All efforts to save the natural teeth should be made during restoration to achieve optimum functionality and aesthetics. Tooth loss is associated with appetite loss and loss of nutritional values. Thus, rehabilitating complete or partial edentulous conditions contributes to improvement in the functioning of the masticatory system. In the latter case of partially dentate condition, the natural teeth present preserve the residual ridges. Extraction of teeth causes alveolar ridge resorption. Poor foundation or ridge form donot provide support for the denture bases which is the factor of utmost consideration for stabilisation of the denture bases. In these instances, use of the telescopic dentures may be indicated. A telescopic denture retains and preserves the natural teeth beneath it. Every dentist aims at preserving the natural and restoring the lost. Preservation of the remaining teeth in turn preserves the natural proprioception mechanism, was thus followed and applied in this case report in which a 25-year-old female patient with diabetic history and on medication since past four years, presented with multiple missing teeth in December 2019. After thorough evaluation, the patient was treated by Marburg double crown system or synonymously termed as telescopic denture opposing the tooth supported overdenture. Follow-up and recall schedule was then explained and operator noted a satisfactory response from the patient. Consecutive follow-ups were maintained.
Double crown system, Telescopic denture, Tooth supported overdenture
Case Report
A moderately built 25-year-old female patient came to the Department of Prosthodontics in the month of December 2019 with the chief complaint of multiple missing teeth in both the arches and failed fixed dental prosthesis units which got dislodged and wanted to get the same rehabilitated. Teeth present were 16,14,12,21,24,26,34,36,46,47 with their respective clinical crown heights as mentioned in [Table/Fig-1]. On enquiry, past dental history revealed endodontic root canal treatment for all the abutment teeth present (16,14,12,21,24,26,34,36,46,47) followed by full mouth rehabilitation using fixed dental prosthesis, using 6 maxillary abutments (16,14,12,21,24,26) [Table/Fig-2], 4 mandibular abutments (34,36,46,47) and previous history of extraction of the remaining teeth due to poor periodontal status and mobility. On further enquiry, it was revealed that the patient was diagnosed with Type 2 Diabetes Mellitus 4 years ago when her HbA1C levels were 8% and was on medication, Tab. Metformin (500 mg twice a day) and Tab. Glimepiride (1 mg twice a day). At present, reports suggested of controlled diabetes with Fasting Blood Sugar (FBS) level 110 mg/dL and Post Prandial Blood Sugar (PPBS) level 160 mg/dL with HbA1C 6.8. On clinical evaluation, residual ridge was low and depressed.
Illustrates the clinical crown height with tooth number.
| Abutment | Clinical crown height | Probing pocket depth |
|---|
| 16 | 6 mm | 2 mm |
| 26 | 5.8 mm | 2.5 mm |
| 14 | 5.9 mm | 1.2 mm |
| 24 | 5.9 mm | 1.2 mm |
| 12 | 5 mm | 1.4 mm |
| 21 | 5 mm | 1.4 mm |
| 34 | 4.8 mm | 1.2 mm |
| 36 | 5 mm | 1.5 mm |
| 46 | 4.5 mm | 1.5 mm |
| 47 | 5 mm | 1.4 mm |
Preoperative photograph (a) when the patient reported with dislodged fixed dental prosthesis, (b) condition of the mouth with the prosthesis removed.

Proposed Treatment Plan
Informed consent was taken from the patient for the use of photographs for the purpose of case presentation and documentation. Diagnostic impressions were recorded using irreversible hydrocolloid and poured in dental stone. The casts were surveyed and areas of retention were identified in the maxillary anterior region.
