Polycystic Ovary Syndrome (PCOS) is a common gynaecological endocrine disorder in reproductive age women with 8.7 to 17.8% range of frequency [1]. Evidences suggest that phenotypes of PCOS vary, most commonly observed in post-pubertal period [2]. The variety of pathways are involved PCOS including steroid hormone synthesis pathway [3,4] insulin signaling pathway [5] and gonadotropin hormonal pathways [6]. Further due to the lack of a common link we find a multifactorial nature and heterogeneity of the syndrome [7]. The most important diagnostic features of PCOS are polycystic ovaries, chronic anovulation, hyperandrogenism and gonadotropin abnormalities [8]. Numerous studies now explain that pathogenesis of this syndrome is disturbance in hypothalamic-pituitary axis, resulting in elevated level of Luteinising Hormone (LH) and normal/low Follicle Stimulating Hormone (FSH) [9]. A study shows that PCOS phenotypes show differential LH/FSH ratio and on the basis of these differences, these were divided into different subgroups [10]. Hyperandrogenism, a condition of excessive androgen hormone production in the body. It’s usually indicated by acne, hirsutism (excessive growth of dark/coarse hair in a male-like pattern) and frontal alopecia (slowly progressive hair loss). Androgen Excess-PCOS (AE-PCOS) Society Task Force report [11] said that PCOS must be considered as a disorder of excess androgen or hyperandrogenism [7,12]. But there are a number of genetic and environmental factors, which influences its pathophysiology and manifestations [13]. Recent studies showed that PCOS women show impaired glucose tolerance and has a higher risk to develop Type 2 Diabetes Mellitus (T2DM) [13,14]. Now insulin-sensitising drugs (e.g., metformin) are showing positive responses in PCOS women in the way of improving metabolic, ovarian and androgen levels [15]. For PCOS androgen excess is the main feature, and so it is important to know the complete pathway of androgen synthesis. Cholesterol is the main precursor for prognenolone being converted to steroid hormones with series of enzymatic reactions [7,16]. In the ovary, LH-stimulated thecal cells form androgen by the expression of cytochrome P450c17 gene, with the synthesis of dehydroepiandrosterone (DHEA) and androstenedione [7,17]. These precursors get converted to oestrogens, the female reproductive hormone by granulose cells by the enzyme P450aromatase (CYP19A1) [18]. Ovaries also secrete androgens directly in blood circulation in the form of androstenedione and testosterone. Ovarian androgens does not affect LH production significantly, so free testosterone or androstenedione does not reduce ovarian production of androgens in women. The CYP19, aromatase gene is localised at chromosome 15q21.1, which is a key enzyme for oestrogen biosynthesis [7]. Any variation in CYP19 gene can affect steroidogenesis in the ovary and adrenal glands and it may result in affected steroid-related phenotypes. These studies indicate that SNPs in CYP19 may change the activity of aromatase, and thus may lead to PCOS [17]. In this study, characteristic features of PCOS (Economic & Marital status, Menstrual cycle regularity, parity, BMI, AAM, sugar levels, hormone profiles etc.,) its frequency in different age groups and whether aromatase gene polymorphism (SNP rs2470152) is associated with susceptibility to PCOS were studied by designing an experiment.
Materials and Methods
This was a pilot study where, control and PCOS samples were collected from Sir Sunderlal Hospital, Banaras Hindu University, Varanasi, Uttar Pradesh, India between January 2018-2019. It was a small study for testing hospital data collection, analysing sample strategies and techniques, potential problem areas, deficiencies faced and protocols can be involved prior to its complete study including a larger population size data. Here a total of 300 subjects were included in this study where 180 were control (Non-PCOS) and 120 were PCOS. Here, women of the control group visited the hospital for some reasons (e.g., tubal factor infertility or male infertility, they were having parity ≤2 or >2. While PCOS patients were diagnosed and included in the study, based on the 2003 Rotterdam Criteria [19]. Ethical clearance was obtained from the Institutional Ethical Committee prior to starting the study (Reference no: ECR/526/Inst/UP/2014 Dt.31.1.14). Before taking the blood samples, subjects were asked to fill the consent form, along with a proforma that includes patient’s history and questions related to the disease. Authors used validated questionnaire on the basis of revised 2003 Rotterdam criteria of PCOS [20,21]. It was having the details of patient-name, age, sex, economic and marital status, menstruation cycle, parity (total number of children), Body Mass Index (BMI), Age At Menarche (AAM), hormone profiles, sugar (Fasting and post-prandial) and about having any previous disease or not. Single Nucleotide Polymorphism was studied for aromatase gene (CYP19) by Polymerase Chain Reaction-Restriction Fragment Length Polymorphism (PCR-RFLP) method. Here GAPDH, a housekeeping gene which catalyses the sixth step of glycolysis (a process in which glucose is converted to pyruvate) was used as a reference gene in comparison of any gene expression. The expression of GAPDH in DNA samples tells that collected blood samples/DNA samples are viable for further evaluation.
