Morel Lavallée lesions (ML lesions) are a rare degloving type of injury occurring after blunt trauma, usually in the peritrochanteric region and resulting into a progressive subcutaneous swelling. The current case series includes three patients with a history of trauma and development of rapidly increasing fluctuant soft tissue swelling during a time period of 18 months. Though these lesions are typically described in peritrochanteric region, two cases were encountered in the knee region. ML lesions were diagnosed precisely using Ultrasound (USG) and Magnetic Resonance Imaging (MRI) modalities and were managed accordingly. Classification of these lesions is paramount to enhance patient outcome and reduce complications.
Blunt trauma, Degloving injuries, Fluctuant swelling, Magnetic resonance imaging, Peritrochanteric, Seroma
Introduction
ML lesions are a rare degloving type of injury which usually occur after blunt trauma resulting into a progressive subcutaneous swelling [1,2]. These are classically located in the peritrochanteric region. USG is the initial investigation of choice, which is supplemented with MRI for further characterisation of the lesion.
Case Series
Case I
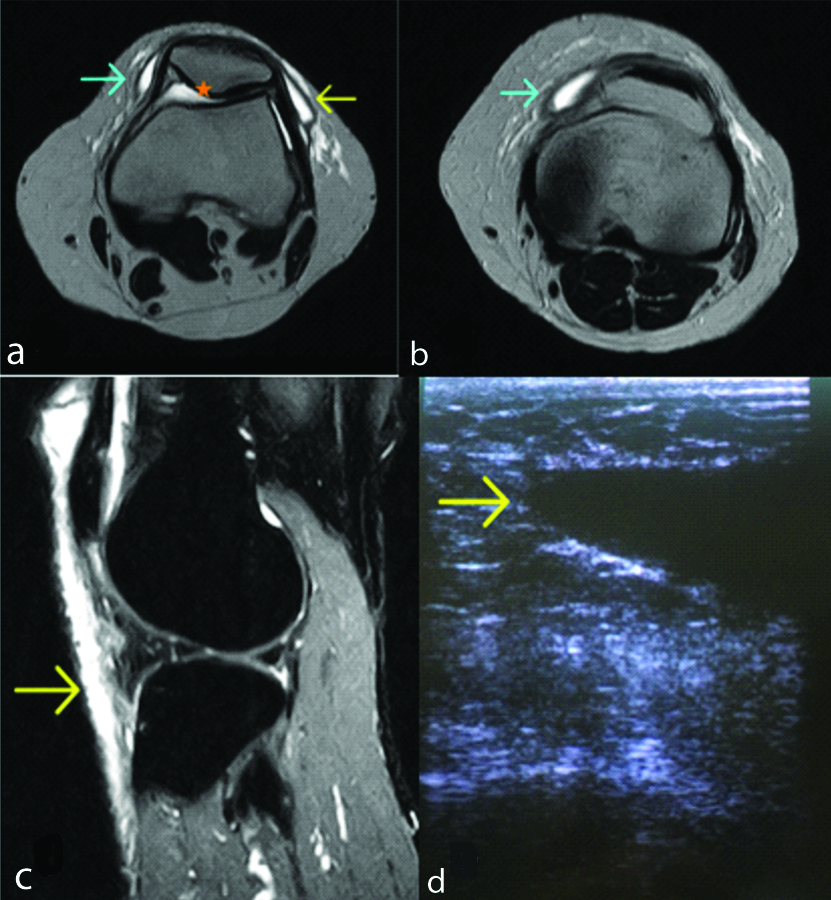
A 35-year-old male patient presented with a history of trauma one month ago. The patient had a fluctuant painful soft tissue swelling in the right knee region, which increased progressively. On local examination, there was discolouration of overlying intact skin. The patient had no history of fever or any other complain. Laboratory investigations were unremarkable and revealed increased Erythrocyte Sedimentation Rate (ESR) and leukocytosis. High frequency USG was done of the knee region which revealed a well-defined fusiform heterogeneously hypoechoic collection with septations and dependent debris between the skin and underlying muscles. No vascularity was seen in this collection on Colour Doppler. A suspicion of ML lesions was raised and MRI was done for further characterisation of this collection. On MRI, T1 hypointense and T2/STIR (Short-TI Inversion Recovery) hyperintense fluid collection was seen in the anterior deeper subcutaneous soft tissue planes of suprapatellar, prepatellar and superficial infrapatellar regions, largest pocket measuring ~46×11×35 mm [Table/Fig-1]. The fluid collection extended medially and laterally in the deeper subcutaneous soft tissue planes along the retinaculum. The fluid collection showed hyperintense signals on T2W and hypointense signals on T1WI. Mild right knee joint effusion was also noted. No ligamentous, meniscal or bony injury was identified. As the fluid pocket extended beyond the expected location of prepatellar and superficial infrapatellar bursa, diagnosis of ML lesions was made. According to the Mellado-Bencardino classification [3] of ML lesions, this injury corresponded to type I injuries. According to the grade of injury, it represents an acute injury and was managed conservatively by aspiration of the serosanguinous fluid and antibiotic therapy. Patient showed quick recovery with resolution of symptoms, after aspiration of the intralesional fluid. The patient was lost to follow-up.