Upper right first molar (16) with grade II mobility was indicated for extraction due to poor periodontal condition and complete healing of the socket was allowed for 1 month, approximately. As the patient was diabetic, the remaining teeth (14, 12, 21, 24, 26, 34, 36, 46, 47) were preserved which aided in prevention of further bone loss and guided in the determination of vertical dimensions. The periodontal conditions of the teeth present were acceptable for short coping cementation. The pocket depth of the remaining abutments has been mentioned in the [Table/Fig-1]. Due to the failed treatment of past fixed dental prosthesis and also poor economic conditions and unwillingness to any surgical intervention, the treatment option of implant supported prosthesis was ruled out. The only favourable treatment option was of tooth supported denture.
Patient was explained in detail about the various treatment modalities available with their pros and cons. On considering patient’s desire, compliance factor and the clinician’s opinions, it was decided to prosthodontically rehabilitate upper and lower arches with fixed removable prosthesis. As the weight of the cast metal prosthesis in comparison to the acrylic prosthesis is more and due to the gravitational factors acting on the denture, hence a tooth supported maxillary overdenture opposing Marburg denture in the mandibular arch were planned. Also, the retention and stability were compromised in the present case hence, overdenture was planned.
Procedure
The assessment of blood glucose levels was done before commencing the treatment.
The treatment phase included the following steps:
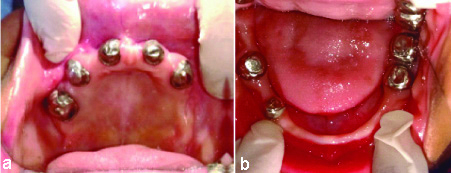
Mouth preparation: Tooth preparation was done for all the endodontically treated teeth with 6 degrees of taper, the cervical portions of the abutments were kept nearly parallel with convergence on the occlusal thirds for clearance fit for the overlaying framework of denture. More taper in the preparation should not be done as retention is compromised. Impressions were recorded using polyvinyl siloxane [Table/Fig-3]. Casts were poured in type IV Dental Stone for the metal coping fabrication made of Co-Cr alloy [Table/Fig-4]. The copings were fabricated and the inner coping crowns were cemented using Type IX Glass Ionomer cement onto the abutments [Table/Fig-5].
Final impressions after tooth preparation, maxillary and mandibular.
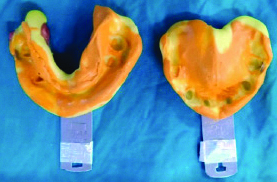
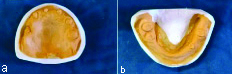
Cast fabrication for copings. (a) Maxillary (b) Mandibular
Intraoral (mirror images) picture with metal copings cemented. (a) Maxillary (b) Mandibular.
After the conventional procedure of border moulding the master cast was fabricated [Table/Fig-6].
Single step border moulding done with polyvinyl siloxane.

The mandibular master cast was surveyed for the fabrication of the frame work with the crowns that would precisely fit onto the inner copings without friction or wedging. The cast framework fit was verified in patient’s mouth. Minimal lateral and effortless gliding movements were permitted along the long axis of path of insertion for the fit of the framework.
Jaw relation was recorded on the lower framework opposing the temporary denture base of the maxillary arch for the tooth supported overdenture [Table/Fig-7]. Acrylic teeth shade selection was done and teeth arrangement was done followed by try in with evaluation of aesthetics, phonetics and Class 1 molar relation [Table/Fig-8] with horizontal overlap of 2 mm. Denture processing, finishing and polishing followed by insertion [Table/Fig-9a-c] and post-insertion instructions were given. Patient was explained about the recall schedule and hygiene maintenance after removal of the denture. The tissue surface and the coping surface should be cleaned as the removable prosthesis causes plaque accumulation on the metallic surface and also around the margins of the copings. Hygiene maintenance plays vital role in this prosthesis.
Orientation jaw relation recording using face bow.


The post-insertion intra-oral photograph of the patient in: a) right lateral; b) frontal; c) left lateral view.

