Case Report
A seven-year-old male patient reported paediatric department with chief complaint of pain in the left lower back tooth region since two weeks. He was clinically diagnosed with multiple deep dental caries (74,75,84,85) and missing permanent right lower central incisor (41) [Table/Fig-1,2]. On radiographic investigation it was found that there was radiolucency involving enamel, dentin and pulp of 75 and radiolucency involving enamel dentin pulp and furcation of 74, 84 and 85. Also, found missing permanent tooth buds of second premolars (35,45) [Table/Fig-3].
Multiple dental caries in the lower deciduous molar.

Microdontia of 31 and missing 41.

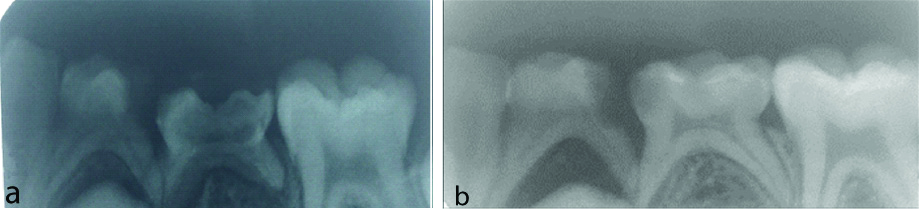
a) IOPAR (intraoral periapical radiograph) of 74, 75; b) IOPAR of 84, 85.
On general examination, he had normal stature and appearance, height of 44 inches, and 18 kg weight. Extra oral examination of limbs, hands, skin, hair, nails and eyes, neck, back, muscles, cranium and joints appeared normal. Intellectual and scholastic performance were normal compared with the children of same age. On intraoral soft tissue examination there were no abnormalities detected in mucosa, palate, floor of mouth, tongue, glands and gingiva.
There were no relevant prenatal and natal development histories. Postnatal child was breastfed for 2 years on demand feeding. Milestones of development attained at appropriate ages and there was no history of childhood diseases; Immunisation were taken at proper time. There were no deleterious habits present. Since, there was no signs and symptoms of any disease and absence of familial history of disease, blood profile was not done.
Radiographic Examination (IOPA) of mandibular left deciduous molars 74 and 75, showed radiolucency involving enamel, dentin and pulp with the furcal involvement in relation to 74 and the tooth 75 showed radiolucency involving enamel, dentin and pulp and missing tooth buds of mandibular left permanent premolar 35 [Table/Fig-3a]. Radiographic examination of mandibular right deciduous molars 84 and 85, showed radiolucency involving enamel, dentin, and pulp with the furcal involvement in relation to 84, 85 and missing tooth buds of mandibular left permanent premolar 45 [Table/Fig-3b].
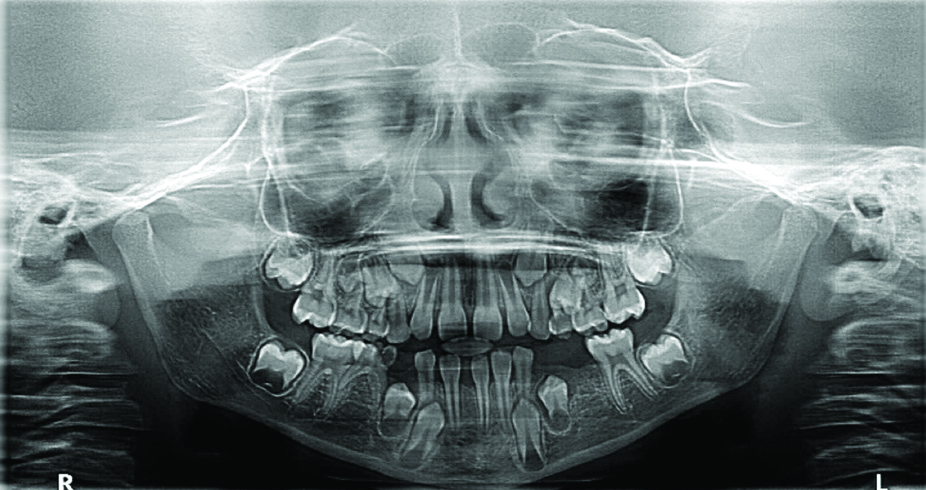
Patient initially refuse OPG. However, after explaining the consequences and extraction of teeth (74,75), OPG was taken to rule out any further missing teeth. OPG showed missing tooth buds of mandibular second premolars (35,45) mandibular right central incisor (41) and microdontia of mandibular left central incisor (31) [Table/Fig-4]. Diagnosis of chronic irreversible pulpitis of 74, 75, 84 and 85 and bilateral hypodontia with microdontia was made based on the radiographic and clinical findings. The mandibular left anterior teeth (31) lacked normal size in all dimensions, both mesiodistally and labiolingually checked from clinically, radiographically and from the diagnostic casts. In normal individual, mesiodistal and labiolingual dimensions of mandibular central incisor is 5 mm and 6 mm [1] and in present patient it was 4.2 mm and 5 mm, respectively.