Inclusion criteria of control group: The control group was eastern Uttar Pradesh women that had a healthy medical examination, in same age group to the case group.
Exclusion criteria of control group: The control group had received hormone therapy, possessed heart, lung, liver, kidney, and/or other organ dysfunction previously, had lived in north-east region less than 10 years and were at gestation or at breastfeeding period.
Inclusion criteria of case group: The patient group diagnosed for PCOS, without endocrine disease or radiation, and/or chemical/oral contraceptives therapy, for three months prior to admission, had no other disease history or mental disease.
Exclusion criteria of case group: The subjects who had received hormonal therapy prior to admission, had severe heart, lung, liver, kidney, and/or other organ dysfunction and had lived in north-east Uttar Pradesh for less than 10 years.
DNA and Serum Isolation
Blood samples were taken from median cubital vein of subjects between 8 to 9 am and collected in vials. DNA was isolated from phenol-chloroform method. For serum, blood was kept at room temperature for 30-60 minutes (for coagulation) and then centrifuged at 3000 rpm for 10 minutes at 4°C. Serum was isolated and stored at -80°C for hormone profiling.
Serum Profiling of Hormones
Steroid extraction from plasma and tissues were described previously [22]. From the collected serum, LH (LH, Lot No-LHG4061), Estradiol (E2, Lot no-42K039-3), Testosterone (T, Lot no-4510A) and Interleukin 6 (IL-6, Lot no-IL06001) levels were estimated by Enzyme Linked Immunosorbent Assay (ELISA), following the manufacturer’s protocol [22]. LH, E2, T and IL-6 kits were used for the measurement of concentration of hormones in serum and its absorbance were measured at using iMarkTM Microplate Absorbance Reader (BioRad, USA) and the concentration was expressed as ng/mL or ng/g. The intra-assay coefficients of variance for LH, E2, T and IL-6 were found to be ≤8.7%, ≤9.3%, ≤7%, ≤9.4%, respectively. The FSH, Triiodothyronine (T3), Tetraiodothyronine (T4) and Thyroid Stimulating Hormone (TSH) levels were noted down from questionnaire filled by the patients, complete charting were done, evaluated and then further compared with control.
Primer Designing for GAPDH and Aromatase Gene (CYP19)
Primers were designed by PRIMER 3 tool and these are as follows [23]:
GAPDH forward primer 5’CCATGGAGAAGGCTGGGG 3’
Reverse primer 3’ CAAAGTTGTCATGGATGACC 5’
CYP19 forward primer 5’ CTGCCTTTGAGGAGCTTA 3’
Reverse primer 3’ CTTCTCTGGCTTTCCCCTCT 5’
Polymerase Chain Reaction
PCR was performed using 0.5U of Taq DNA polymerase (Thermus aquatics), 2X Buffer, 10 mM deoxynucleotide triphophatase, 10 pmol of each primer, 100 ng genomic DNA, 2.5 mM MgCl2 in total volume of 25 μL GAPDH gene was amplified by 30 cycles of denaturation (50s at 94°C), primer annealing (1 min at 58°C) and extension (1 min at 72°C) in PCR cycler. Amplification was checked by running 5 μL of the PCR product on 2% agarose gel in 1X TAE buffer. Similarly, PCR reaction was performed for aromatase gene, with annealing temperature of 58°C [24].