Axial T2WI and Sagittal STIR image of right knee joint reveal: a) & b) T2 hyperintense fluid collection in medial (blue arrow) and lateral retinaculum (yellow arrow) with mild joint effusion (star); c) STIR hyperintense fluid collection in anterior deeper subcutaneous soft tissue planes of suprapatellar, prepatellar and superficial infrapatellar regions (yellow arrow); d) Grey scale USG image shows well-defined hypoechoic collection with distal tapering under the subcutaneous tissue (yellow arrow).
Case II
A 16-year-old adolescent male had a history of fall on his right side one week before. The patient had no complaint of pain or difficulty in walking but development of a boggy soft tissue swelling along the anterolateral aspect of right thigh was observed. His laboratory investigations showed increased leucocytes and ESR. High frequency USG was done which revealed well-defined avascular, predominantly anechoic fluid collection underneath the subcutaneous tissue in the peritrochanteric region. The underlying muscle fibers appeared intact. The patient was managed conservatively with USG-guided aspiration of the collection, which came out to be serosanguinous in nature. Approximately, 150 mL of fluid was aspirated from the site [Table/Fig-2].
a) High-frequency USG image shows well-defined subcutaneous collection (yellow arrow) with normal underlying muscle (star) in the peritrochanteric region of right hip; b) Serosanguinous fluid was aspirated from the site under USG guidance.
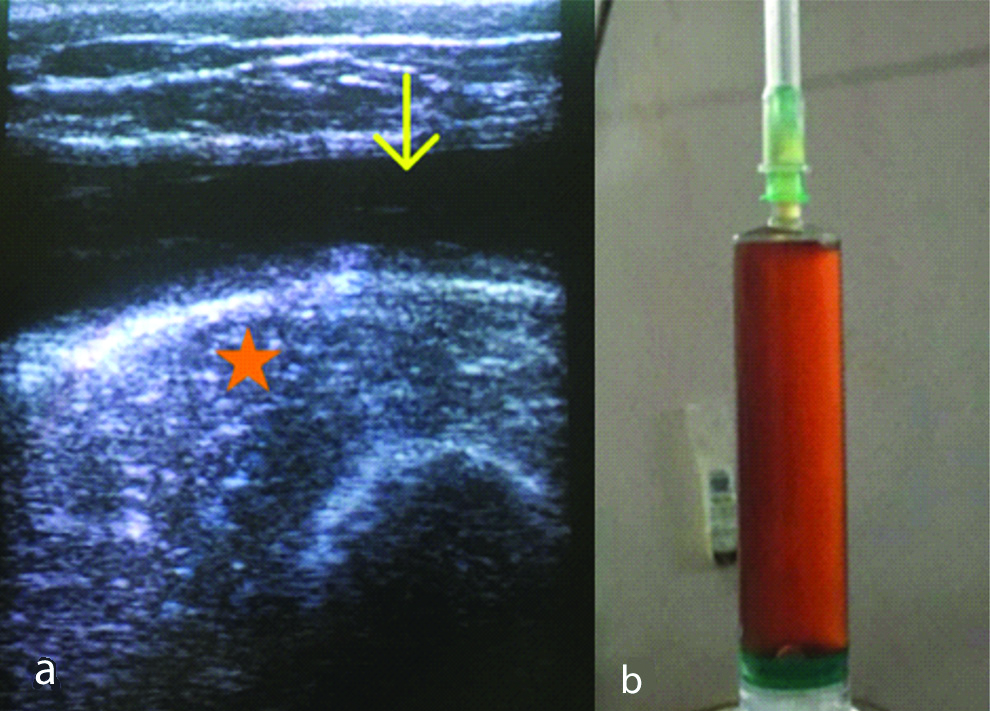
Diagnosis of ML lesion was made thereby. Near complete aspiration of fluid was followed by application of compression bandaging. The patient recovered well without recurrence of the lesion, in the follow-up period. The patient was followed for three months and didn’t show any sign of recurrence of the lesion.
