Fetal Autopsy Showing Two Ventral Body Wall Defects: An Unusual Presentation
Anupriya Kaur1, Arun Prasad2, Jessy Jayaraman Pushpaja3, Kanchan Kapoora4
1 Assistant Professor, Department of Paediatrics (Genetics), PGIMER, Chandigarh, India.
2 Tutor, Department of Anatomy, Symbiosis Medical College for Women, Symbiosis International University, Pune, India.
3 Senior Resident, Department of Anatomy, AIIMS, New Delhi, Delhi, India.
4 Professor and Head, Department of Anatomy, Government Medical College and Hospital, Chandigarh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anupriya Kaur, Assistant Professor, Department of Paediatrics (Genetics), Advanced Paediatric Center, Room No. 4110, PGIMER, Chandigarh-160012, India.
E-mail: anukaur.genetics@gmail.com
Thoracoschisis and gastroschisis are types of ventral body wall defects. Usually thoracoabdominoschisis presents as a continuous defect. Here the authors present the case of autopsy of 18 weeks old fetus with two well-separated ventral body wall defects. Thoracoschisis was a right lateral thoracic wall defect while gastroschisis, a midline infraumblical abdominal wall defect. Through the right lateral thoracic wall parts of two organs appeared to be protruding. On dissection, 8th and 9th ribs with the liver and the lower lobe of the right lung were herniating outside the body. The right lung was haemorrhagic. Various embryological theories on ventral body wall defects have been discussed in view of the present case.
Embryology, Fetus, Gastroschisis, Thoracoschisis
Case Report
An autopsy of 18-week-old fetus was performed. Mother was 19 years-old without history of any chronic illness or drug intake during pregnancy. Antenatal scan done at 18 weeks of pregnancy suggested a meningomyelocele, after which the pregnancy was terminated surgically.
Fetal autopsy was performed after obtaining written consent. The fetus was male with anthropometric parameters corresponding to approximate 20-22 weeks. Gastroschisis with a small defect in the abdominal wall in midline adjacent and inferior to the umbilicus was noted. The umbilical cord was normally inserted and the abdomen was distinctly scaphoid. There was an approximately 3×2 cm defect in the right lateral thoracic wall through which parts of two organs appeared to be protruding. On dissection, this defect was found to be between the 8th and 9th ribs with the liver and the lower lobe of the right lung herniating outside the body [Table/Fig-1,2]. The round ligament was passing through the diaphragm connecting the liver above to the umbilical cord below. The stomach was notably horizontal in its orientation [Table/Fig-3].