Genotyping
Genotyping of SNP (-1562C/T) CYP19 gene was done by PCR-RFLP. Genomic DNA was extracted from peripheral blood of 100 patients (with 46XX karyotype) and 200 healthy controls using a standard salting-out procedure. PCR amplification of the -1562C/T mutation region in the aromatase gene was performed using primers (forward: 5’-CTGCCTTTGAGGAGCTTA-3’; reverse: 5’CTTCTCTGGCTTTCCCCTCT-3’). The PCR condition was 30 cycles at 94°C for 1 minute, 58°C for one minute and 72°C for one minute. For RFLP analysis, the 278-bp fragment was restricted with HPY CH4 IV (restriction enzyme) at 37°C for overnight. If there was a T→C transition, the fragment generated two restriction products of 179 and 99 bp. Thus, homozygous wild type phenotype (TT) shows a single thick band of 278 bp, heterozygous (TC) 2-bands of 179 and 99 bp, while homozygous recessive (CC) shows a single band of 99 bp size [25].
Statistical Analysis
Statistical analyses were performed using the Graphpad Prism software, version 5.0. The data was presented as Mean±SD. Student’s t-test was used to compare the mean for the two independent groups. Two-tailed p-values less than 0.05 were considered statistically significant. Allele and genotype distribution among groups were evaluated using the chi-squared test or Fisher’s-Exact test. The difference in frequencies between the case and control groups was analysed for statistical significance at the 95% Confidence Interval (CI) using the chi-square test. Odds Ratios (OR) were calculated and reported within the 95% confidence limits. A p-value <0.05 was considered as significant in all the analyses.
Results
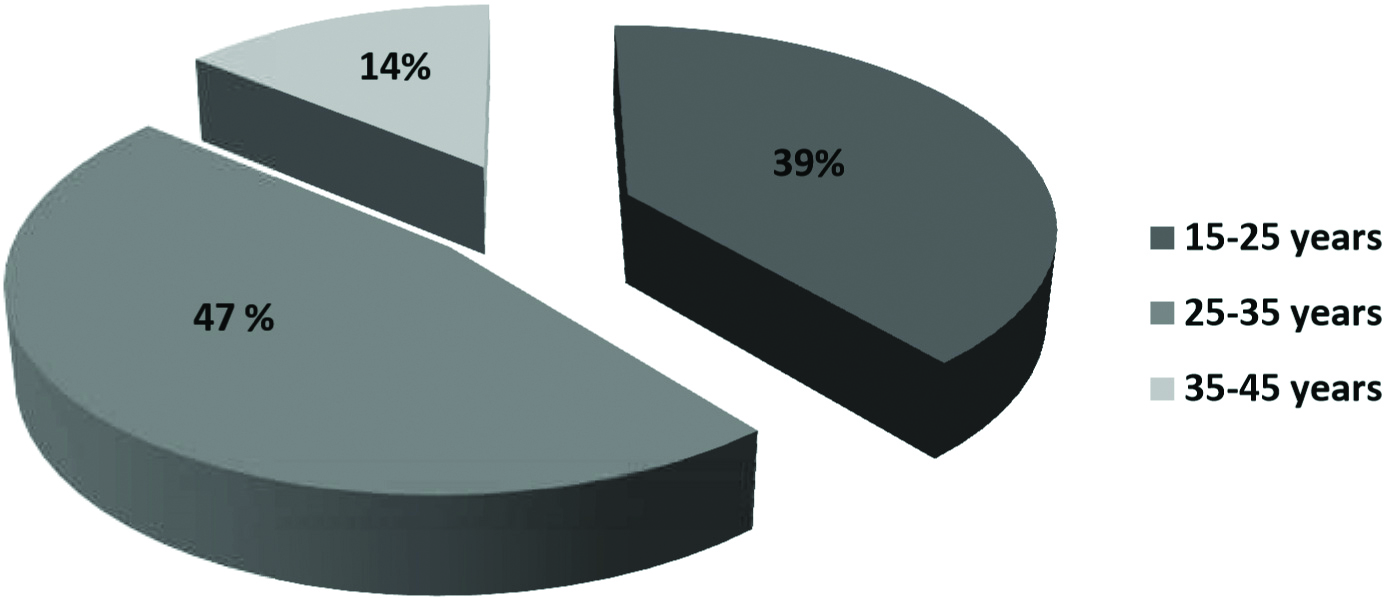
Total 300 samples (120 cases and 180 controls) were collected and evaluated. Results were showing that the point prevalence of PCOS (N=120) in this studied population was having a higher frequency in the age group of 25-35 years (47%) [Table/Fig-1]. Survey details of control and PCOS patients were charted and percentages of different age group patients were calculated. The included