Case III
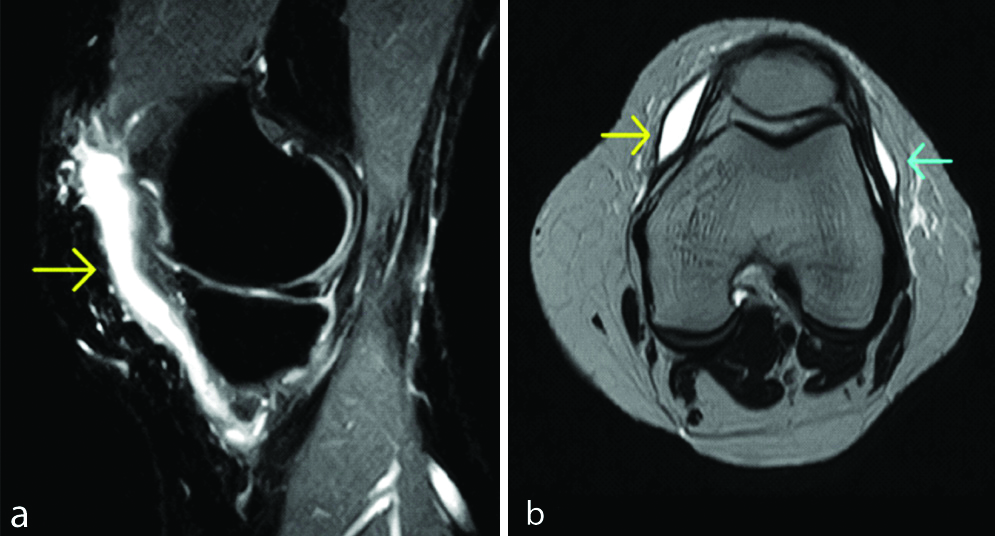
A 36-year-old female having a history of trauma two months back, presented with a painless consistent swelling in the left knee region. Laboratory investigations were normal. MRI knee was done for the same. MRI [Table/Fig-3] revealed small T1 hypointense and T2/STIR hyperintense fluid pockets overlying medial and lateral retinaculum, largest measuring ~27×16×9 mm in the left knee joint. T2 hypointense capsule lining was also noted in the lesion. No obvious meniscal or ligamentous injury was noted. The lesion was classified as type III injury and a radiological diagnosis of ML lesion was made after aspiration of haemolymphatic fluid from the swelling. Surgical exploration was advised. The patient could not be followed for complete resolution or persistence of the lesion.
Sagittal STIR (a) And axial T2W images; (b) Show well-defined hyperintense fluid pockets overlying medial and lateral retinaculum in the left knee region (arrows).
[Table/Fig-4] shows features and outcome of ML lesion of all three cases.
Describing various features and outcome of ML lesion cases.
| Case | Clinical features | Lab investigations | Therapy | Outcome |
|---|
| Case I | Soft-tissue swelling in right knee region with abrasion of overlying skin | Increased ESR and leucocytosis | USG-guided therapeutic aspiration | Could not be followed-up |
| Case II | Fluctuant soft-tissue swelling over the right peritrochanteric region | Increased ESR and leucocytosis | USG-guided therapeutic aspiration followed by compression bandaging and antibiotic therapy | Complete recovery |
| Case III | Painless stable swelling over left knee joint | Normal | Diagnostic aspiration of sero-sanguinous fluid | Immediate relief with reduction of swelling.Patient advised for further surgical management but was lost to follow-up. |
Discussion
ML lesions were first described by a French surgeon, Victor-Auguste-François-Morel Lavallée in 1848 [4]. ML lesions are a rare degloving type of injury which usually occurs after blunt trauma. ML lesions can also be sequelae of sports injury or post-liposuction procedure. The shearing traumatic force causes abrupt separation of skin and subcutaneous fat from underlying muscle fascia [3]. The potential space thereby, created is progressively filled with blood, fat and debris coming from torn vessels and lymphatics [4]. These are typically well-defined, oval or fusiform in shape seen extending along the fascial planes. There may be associated fracture of the underlying bone. ML lesions were typically described for peritrochanteric region but are also seen along the anterolateral aspect of thigh, peripelvic region, knee region, scapular and lumbar region and subcutaneous plane of anterior abdominal wall [1,4]. These degloving injuries are under-reported or misdiagnosed due to their non-specific presentation and close mimickers with comparable imaging features [1].