Fetal photograph showing two body wall defects- a midline infraumblical gastroschisis and right lateral thoracoschisis. Note the traumatic appearance of the liver due to exteriorization. U-Umblical cord.

Fetal photograph (lateral view) showing the extent of thoracic wall defect with liver and a tongue like protrusion of the lower lobe of the right lung herniating outside the body. Also seen is scaphoid abdomen and gastroschisis. R-Rib, SI-Small Intestine, U-Umblical cord.

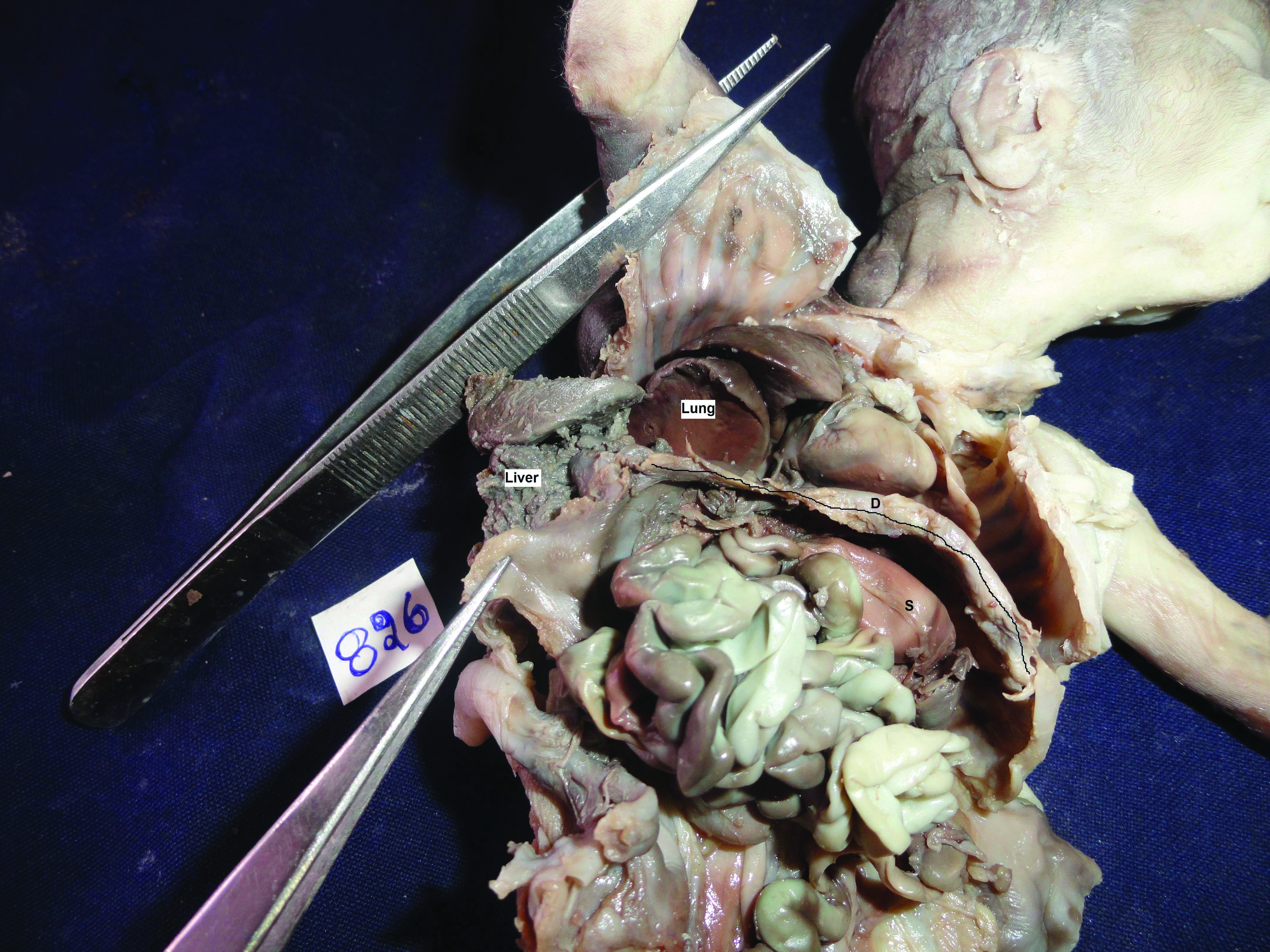
Fetal photograph after dissection showing a horizontally oriented stomach(S), diaphragm (D-outlined), haemorrhagic right lung and the absence of liver in abdominal cavity.
The rest of the abdominal examination was normal. The right lung was haemorrhagic. An overlying area of haemorrhage was also found over the right scapula suggesting trauma to the fetus as was also suggested by the nibbled appearance of the liver. The heart and great vessels did not show any major defect. There were no constriction rings or limb reduction defect in the extremities. Grossly no neural tube defect was seen. The face was not dysmorphic and there were no facial clefts. The anal opening was normal and the external genitalia were of the normal male type. The placenta was not available for examination. The fetal radiograph showed 12 pair of ribs and a discontinuity in the right sided thoracic wall.
Discussion
Congenital thoracoschisis and gastroschisis are types of ventral body wall defects with evisceration of organs outside the body. Thoracoabdominoschisis implies a midline continuous defect in the thoracic and abdominal walls. A defect of only the ribs results in lateral thoracoschisis which is a very rare congenital anomaly. There are only nine published case reports on this condition. Karaman I et al., have presented their case and reviewed four earlier case reports [1]. Additionally two cases labeled as Congenital Intercostal Liver Herniation by Ertan G et al., one case each by Bhattacharya NC et al. and Seleim HM et al., were found to be published [Table/Fig-4] [1-8].
Cases of thoracoschisis reported in literature.