subjects in this study whether PCOS or non-PCOS, all belonged to lower, middle and higher class and there was not any association of occurrence of PCOS with their economic status. All the control (non-PCOS) subjects were married as they have visited the hospital because of tubal factor or male related infertility, but the PCOS subjects were mostly including unmarried girls at the time of their diagnosis who have visited the hospital because of their menstrual irregularities but 25% of them were married and diagnosed to have PCOS later. The marital status and menstrual irregularities in PCOS subjects showed significant values (p-value <0.001) as the diagnosis has been done earlier mostly in the puberty because of menstrual irregularities in respect to control. The non-PCOS and PCOS subjects have parity ≤2 or >2 without showing any significant association with PCOS [Table/Fig-2].
Percentage of women of different age groups suffering with PCOS.
Socio Demographic characteristics of the study subjects (N=300).
| Sl. No | Factors | PCOS (case) (N=120) | Non-PCOS (control) (N=180) | p-value |
|---|
| 1. | Economic status | Low | 30 (25.0%) | 40 (22.2%) | 0.148 |
| Middle | 50 (41.7%) | 60 (33.3%) |
| High | 40 (33.3%) | 80 (44.4%) |
| 2. | Marital status | Unmarried | 90 (75.0%) | 0 (0.0%) | <0.001*** |
| Married | 30 (25.0%) | 180 (100%) |
| 3. | Menstrual cycle | Regular | 22 (18.3%) | 180 (100%) | <0.001*** |
| Irregular | 98 (81.7%) | 0 (0.0%) |
| 4. | Parity | <2 | 62 (51.7%) | 88 (48.9%) | 0.637 |
| ≥2 | 58 (48.3%) | 92 (51.1%) |
PCOS: Polycystic ovary syndrome; N=Total number of subjects; p>0.05; * p<0.05; ** p<0.01; ***p<0.001; Chi-square test or Fisher’s exact test was used to study the significance of difference between proportions. Two-tailed p-values less than 0.05 were considered statistically significant
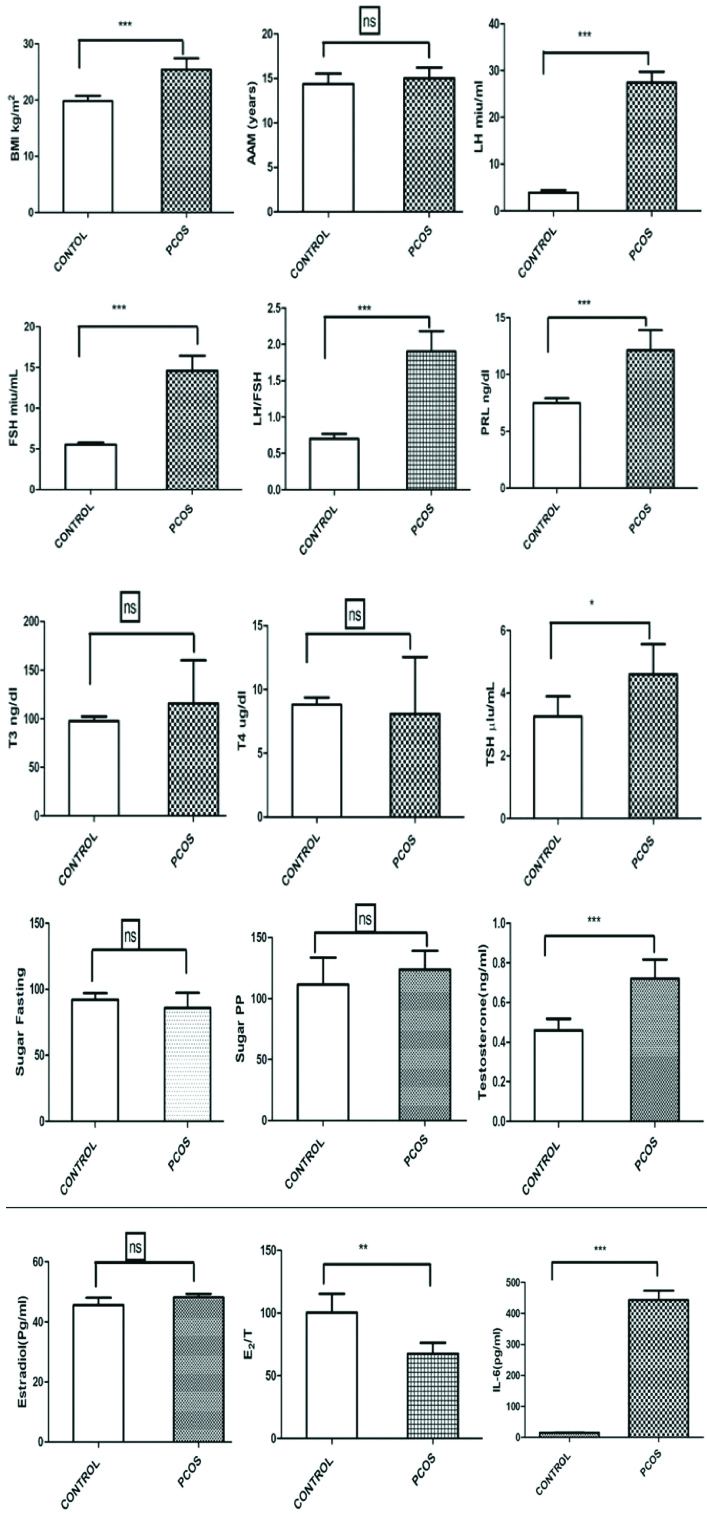