Patients can present within hours of injury to days and even months post-trauma [5]. In the current study, presentation time ranged from a week to two months. USG reveals presence of a well-defined anechoic to hypoechoic collection with fluid-fluid level or dependent debris between the subcutaneous plane and underlying muscles. The lesion may contain echogenic nodules along its walls, representing fat globules [3]. Underlying muscle usually appears normal. On Computed Tomography (CT), ML lesions are typically seen above the muscles, appearing hypodense with some fatty component and do not enhance. Capsule when present can show enhancement [3]. MRI accurately determines the size, extent and nature of the lesion. ML lesions are usually T1 hypointense and appear hyperintense on T2 and STIR images. Fat-fluid levels or scattered fat globules can also be seen.
Mellado-Bencardino in 2005, proposed a six-stage MRI-based classification for Morel Lavallée lesions (ML lesions) [6]:
Type I- Seroma appearing homogeneously hypointense on T1-Weighted Image (T1WI) and hyperintense collection on T2-Weighted Images (T2WI), without evidence of outer capsule formation.
Type II- Subacute haematoma appearing homogeneously hyperintense on both T1WI and T2WI due to the presence of methemoglobin.
Type III- Chronic organising haematomas appearing hypointense on T1WI and heterogeneously hypointense/isointense on T2WI with T2 hypointense capsule formation. On post-contrast sequences, may show capsular and internal enhancement secondary to neovascularisation and granulation tissue in the organising haematoma.
Type IV- Represents a closed laceration, with the absence of a capsule. It shows T1 hypointense and T2 hyperintense signals.
Type V- Demonstrates a small, rounded, pseudonodular appearance and has variable T1 and T2 signal intensities.
Type VI- Represents superimposed infection, with a thick enhancing capsule and can be associated with sinus tract.
MRI was done in two of the three cases and Mellado-Bencardino classification was applied. One case each of type I and type III ML lesion was found. Type III ML lesion showed T2 hypointense capsule on MRI.
ML lesions have been reported by various studies to be most frequently occurring in the peritrochanteric region [6,7], but in this series, knee region was more commonly affected. Early diagnosis and management are essential for better patient outcome and to ensure complete resolution of the lesion. These lesions may show spontaneous resolution or may get encapsulated and persist. ML lesions can also get infected with skin necrosis and formation of sinus tract upto the skin [4,7]. ML lesions along the medial aspect of knee joint can lead to exposure of underlying bone due to poor vascularity and lack of muscle attachments in this region [2].
Differential diagnosis includes a soft tissue haematoma, abscess, ruptured bursa, muscle tear with overlying haematoma, fat necrosis and prepatellar bursitis in knee region [2,3,8]. ML lesions are usually distal to joint but a ruptured bursa will appear in its typical location. Ruptured bursa will show similar appearance as that of type I ML lesion but in a different location [8]. Bursitis and haematoma can be differentiated from ML lesions based on their locations [8,9]. However, chronic haemorrhagic bursitis can resemble type III ML lesion. An abscess has a thick enhancing wall and shows central diffusion restriction. In longstanding cases, ML lesions can grow slowly and mimic a soft tissue neoplasm [9]. A soft tissue sarcoma will show marked homogenous post-contrast enhancement as compared to ML lesion [9].
Treatment of ML lesions is not specifically established and depends on the stage of the lesion when detected. It ranges from conservative management using compression bandage to USG-guided percutaneous aspiration, debridement or surgical removal of the fibrous capsule. Other treatment options include vacuum-assisted closure device and radical debridement with full-thickness skin grafting [10]. In case of associated bony injuries, internal or external fixation of the bone is also done along with NSAIDs and antibiotic therapy. If untreated, the lesion may continue to progress, get infected or remain persistent due to formation of thick fibrous capsule [8]. Also, the lesion can cause a cosmetic deformity in the particular area in the long run due to tissue necrosis.