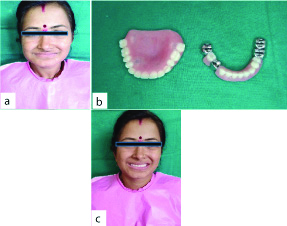
On follow-up after one week, the patient got well adapted to the dentures regarding its usage and maintenance. Preoperative photograph of the patient was compared and showed remarkable improvement in aesthetics as well as restored the phonetics and function [Table/Fig-10a,c]. Extraoral photographs of maxillary tooth supported overdenture and mandibular Marburg denture has been shown in [Table/Fig-10b].
a) Preoperative photograph; b) Extraoral photograph of Mandibular Marburg denture and Maxillary Overdenture; c) Postoperative extraoral photograph with prosthesis in place.
Discussion
The fundamental aspects in restoring facial aesthetics are mouth and teeth [1]. Systemic conditions majorly affect the outcome of any treatment modality and hence thorough investigation and medical history has to be carried out [2]. Patients with diabetes are more susceptible to periodontal disease than the general population; diabetes being the most prevalent systemic illness affects the treatment planning and needs special attention and techniques [2]. In the present case report, patient at the age of 25 years with a known history of diabetes mellitus post-extraction was advised to wait for 1 month for healing to occur. Preservation of the remaining natural teeth helps in preserving the proprioception mechanism. The extraction of all natural teeth results in the complete loss of tooth proprioception which has helped to program the masticatory system throughout a large portion of the patient’s life [3]. There are varied treatment modalities for partially missing teeth such as implant/tooth supported denture, full mouth extraction followed by complete denture and conventional overdenture [3]. Conventional overdenture was selected for the present case scenario. Selection of the treatment option is based on patient’s clinical condition, like denture bearing area, periodontal condition of the remaining natural teeth, compliance factor and durability [3]. On analysis of all the confounding factors, the implant supported dentures were ruled out due to poor bone support and delayed healing seen in diabetes [2]. Complete extraction was not advisable as the residual ridge needs to be preserved which might get compromised post-extraction leading to progression of bone loss [2]. Hence, the treatment plan formulated comprised of the tooth supported dentures. Telescopic dentures can be used in combination with other treatment option [4], like in this case, Marburg denture opposing the maxillary tooth supported overdenture was used. The Marburg double crown system in which natural teeth or implants can be used as abutments was first described by Lehmann and Gente where natural teeth or implants can be used as abutments. The principal objective of double crown used in removable partial denture cases is reduction of the detrimental occlusal forces acting axially [5]. This system provides cross arch and multiple abutment splinting for stabilisation. These resilient designs are advantageous for cases with weak or few abutments [5].
The present case was thoroughly examined and evaluated. The failed full mouth fixed dental prosthesis was ruled out primarily due to poor health of the periodontium, longevity and past experience with the patient. Therefore, the decision of rehabilitation with the tooth mucosa supported removable partial denture therapy was finalised, as selection is based on the nature of the support of denture-bearing areas and stability of the remaining natural dentition [6-8].
For maxillary arch, cementation of short copings was done, which aided in frictional retention between the denture and the abutments [9]. A case report by Prakash V et al., also described a case with similar findings of few abutment teeth present with presence of systemic conditions which was treated with Marburg denture for the maxillary arch [10]. Patient compliance plays a major role. The follow-ups of the patient are frequent for evaluation of the abutment and condition of the denture and hygiene [11]. Patients who do not follow the schedule of treatment explained to them can be labelled as non-adherent. Non-adherence is a serious problem in both developed and developing countries [11]. The metal framework prosthesis which is fabricated by conventional casting procedures can be fabricated by the rapid prototyping or direct metal laser sintering process. The designing of the prosthesis can be done virtually on the software of Haptic interface and can be manufactured by 3-D printing [12].