Orthopantomograph (OPG) showing congenitally missing bilateral mandibular second premolars and central incisor.
Further Investigations: Detailed investigation was done to evaluate syndromic association. Hypodontia with microdontia is usually associated with syndromes or can be nonsyndromic. There was no indication of any oronasal defects or abnormality in the extremities and ectodermal characteristics like hair, nail, skin is indicative of syndrome. Growth charts were charted and growth percentiles were recorded. Height, weight and BMI showed below 3rd percentile which is below the normal percentile [Table/Fig-5] suggesting there is generalised retarded growth pattern.
Growth percentiles in each group (height, weight and BMI) according to World Health Organisation child growth standards [5].
| Sl no | Parameters | Obtained value | Growth percentile | Height at 50th percentile | Expected age |
|---|
| 1 | Height | 111.76 cm | <3rd | 127 cm | 5-6 years |
| 2 | Weight | 18 kg | <3rd | 26 kg | 4-5 years |
| 3 | BMI | 14.4 | <5th | 15.8 | 6-8 years |
Familial recurrence exemplar in hypodontia depicts a great level of genetic contribution [2]. But the radiographs of the sibling showed bilateral presence of second premolars. Parents are already patients of the same dental institution for endodontic procedures. Intraoral findings showed, both have all the permanent teeth present.
Differential diagnosis considered were: Hypoparathyroidism, Pseudohypoparathyroidism, Vitamin D Resistant Rickets, Oculodentoosseus Dysplasia, Dystrophic Epidermolysis Bullosa, Trichodentoosseous Syndrome, Ectodermal Dysplasia [3].
Since, there was no indication of any abnormality in the extremities and ectodermal characteristics like hair, nail, skin, the condition of ectodermal origin like those of dystrophic epidermolysis bullosa, ectodermal dysplasia, Trichodentoosseous Syndrome was ruled out.
Sweating, muscle weakness or temperature changes which are a feature of hypoparathyroidism were not noted. Absence of classic features of Vitamin D resistant rickets including that of frontal bossing, bowed legs, pot belly, pigeon’s chest, irritability, and restlessness helped in ruling it out. In our case the patient did not had any relevant systemic diseases [4]. All the above-mentioned conditions of differential diagnosis helped to rule out syndromic association and then concluded as nonsyndromic.
[Table/Fig-5] shows the growth percentiles in which the patient’s height, weight and BMI are corelated with the standard values. All the parameters have values below 3rd percentile.