| Author | Thoracic defect | Abdominal defect | Additional abnormalities |
|---|
| Karaman I et al., [1] | Left eight Intercostal space | None | ASD, PDA |
| Ertan G et al., [2] | Case 1-Right sided thoracic wall defectCase 2- Right lateral chest wall defect | Case 1- Diaphragmatic eventratioCase 2-Omphalocele with eventrated diaphragm | Case 1-B/L short arms with clinodactyly of the right 5th finger, a digitalised thumb and camptodactyly of the left index finger |
| Bhattacharya NC et al., [3] | Right thoracic wall defect | Right supraumblical abdominal wall defect | Agenesis of the right upper limb with a rudimentary finger-like structure attached to the right shoulder |
| Seleim HM et al., [4] | Left anterior thoracic wall widely spaced ribs | - | Dextrocardia, PDA |
| Davies MRQ and Cywes S [5] | Left third intercostal | Left anterolateral diaphragmatic defect | No left forearm, syndactyly, dextrocardia |
| Bamforth JS et al., [6] | Left sixth rib | Left posterior diaphragmatic defect | Left Poland anomaly, left scapula hypoplastic, no humerus-radius-ulna, dextrocardia, ectopic pancreas in the duodenum, intestines in the left hemithorax |
| Derbent M and Balci S [7] | Right second to fourth ribs | Right anterolateral diaphragmatic defect | - |
| Biri A et al., [8] | Left (location not specified) | Hiatus hernia | Left forearm agenesis, right arm-hand agenesis, spleen, stomach, colon, liver herniated into the thorax, VSD |
| Present case | Right eight and ninth ribs | Gastroschisis (adjacent and inferior to the umbilicus) | None |
ASD: Anterior septal defect; PDA: Patent ductus arteriosus; VSD: Ventral septal defect; B/L: Bilateral
To summarise, all these cases had thoracic wall defect (left sided> right sided) with diaphragmatic defect such that the corresponding lobe of the liver (Left/Right) herniated outside the body and other intra-abdominal organs herniated in the thoracic cavity. All cases except three, had associated upper limb anomalies in the form of syndactyly, camptodactyly, digitalization of thumb, Poland anomaly, hypoplastic scapula and agenesis of forearm on the side of thoracoschisis. The case by Karaman I et al., however had only congenital heart defects which were Patent Ductus Arteriosus and Atrial Septal Defect [1]. Patent Ductus Arteriosus was also seen in the case by Seleim HM et al., [4].
The case of this study differs from the cases of thoracoabdominoschisis in not being a continuous midline body wall defect but two well-separated defects i.e., a right lateral thoracic wall and a midline infraumblical abdominal wall defect. It also differs from the cases of thoracoschisis by neither having any associated limb or heart defects. Also, in the index case there is assosiated gastroschisis along with thoracoschisis. The case by Ertan G et al., had omphalocele along with thoracoschisis [2]. However, omphalocele is considered to have an altogether different aetiology i.e., failure of the bowel loops to return into the abdominal cavity after physiological herniation rather than defect in ventral abdominal wall closure leading to gastroschisis [9].
A number of theories on the embryological basis of ventral body wall defects have been proposed. We ruled out some of these as:
Early embryonic maldevelopment due to defect in the germ disc leading to blastogenic anomalies[10]: This presents with multiple congenital anomalies which were not there in this case.
Amniotic band disruption theory wherein a primary rupture of amnion causes direct mechanical disruption of organs. This would present with body wall defects together with, constriction rings with limb deficiencies, cranio-facial anomalies lacking in the present case [10].
Vascular disruption theory: Here altered vascular blood flow leads to disruption and incomplete embryonic development. This is less likely in this case as there were two distant body wall defects and not a localised one [10].
Body wall hypothesis proposed by Duhamel B in 1963 [11] says that a primary effect on the mesenchyme (lateral plate mesoderm) of the lateral body folds by a teratogen is responsible for ventral body wall defects. The teratogenic effect is on cell proliferation, migration, production of extracellular matrix resulting in failure of proper movement and/or fusion of lateral body folds. According to Sadler TW and Rasmussen SA [12], this is the most unifying theory to explain ventral body wall defects such as ectopia cordis, gastroschisis and bladder exstrophy.
In this case, authors speculated that a teratogen acted additionally on paraxial mesoderm, the cells which migrate into the lateral body folds to form rib cartilages and muscles of the limbs and body wall thus explaining the associated lateral thoracic wall defect in the form of thoracoschisis. However, it is intimidating to know why a teratogen act on two different developmental blocks and why only on the right thoracic paraxial mesodermal cells.
Therefore, this case was presented due to unusual type of body wall defect in two different regions of the body i.e., thorax and abdomen- one in midline and the other lateral.
There are a few more points in this case that we would like to highlight. The antenatal diagnosis of meningomyelocele was incorrect highlighting the importance of doing fetal autopsies. The maternal age was 19 years. Notably the only epidemiologic feature found consistent with cases of gastroschisis is young maternal age [13]. The horizontal position of the stomach noted in this case has been proposed as a marker for diaphragmatic hernia on antenatal USG scan [14]. In the absence of any report of the familial occurrence of such case, we considered the malformation to be a sporadic event and counseled the parents for a low probability of recurrence.