Conclusion(s)
Telescopic prostheses are widely used in clinical practice and also have varied types of designs and possibilities depending on the prognosis of the remaining teeth, age and patient compliance. The main goal of the case was to preserve the residual ridge and prevent further bone loss. On follow-up, the patient was satisfied with the denture and its functioning. These dentures can be indicated for patients with few abutment teeth present and poor bony conditions along with systemic illnesses where the abutments can be treated periodontally or endodontically and can be preserved. Telescopic crowns are used as removable retainers that rest on the natural abutments and do not require precision attachment systems or clasp assemblies. In this case, the patient was young enough and had clinical findings of partially dentate arch comprising of abutments of poor prognosis. The aesthetics and functionality were restored to an extent acceptable to the patient.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: May 11, 2020
Manual Googling: Aug 08, 2020
iThenticate Software: Sep 19, 2020 (5%)
[1]. Pisulkar SK, Agrawal R, Belkhode V, Nimonkar S, Borle A, Godbole SR, Perception of buccal corridor space on smile aesthetics among specialty dentist and laypersonJournal of International Society of Preventive & Community Dentistry 2019 9(5):499-504. [Google Scholar]
[2]. Wray L, The diabetic patient and dental treatment: An updateBritish Dent Journal 2011 211(5):209-15.10.1038/sj.bdj.2011.72421904352 [Google Scholar] [CrossRef] [PubMed]
[3]. Crum RJ, Loiselle RJ, Oral perception and proprioception: A review of the literature and its significance to prosthodonticsThe Journal of Prosthetic Dentistry 1972 28(2):215-30.10.1016/0022-3913(72)90141-2 [Google Scholar] [CrossRef]
[4]. Langer Y, Langer A, Tooth-supported telescopic prostheses in compromised dentitions: A clinical reportJournal of Prosthetic Dentistry 2000 84(2):129-32.10.1067/mpr.2000.10802610946327 [Google Scholar] [CrossRef] [PubMed]
[5]. Ohkawa S, Okane H, Nagasawa T, Tsuru H, Changes in retention of various telescope crown assemblies over long-term useThe Journal of Prosthetic Dentistry 1990 64(2):153-58.10.1016/0022-3913(90)90170-H [Google Scholar] [CrossRef]
[6]. Wenz HJ, Lehmann KM, A telescopic crown concept for the restoration of the partially edentulous arch: The Marburg double crown systemInt J Prosthodont 1998 11(6):541-50. [Google Scholar]
[7]. Wenz HJ, Hertrampf K, Lehmann KM, Clinical longevity of removable partial dentures retained by telescopic crowns: Outcome of the double crown with clearance fitInt J Prosthodont 2001 14(3):207-13. [Google Scholar]
[8]. Widbom T, Löfquist L, Widbom C, Söderfeldt B, Kronström M, Tooth-supported telescopic crown-retained dentures: An up to 9-year retrospective clinical follow-up studyInternational Journal of Prosthodontics 2004 17(1):29-34. [Google Scholar]
[9]. Hakkoum MA, Wazir G, Telescopic dentureThe Open Dentistry Journal 2018 12:246-54.10.2174/187421060181201024629760817 [Google Scholar] [CrossRef] [PubMed]
[10]. Prakash V, Parkash H, Gupta R, Fixed removable prosthesis employing Marburg double crown systemThe Journal of Indian Prosthodontic Society 2008 8(1):59-62.10.4103/0972-4052.43258 [Google Scholar] [CrossRef]
[11]. Kalucha S, Mishra KK, Gedam SR, Noncompliance in psychosisJournal of Datta Meghe Institute of Medical Sciences University 2017 12(1):61-65.10.4103/jdmimsu.jdmimsu_28_17 [Google Scholar] [CrossRef]
[12]. Eggbeer D, Bibb R, Williams R, The computer-aided design and rapid prototyping fabrication of removable partial denture frameworksProceedings of the Institution of Mechanical Engineers, Part H: Journal of Engineering in Medicine 2005 219(3):195-202.10.1243/095441105X937215934395 [Google Scholar] [CrossRef] [PubMed]