As treatment plan, pulpectomy using MTA (Angelus MTA Mineral Trioxide Aggregate 2 Doses .28 gm) followed by stainless steel crown (3M” ESPE”) placed on 85, extraction of 84,74 and 75 followed by bilateral removable functional space maintainer for a period of three months. Apart from maintaining the mesiodistal dimension of the space created by extraction of a tooth, bilateral functional space maintainer should aid in mastication and prevent overeruption of the opposing tooth or teeth. It should also be simple, not interfere with normal occlusal adjustments, or restrict normal growth and development. Since the permanent teeth have not erupted yet, the patient is being kept under regular follow-up. As a long-term treatment option for hypodontia, placement of mini-implant and for microdontia, porcelain jacket crown was suggested once all the permanent teeth erupt.
The choice on whether the treatment plan requires space closure or opening of the spaces of the missing mandibular second premolars depends on determinants such as the age of the patient; the level of inherent crowding; status of the deciduous teeth; class of malocclusion; and the conditions of the patient (finances, attitude towards treatment, etc.,). In hypodontia patients, dental development is often discouraged, as is orthodontic treatment. So, in our case as a part of long-term treatment plan, placement of mini-implants for hypodontia, orthodontic treatment for space closure or delay the treatment plan until all the permanent teeth erupts was suggested to the parents. Patient’s parent opted for delaying the treatment.
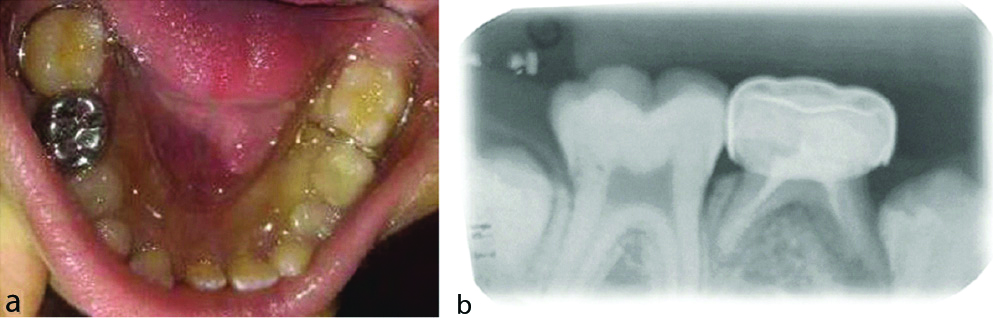
[Table/Fig-6a,b] shows post-operative view of pulpectomised teeth with bilateral functional space maintainer.
(a,b): Postoperative view: (a) Removable space maintainer in relation to 74,75 and 84; (b) Radiograph of 85.
Discussion
Congenitally missing teeth may range from hypodontia (few teeth), to multiple teeth (oligodontia) and to the complete absence of teeth (anodontia) [6]. Discrepancy in the space available and size of jaw, disturbances in the formation of the dental lamina, failure of tooth germ development is the main reasons for congenitally missing teeth [7]. A 3 to 10 % of the population have this clinical condition (hypodontia) if third molar is not considered. Third molars, second premolars, central and lateral incisors are the most commonly missing teeth [8]. Hypodontia can be presented as alone or along with other developmental anomalies like Microdontia, Delayed tooth development, Conical-crown shape Enamel hypoplasia, Taurodontism, Supernumerary teeth [9].
The skeletal age is inferior to the stature age but superior to the chronological age. The hormone excites protein synthesis and consequently tissue growth, including that of bone. However, considering deficiency of growth hormone is not a condition, the patient may reach adulthood, although he/she will be evaluated by the characteristics procured in childhood, such as height below 120 cm, which is the best attainable. The inadequate development of the forehead may lead to the maxilla and mandible being abnormally small, so that the physiological alterations associated with tooth eruption may direct to tooth malformation [10].
The significantly smaller tooth crown dimensions which were reported in the concerned family members showed the effect of the PAX9 mutation. This type of mutation is seen in both microdontia and hypodontia [11]. The present case reported a condition with simultaneous occurrence of microdontia and hypodontia with no familial tendency since the sibling’s radiograph showed the presence of teeth.