All the non-PCOS subjects were having normal ovulatory and menstrual cycle. They did not suffer with hirsutism (male-like hair-patterns), obesity or insulin resistant or with any other disease. While the PCOS patients were having ovulatory and menstrual irregularities, features of hirsutism, all together falling into the 2003 Rotterdam criteria of PCOS diagnosis. Patients of different ages were divided into 3-different age groups. BMI, AAM and hormone profiling were evaluated from the chartings. From all the patients and control, blood samples were collected on 3rd to 5th day of their menstruation in morning time (8 to 10am) having a overnight fast of 12 hours. All the samples were further processed for DNA and serum, then hormone profiling and SNP analysis were done. The variables BMI, LH, FSH, LH/FSH ratio, PRL, Testosterone, E2/T ratio and IL-6 were significantly higher (p=0.005) in PCOS subjects than those of control group. While findings AAM, T3, T4, Sugar fasting and PP, E2 of PCOS were not found significant (p>0.05) as compared to the same parameters of the control group subjects [Table/Fig-3].
Difference in characteristics of PCOS patients and control (N=300).
| Sl. No | Factors/hormones | PCOS (N=120) | Control (N=180) |
|---|
| 1. | BMI (Kg/m2) | 25.44±2.00 | 19.82±0.94*** |
| 2. | AAM (years) | 15.00±1.22 | 14.4±1.14 |
| 3. | LH (miu/mL) | 24.45±2.31 | 3.87±0.53*** |
| 4. | FSH (miu/mL) | 14.59±1.84 | 5.50±0.27*** |
| 5. | LH/FSH | 1.90±0.27 | 0.70±0.06*** |
| 6. | PRL (ng/dL) | 12.14±1.75 | 7.49±0.41*** |
| 7. | T3 (ng/dL) | 115.72±44.33 | 97.53±4.61 |
| 8. | T4 (Ug/dL) | 8.08±4.45 | 8.80±0.56 |
| 9. | TSH (μlu/mL) | 4.60±0.95 | 3.26±0.63* |
| 10. | Sugar (fasing) | 85.86±11.50 | 92.20±4.91 |
| 11. | Sugar (PP) | 123.8±15.32 | 111.4±22.28 |
| 12. | Estradiol E2 | 48.15±1.20 | 45.56±2.52 |
| 13. | Testosterone | 0.72±0.09 | 0.46±0.05*** |
| 14. | E2/T ratio | 100.5±15.02 | 67.68±8.60** |
| 15. | IL-6 | 443.6±30.13 | 15.34±0.69*** |
PCOS: Polycystic ovary syndrome; N: Total number of subjects; p>0.05, *p<0.05, **p<0.01, ***p<0.001
The significant difference in hormone levels of PCOS patients with respect to control where, ns=not significant, p>0.05, *p<0.05, **p<0.01, ***p<0.001 [Table/Fig-4].