Conclusion(s)
This case of fetal autopsy had two well-separated ventral body wall defects which help in understanding of the embryological basis of body wall defects. The Body Wall hypothesis proposing a primary teratogenic effect on the mesenchyme of the lateral plate mesoderm is considered to be the most satisfactory explanation for majority of the ventral body wall defects.
ASD: Anterior septal defect; PDA: Patent ductus arteriosus; VSD: Ventral septal defect; B/L: Bilateral
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes (from parents)
For any images presented appropriate consent has been obtained from the subjects. Yes (from parents)
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Aug 24, 2020
Manual Googling: Aug 25, 2020
iThenticate Software: Sep 19, 2020 (13%)
[1]. Karaman I, Karaman A, Erdoğan D, Cavuşoğlu YH, Ozgüner IF, The first male with thoracoschisis: Case report and review of the literatureJ Pediatr Surg 2011 46(11):2181-83.10.1016/j.jpedsurg.2011.08.01622075354 [Google Scholar] [CrossRef] [PubMed]
[2]. Ertan G, Sinzig M, Tekes A, Huisman TA, Congenital Intercostal Liver Herniation: Report on two NeonatesEur J Pediatr Surg 2010 20(3):196-98.10.1055/s-0029-123773319882504 [Google Scholar] [CrossRef] [PubMed]
[3]. Bhattacharyya NC, Gogoi M, Deuri PK, Thoracoschisis with limb agenesisJ Indian Assoc Pediatr Surg 2012 17(2):78-79.10.4103/0971-9261.9397222529555 [Google Scholar] [CrossRef] [PubMed]
[4]. Seleim HM, ElFiky MMA, Fares AE, Elbarbary MM, Isolated Thoracoschisis: Case Report and Review of LiteratureEuropean J Pediatr Surg Rep 2015 3(1):40-42. [Google Scholar]
[5]. Davies MRQ, Rode H, Cywes S, “Thoracoschisis” associated with an ipsilateral distal phocomelia and an anterolateral diaphragmatic hernia-a case reportJ Pediatr Surg 1977 12(5):755-57.10.1016/0022-3468(77)90413-4 [Google Scholar] [CrossRef]
[6]. Bamforth JS, Fabian C, Machin G, Honore L, Poland anomaly with a limb body wall disruption defect: Case report and reviewAm J Med Genet 1992 43(5):780-84.10.1002/ajmg.13204305041642261 [Google Scholar] [CrossRef] [PubMed]
[7]. Derbent M, Balcý S, Thoracoschisis associated with diaphragmatic hernia in a 31-week-old stillbirthTurk J Pediatr 2001 43(3):269-71. [Google Scholar]
[8]. Biri A, Korucuoglu Ü, Turp A, Karaoguz M, Himmetoglu O, Balci S, A new syndrome with prenatally diagnosed thoracoschisis, hiatal hernia and extremities agenesis: case reportGenet Couns 2006 17(2):161-65. [Google Scholar]
[9]. Davies BR, Duran M, The confused identity of cantrell’s pentad: ectopia cordis is related either to thoracoschisis or to a diaphragmatic hernia with an omphalocelePediatr Pathol Mol Med 2003 22(5):383-90.10.1080/pdp.22.5.383.390 [Google Scholar] [CrossRef]
[10]. Hartwig NG, Vermeij-Keers C, De Vries HE, Kagie M, Kragt H, Limb body wall malformation complex: An embryologic aetiology?Hum Pathol 1989 20(11):1071-77.10.1016/0046-8177(89)90225-6 [Google Scholar] [CrossRef]
[11]. Duhamel B, Embryology of exomphalos and allied malformationsArch Dis Child 1963 38(198):142-47.10.1136/adc.38.198.14221032411 [Google Scholar] [CrossRef] [PubMed]
[12]. Sadler TW, Rasmussen SA, Examining the evidence for vascular pathogenesis of selected birth defectsAm J Med Genet Part A 2010 152A(10):2426-36.10.1002/ajmg.a.3363620815034 [Google Scholar] [CrossRef] [PubMed]
[13]. Rasmussen SA, Frías JL, Non-genetic risk factors for gastroschisisAm J Med Genet Part C 2008 148C(3):199-212.10.1002/ajmg.c.3017518655102 [Google Scholar] [CrossRef] [PubMed]
[14]. Conturso R, Giorgetta F, Bellussi F, Youssef A, Tenore A, Pilu G, Horizontal stomach: A new sonographic clue to the antenatal diagnosis of right-sided congenital diaphragmatic herniaUltrasound Obstet Gynecol 2013 41(3):340-41.10.1002/uog.1228322903526 [Google Scholar] [CrossRef] [PubMed]