Graber LW reported in his study that cause of the congenitally missing teeth is one or more-point mutations in a polygenic system and transmission of these mutations takes place in an autosomal dominant pattern with variable expressions [8]. The cause of single missing teeth can be familial tendency in many cases. A few reports have been published regarding aetiology, prevalence, location and severity of hypodontia in families [12]. In a report, Parkin N et al., mentioned that there is no correlation in the number and location of the missing teeth of the patients and their parents or siblings. Environmental and epigenetic factors also play a major role in hypodontia suggesting that the variation in the expression of hypodontia in families is not solely genetic [13].
Brook AH et al., did a study associated with tooth dimensions in a family with hypodontia in which mutation was confirmed. They noted that all the teeth were of smaller size in family members with hypodontia as correlated to the control group. It was described that PAX9 mutation was accountable for congenitally missing teeth and smaller size of the crowns of the teeth [14]. Studies on the mouse genetics have shown a substantial fraction of genes are responsible for familial hypodontia, but in human only three genes have been identified for this condition: MSX1, PAX9 and AXIN2 [15].
Prevalence of hypodontia ranges from 4.19% in Indian population [16]. Most commonly missing teeth are mandibular second premolars (2.9%-3.22%) and mandibular lateral incisors (1.55%-1.78%) [8]. The present case shows a bilateral congenital missing of lower second premolars and lower central incisors.
Bargale SD and Kiran SD reported a case of non-syndromic occurrence of true generalised microdontia with mandibular mesiodens in a 12-year-old boy which contrasts with localised form of microdontia with concomitant occurrence of bilateral hypodontia as observed in our case. It is also been reported that the simultaneous presence of microdontia and supernumerary teeth to be reported in conditions with hypodontia [17].
Yunus N reported that as the number of missing teeth increased, the size of the crowns of the remaining teeth decreased signifies that concomitant occurrence of microdontia and hypodontia [18]. Chen Y et al., reported the permanent teeth germs for the bilateral maxillary lateral incisor were congenitally absent in a 9-year-old female with nonsyndromic occurrence of true generalised microdontia with hypodontia while the present case reports the absence of bilateral mandibular second premolar [19].
Periodontal damage, malocclusion, aesthetic problems, and alveolar bone deficiency are some complications in hypodontia. Multidisciplinary approach must be considered while treating missing premolars and central incisors [20].
Conclusion(s)
There are greater probabilities for the occurrence of multiple developmental dental anomalies in nonsyndromic patients and the diagnosis of these anomalies plays a crucial role in the final outcome of the treatment process owing to its implication in the growth and development of the child. A multidisciplinary approach should be carried out for treatment in patients with such conditions. The treatment should not only aim at improving aesthetics, speech and mastication, but also overall quality of life of the patient. Careful case selection, early diagnosis, timely intervention, patient cooperation, long term stabilisation and proper recall visits will ensure a treatment result that is successful, aesthetic and stable.