Hormone levels in serum of control and PCOS patients.
ns: not significant, p>0.05, *p<0.05, **p<0.01, ***p<0.001
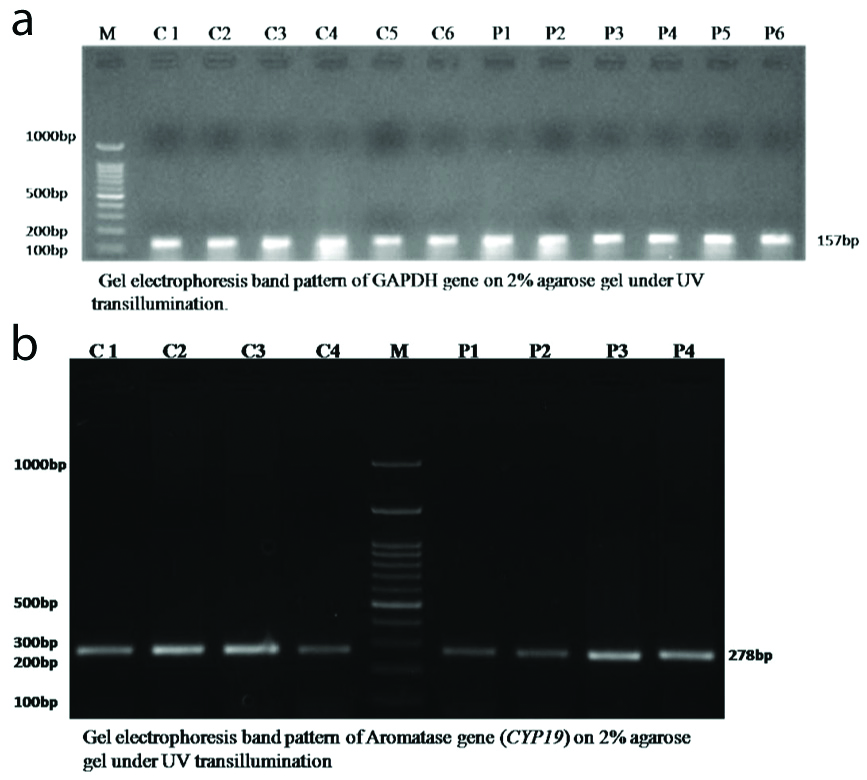
[Table/Fig-5a,b] showed a band of 157 base pair in all the DNA samples of control and PCOS, showing that GAPDH gene is equally expressed in all the samples. Similarly, the gel picture-5(B) is also showing an equally expressed band of 278 base pair in DNA samples of both control and PCOS, that tells aromatase gene is also equally expressed in all samples.
a) Lane M is 100bp ladder, Lane 2-7 (C1-C6) are control and lane 8-13 (P1-P6) are PCOS samples. Gel picture is showing that GAPDH gene is expressed in all the samples; b) Lane 1-4 (C1-C4) is control, Lane M is 100 bp ladder and lane 6-9 (P1-P4) is case samples.
GAPDH: Glyceraldehyde 3-phosphate dehydrogenase, PCOS: Polycystic ovary syndrome
The samples having wild type genotype (single band of 278 base pair size) means they have 2 similar copy of the aromatase gene and these are equally expressed producing sufficient amount of aromatase enzyme. While heterozygote (3 bands of 278, 179 and 99 base pair size) have one normal and other mutant aromatase gene copy, producing insufficient amount of aromatase enzyme as both copies of gene are not equally expressed [Table/Fig-6].
