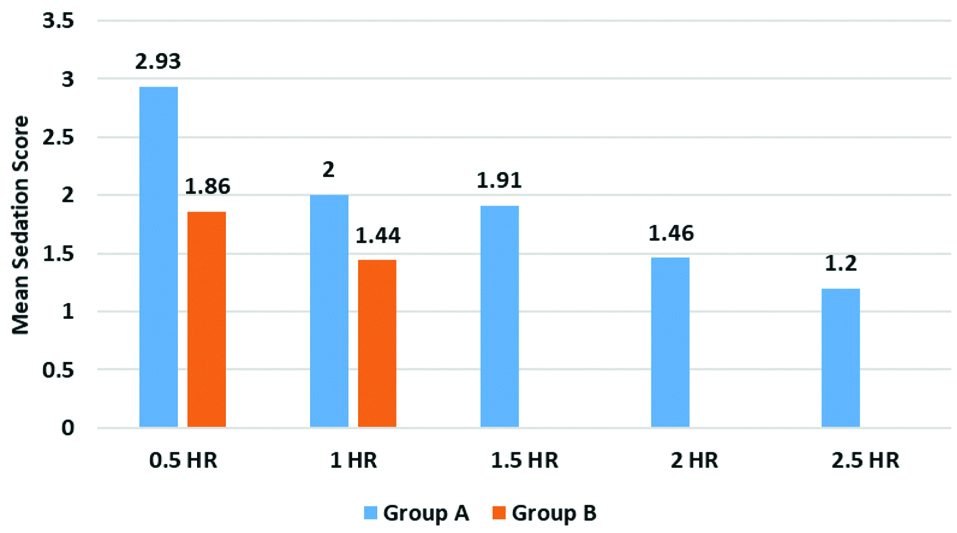
Mean sedation score at 0.5 hour after surgery was 2.93±0.34 in group A and 1.86±0.81 in group B and 1 hour after surgery it was 2±0.55 in group A and 1.44±0.51 in group B. The difference in mean sedation score between group A and group B was statistically significant (p<0.001) [Table/Fig-7].
Mean sedation scores at different time intervals.
Discussion
Dexmedetomidine, a potent α2-adrenoreceptor agonist, also has been tried in various studies to attenuate haemodynamic alterations due to stress of surgery and anaesthesia during PNP in LC [2,7,8]. In present study, it was observed that dexmedetomidine group had a significantly better attenuation of HR response to pneumoperitonium as compared to fentanyl group. This is because dexmeditomidine effectively blunts sympathoadrenal response to pneumoperitonium and has good sympatholytic activity [9].
Kataria AP et al., also found that the HR was increased during PNP in both dexmedetomidine group and fentanyl group but in dexmedetomidine group HR returned to baseline at around 30 to 45 min after creation of PNP while in fentanyl group after creation of PNP, HR remained above the baseline until the end of PNP [2]. Similar observations were also noted by Neil L et al., and Vaswani JP et al., they found that dexmedetomidine group had better attenuation of HR during PNP as compared to fentanyl group [7,8].
In the present study, there was less fluctuation in SBP, DBP and MAP in dexmedetomidine group in comparison to fentanyl with p-value <0.05 after intubation, after PNP and after extubation. Dexmedetomidine stimulates receptors in the medullary vasomotor center, reducing norepinephrine turnover and controls central sympathetic outflow. This results alterations in sympathetic function, hence suppressing the haemodynamic response to PNP. It leads to a dose dependent decrease of BP and HR due to decrease in serum norepinephrine concentrations. Also, this is due to decrease in central stimulation of parasympathetic outflow and inhibition of sympathetic outflow from the brainstem- the locus coeruleus [7].
Dexmedetomidine provides good analgesia postoperatively. Dexmedetomidine provides analgesia by suppression of neuronal firing in the locus coeruleus along with inhibition of norepinephrine release and activity in the descending medullospinal noradrenergic pathway, secondary to activation of central α2 adrenoceptors [10]. Bajwa SS et al., conducted a study on preoperative use of dexmedetomidine on attenuation of haemodynamic response and postoperative analgesic requirements and found that requirement of analgesia in the postoperative period was lower in dexmedetomidine group than fentanyl group [11].
In the study conducted by Vaswani JP et al., postoperatively the mean duration of adequate analgesia was 81.233±16.515 minutes in Group D whereas it was 41.87±10.180 minutes in Group F, (p-value 0.001) which is statistically significant [8].
Kataria AP et al., also found that in their study postoperative VAS score was higher in fentanyl group than in dexmedetomidine group [2]. Helmy N et al., showed similar results in VAS score as in present study during postoperative period and these findings were also consistent with that of Turgut N et al., and Gurbet A et al., [12-14].
In present study patients that received dexmedetomidine were better sedated with higher Ramsay sedation score but were easily arousable with the help of verbal or physical stimuli. Patel CR et al., also found that postoperatively dexmedetomidine (1 μg/kg) shows significant sedation at two hours than fentanyl (2 μg/kg) [15].
Studies done by Vaswani JP et al., and Patel ND et al., also support the findings of present study [8,16]. However, Kataria AP et al., found comparable sedation in both the groups. In their study orientation time was more in fentanyl group than in dexmedetomidine group [2]. Dexmedetomidine can lead to cardiovascular depression, causing bradycardia and hypotension. But, none of the patients in the present study had such an incidence, possibly due to the use of a lower dose and of dexmedetomidine [17,18].
Limitation(s)
Absence of a placebo-controlled group; Cardiac output, systemic vascular resistance and plasma catecholamine or stress hormone concentrations were not measured. Monitoring of invasive blood pressure could be more accurate. Cerebral perfusion pressure studies to establish patient safety and use of Bispectral Index (BIS) for monitoring depth of anaesthesia that could be more informative as changes in depth of anaesthesia also leads to changes in haemodynamics.
Conclusion(s)
Dexmedetomidine and fentanyl are administered intravenously, dexmedetomidine shows better attenuation of haemodynamic response to PNP in laparoscopic surgeries as compared to fentanyl with better sedation, larger duration of analgesia and no significant side effects.
Chi-square test
PNP: Pneumoperitonium; Student t-test
*PNP: Pneumoperitonium; Student t-test
*PNP: Pneumoperitonium; Student t-test
*PNP: Pneumoperitonium; Student t-test