[1]. Wheeler RC, Textbook of Dental Anatomy and Physiology 1993 ed. 7PhiladelphiaWB Saunders Company:25 [Google Scholar]
[2]. Andersson E-MM, Axelsson S, Austeng ME, Øverland B, Valen IE, Jensen TA, Bilateral hypodontia is more common than unilateral hypodontia in children with Down syndrome: A prospective population-based studyEur J Orthodont 2014 36(4):414-18.10.1093/ejo/cjt06324014738 [Google Scholar] [CrossRef] [PubMed]
[3]. Suprabha BS, Sumanth KN, Boaz K, George T, An unusual case of nonsyndromic occurrence of multiple dental anomaliesIndian Journal of Dental Research 2009 20(3):38510.4103/0970-9290.5736419884730 [Google Scholar] [CrossRef] [PubMed]
[4]. Sahay M, Sahay R, Rickets-vitamin D deficiency and dependencyIndian Journal of Endocrinology and Metabolism 2012 16(2):16410.4103/2230-8210.9373222470851 [Google Scholar] [CrossRef] [PubMed]
[5]. World Health Organization. WHO child growth standards: Length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development. World Health Organization; 2006 [Google Scholar]
[6]. White and pharaoh editors, Oral Radiology principles and interpretation5th edition:332 [Google Scholar]
[7]. Rajendran R, Sivapathasundharam B, Shafer’s A textbook of Oral Pathology 2007 5th editionElsevier publication:64 [Google Scholar]
[8]. Graber LW, Congenital absence of teeth: A review with emphasis on inheritance patternsJ Am Dent Assoc 1978 96:266-75.10.14219/jada.archive.1978.0054342579 [Google Scholar] [CrossRef] [PubMed]
[9]. Alexandersen V, Nielsen OV, Generalised microdontia probably associated with intrauterine growth retardation in a medieval skeletonAm J Phys Anthropol 1970 33(3):389-401.10.1002/ajpa.13303303134321404 [Google Scholar] [CrossRef] [PubMed]
[10]. Acerbi AG, Freitas C, Magalhaes MHCG, Prevalance of numeric anomalies in the permanent dentition of patients with down syndromeSpecial Care Dentistry 2001 21(2):75-78.10.1111/j.1754-4505.2001.tb00230.x11484586 [Google Scholar] [CrossRef] [PubMed]
[11]. Brook AH, Griffin RC, Smith RN, Townsend GC, Kaur G, Davis GR, Tooth size patterns in patients with hypodontia and supernumerary teethArch oral biol 2008 54(Suppl1):S63-70.10.1016/j.archoralbio.2008.05.01618675390 [Google Scholar] [CrossRef] [PubMed]
[12]. Byahatti SM, The concomitant occurrence of hypodontia and microdontia in a single caseJournal of Clinical and Diagnostic Research 2010 4:3632-38. [Google Scholar]
[13]. Parkin N, Elcock C, Smith RN, Griffin RC, Brook AH, The aetiology of hypodontia: the prevalence, severity and location of hypodontia within familiesArch Oral Biol 2008 10.1016/j.archoralbio.2008.11.00219100963 [Google Scholar] [CrossRef] [PubMed]
[14]. Brook AH, Elcock C, Aggarwal M, Lath Dl, Russell JM, Patel Pi, Tooth dimension in hypodontia with a known PAX9 mutationArch Oral Biol 2008 54(Suppl 1):S57-62.10.1016/j.archoralbio.2008.05.01718653171 [Google Scholar] [CrossRef] [PubMed]
[15]. Cobourne MT, Familial human hypodontia- Is it all in the genes?Br Dent J 2007 203(4):203-08.10.1038/bdj.2007.73217721480 [Google Scholar] [CrossRef] [PubMed]
[16]. Gupta SK, Saxena P, Jain D, Prevalance and distribution of selected developmental anomalies in Indian populationJ Oral Sci 2011 53:231-23.10.2334/josnusd.53.23121712629 [Google Scholar] [CrossRef] [PubMed]
[17]. Bargale SD, Kiran SD, Nonsyndromic occurrence of true generalised microdontia with mandibular mesiodens-A rare caseHead & Face Medicine 2011 7(1):1910.1186/1746-160X-7-1922035324 [Google Scholar] [CrossRef] [PubMed]
[18]. Yunus N, Simultaneous occurrence of hypodontia and microdontia in a single caseAnnals of Dental Specialty 2014 2(1):31 [Google Scholar]
[19]. Chen Y, Zhou F, Peng Y, Chen L, Wang Y, Nonsyndromic occurrence of true generalised microdontia with hypodontia: A case reportMedicine 2019 98(26)10.1097/MD.000000000001628331261601 [Google Scholar] [CrossRef] [PubMed]
[20]. Gills DS, Barker CS, The multidisciplinary management of hypodontia: Team approachBritish Dent J 2015 218(3):29-35.10.1038/sj.bdj.2015.5225686431 [Google Scholar] [CrossRef] [PubMed]