Restriction enzyme HpyCH4IV digestion of CYP19 gene mapping. Lanes on the agarose gel are denoted: lane L1=Marker (M), lanes L2-L6 control (C) and lane L7-L10 PCOS (E) samples. Lane L1, L2, L3, L10= heterozygote and Lane L4, L6, E7, E8, E9= wild type.
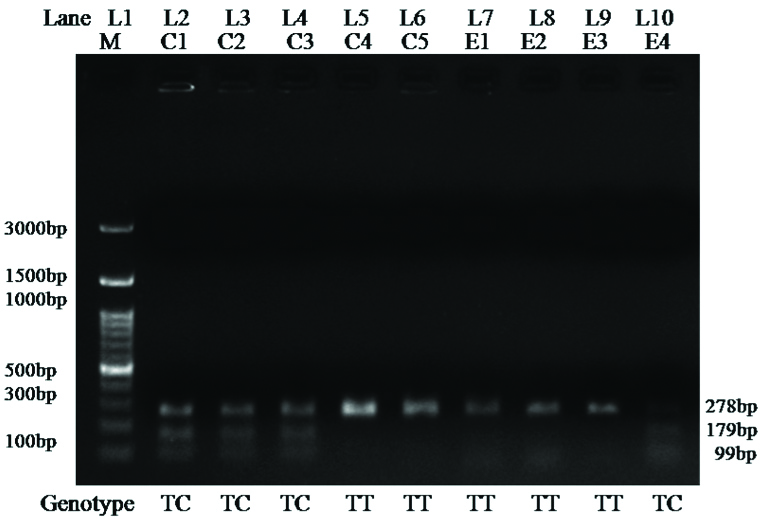
[Table/Fig-7] showed that the genotypic distributions (TC and TT) in women with PCOS (0.633 and 0.300) was differ from that of the controls (0.600 and 0.333, but genotype CC in women with PCOS (0.066) was similar to that in control (0.066) (p=0.8267). The rs2470152 (T, C) allele frequency in PCOS patients (0.617, 0.382) was not similar to that in controls (0.633, 0.366) (p=0.7699).
The frequency distribution of CYP19rs2470152 in women of PCOS and control.
| rs2470152 | Alleles N (%) | | p-valuea | Genotype N (%) | | | p-valueb |
|---|
| T | C | 0.7699 | TT | TC | CC | 0.8267 |
| Control | 114 (0.633) | 66 (0.366) | 60 (0.333) | 108 (0.600) | 12 (0.066) |
| PCOS | 74 (0.617) | 46 (0.382) | 36 (0.300) | 76 (0.633) | 8 (0.066) |
a: Based on the allele frequencies vs. control; b: Based on the genotype frequencies vs. control
Discussion
PCOS is a common reproductive endocrinological disorder among women of fertile age and if any alteration in reproductive hormones occurs, it may lead to PCOS phenotypes. Here, the study results showed that the highest percentage of women belonged to normal middle class. No association was found between occurrence of PCOS with their economic status. The control group included all married women with parity number >2-3 while frequency of unmarried girls was high in PCOS diagnosed subjects. As the initial symptoms included the irregular menstrual cycle and because of it the women were advised for PCOS diagnosis.