Conclusion(s)
ML lesions are post-traumatic degloving type of injury in the subcutaneous plane with accumulation of haemolymphatic fluid in the potential space thereby created between the superficial and deep fascia. Though ML lesions are typically seen in the peritrochanteric region, development in the knee region is not rare. Due to its close mimickers this entity is often misdiagnosed and under-reported. USG and MRI are highly accurate in the diagnosis and characterisation of these lesions when combined with history of trauma. MRI clearly depicts presence of encapsulating fibrous tissue, if any. ML lesions can be managed conservatively or surgically depending on the stage of the lesion at presentation. If not diagnosed and managed properly they can persist and complicate. Therefore, these injuries need accurate and timely reporting. MRI is the modality of choice for diagnosis. Type I and II injuries can be managed conservatively by percutaneous aspiration of fluid under CT/USG guidance followed by compression bandaging and antibiotic therapy. Type III lesions and others with capsule lining often need to be managed surgically.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: May 28, 2020
Manual Googling: Jul 28, 2020
iThenticate Software: Sep 17, 2020 (9%)
[1]. McLean K, Popovic S, Morel-Lavallée lesion: AIRP best cases in radiologic-pathologic correlationRadiographics 2017 37(1):190-96.10.1148/rg.201716016928076017 [Google Scholar] [CrossRef] [PubMed]
[2]. Vassalou EE, Zibis AH, Raoulis VA, Tsifountoudis IP, Karantanas AH, Morel-Lavallée lesions of the knee: MRI findings compared with cadaveric study findingsAmerican Journal of Roentgenology 2018 210(5):W234-39.10.2214/AJR.17.1861429570368 [Google Scholar] [CrossRef] [PubMed]
[3]. Nair AV, Nazar PK, Sekhar R, Ramachandran PV, Moorthy S, Morel-Lavallée lesion: A closed degloving injury that requires real attentionThe Indian Journal of Radiology & Imaging 2014 24(3):28810.4103/0971-3026.13705325114393 [Google Scholar] [CrossRef] [PubMed]
[4]. Sharma BB, Sharma S, Ramchandran P, Magu NK, Aziz MR, Singh S, Morel-Lavalle lesion-radiological spectrumPlast Aesthet Res 2016 3:335-38.10.20517/2347-9264.2016.65 [Google Scholar] [CrossRef]
[5]. Gummalla KM, George M, Dutta R, Morel-Lavallee lesion: Case report of a rare extensive degloving soft tissue injuryUlus Travma Acil Cerrahi Derg 2014 20(1):63-65.10.5505/tjtes.2014.8840324639319 [Google Scholar] [CrossRef] [PubMed]
[6]. Mellado JM, Bencardino JT, Morel-Lavallée lesion: Review with emphasis on MR imagingMagnetic Resonance Imaging Clinics 2005 13(4):775-82.10.1016/j.mric.2005.08.00616275583 [Google Scholar] [CrossRef] [PubMed]
[7]. Padmanabhan E, Rudrappa RK, Bhavishya T, Rajakumar S, Selvakkalanjiyam S, Morel-Lavallee Lesion: Case report with review of literatureJournal of clinical and diagnostic research: JCDR 2017 11(7):TD0510.7860/JCDR/2017/25307.1018628893006 [Google Scholar] [CrossRef] [PubMed]
[8]. Myrick KM, Davis S, Morel-Lavallee injury a case studyClinical Case Reports 2018 6(6):103310.1002/ccr3.151829881558 [Google Scholar] [CrossRef] [PubMed]
[9]. De Coninck T, Vanhoenacker F, Verstraete K, Imaging features of Morel-Lavallée lesionsJournal of the Belgian Society of Radiology 2017 101(Suppl 2):01-08.10.5334/jbr-btr.140130498807 [Google Scholar] [CrossRef] [PubMed]
[10]. Latifi R, El-Hennawy H, El-Menyar A, Peralta R, Asim M, Consunji R, Al-Thani H, The therapeutic challenges of degloving soft-tissue injuriesJournal of Emergencies, Trauma, and Shock 2014 7(3):22810.4103/0974-2700.13687025114435 [Google Scholar] [CrossRef] [PubMed]