In this study, it was found that the women of 25-35 year age group in eastern Uttar Pradesh population were suffering with PCOS. The age may be a factor for the occurrence of the disease, but in this study, it was found that most of the women of reproductive age (25-35 years) suffer from PCOS having a mean BMI value of 25.44±2.00 (p<0.001) while AAM is not correlated with it. Studies showed that for normal reproductive health of women, a number of steroid hormones are involved and cholesterol is the main precursor for series of enzymatic reactions [7,16]. It also includes thyroid, the regulatory hormone for all the precursor hormones. TSH synthesises thyroid and it further activates positively on synthesis of other reproductive hormones, leading to normal reproductive cycling. One of the studies showed that Insulin resistance and hyperinsulinemia is all related to intra-abdominal accumulation of fat leading to obesity [26]. Intra-abdominal fat tissues undergo lipolysis and releases Free Fatty Acids (FFAs) in the circulation, and produces several cytokines (IL-6, TNF-α, leptin, resistin etc.,) all involved in insulin resistance. Circulating FFAs accumulate in non-adipose tissues of the body and causes increased level of lipoproteins called as lipotoxicity [26]. A study showed that the higher level of IL-6 in PCOS may not be a characteristic feature for PCOS diagnosis but it can be useful as a biomarker for its diagnosis [27]. Further reproductive or endocrine hormones in PCOS suffering women were evaluated. Levels of LH, FSH, Prolactin hormone (PRL) and TSH were significantly associated with PCOS in the studied data set. While ratio of LH/FSH (p<0.001) was also highly associated with the disease. The level of T3 and T4 were not found significantly variable. The levels of fasting, post-prandial sugar and estradiol (E2) were not found associated with PCOS, but the E2/T ratio was significantly associated (P<0.036) with the disease. In this study, Testosterone and IL-6, the two important biomarkers were also found significantly associated with PCOS. There were difference in hormone levels in each and every patient of PCOS, but at the end these all were leading to PCOS phenotypes. So it can be concluded here that many aetiological factors with altered hormone profiles together leading to PCOS condition. Several SNPs in CYP19 gene have been reported to be associated with aromatase activity. A 684-sample study in CYP19 (rs2414096) reported that it is associated with PCOS and the A allele is positively associated with aromatase activity [28]. A large case-control study that involved 1,078 samples and found that the Arg214Cys variant of CYP19 (rs700519) is associated with PCOS. In an additional functional study, it was found that 293 embryonic kidney cells transfected with the Arg264Cys variant (minor T allele) resulted in increased conversion of androstenedione to oestrogen when compared to wild type (major C allele) construct [29]. In this study, no significant association of aromatase gene polymorphism was found with PCOS. It was found that, SNP rs2470152 in CYP19 was not a major aetiological factor for PCOS, but the heterozygous TC genotype may inhibit aromatase activity and thus results in hyperandrogenism, particularly in PCOS patients. As heterozygotes have both wild type and mutated genes of aromatase, and because of, it the level of aromatase will be less compared to normal. It’s known DHEA and androstenedione precursors get converted to oestrogens by the enzyme P450 aromatase (CYP19A1) [18], if there be less aromatase enzyme in the body, the less of precursors get converted to oestrogen leading to higher level of androgens also called as hyperandrogenism, a leading cause of PCOS.
Limitation(s)
This study does not include the separate study of genotypes with their hormone profiles as different PCOS suffering individual have different hormone profiling and the table is showing the average of all the data sets. As some hormone profiles fall in the PCOS criteria and some other are in normal range.
Conclusion(s)
Many factors are responsible for PCOS phenotypes. So in this study, more than one factor has been evaluated and related or associated to PCOS patients but still definitive conclusion is very difficult to draw from it. The economic status and parity has no association with PCOS. Further, the studies demonstrated that age, marital status, menstrual cycle irregularities and BMI can’t be used to confer causality but it may be possible scenarios to envision explaining for the disease. Even further data supports a high association of LH/FSH, PRL, TSH, E2/T and IL-6 with PCOS. It was concluded that aromatase gene polymorphism (SNP rs2470152) was not found associated with PCOS. The research studies till today tells that hyperandrogenism is the leading feature during PCOS but its complete pathway is still unknown. So, further we can elaborate the studies for the genes involved in the pathway for the cause of hyperandrogenism or other regulatory factors involved here.
PCOS: Polycystic ovary syndrome; N=Total number of subjects; p>0.05; * p<0.05; ** p<0.01; ***p<0.001; Chi-square test or Fisher’s exact test was used to study the significance of difference between proportions. Two-tailed p-values less than 0.05 were considered statistically significant
PCOS: Polycystic ovary syndrome; N: Total number of subjects; p>0.05, *p<0.05, **p<0.01, ***p<0.001
a: Based on the allele frequencies vs. control; b: Based on the genotype frequencies vs. control