The LMA is a supraglottic device which provides a safe and effective method of securing an airway in anaesthesia and critical care setting. With the increasing trend of day care surgery, day care anaesthesia has increased leading to increasing use of the LMA instead of facemask or tracheal tube. It is a better and safer alternative in emergency situations to secure airway or in situations where difficult airway is anticipated. Complications such as gagging, coughing and laryngospasm may occur in response to inserting LMA making its correct positioning difficult and leading to difficulty in insertion of LMA [1].
This may also increase the number of attempts of insertion leading to increase in incidence of sore throat. In spite of being used commonly, the technique for its insertion varies. Most commonly Propofol is preferred as it suppresses upper airway reflexes and provides adequate jaw relaxation [2,3]. However, side effects such as prolonged apnea and hypotension accompanies the drug [4,5]. Use of rapid onset, short acting neuromuscular blocking drugs such as succinylcholine suppress laryngeal reflexes but also leads to prolonged apnea, myalgia on administration of intubating dose (1-2 mg/kg) [6]. Therefore, low dose succinylcholine has been used. Low dose signifies the minimum dose at which adequate suppression of laryngeal reflexes occur with minimum or no incidence of myalgia [6].
Thus, this study was designed to assess the effects of low dose succinylcholine (0.1 mg/kg) with semi-inflated cuff on facilitation of LMA insertion as the primary objective. The secondary objective was to assess the avoidance of side effects associated with succinylcholine with use of lower dose (0.1 mg/kg).
Materials and Methods
A single-blinded randomised study was done in Acharya Vinobha Bhave Rural Hospital, Sawangi in unit of Jawaharlal Nehru Medical College, Sawangi in July 2019 after approval from the Institutional Ethics committee. {RefNo. DMIMS(DU)/IEC/2019/7942}.
Sample size was derived using software OpenEpi (openepi.com). For the sample size, the power was set at 80% (β=0.2) with an odd ratio of 30. The significant level was set as 5% (α=0.05, two-tailed). The calculated sample size was minimum 28, so taking potential drop-outs into consideration; the sample size was set as 30 for each group. A total of 60 American Society of Anesthesiologists.
Inclusion criteria: (ASA) class I and II patients of either sex, aged 20 to 60 years scheduled for surgical procedures under general anaesthesia lasting for less than one hour were taken for the study. A written and informed consent was derived from all patients.
Exclusion criteria: Following patients were excluded from the study:
ASA class >II
Patients having any anatomical abnormality of mouth, pharynx and larynx.
Risk of aspiration (gastroesophageal reflux or upper gastrointestinal surgery).
Full stomach (pregnancy, hiatal hernia).
High airway resistance
Anticipated difficult airway
Low pulmonary compliance (severe obesity).
History of hypersensitivity to study drug
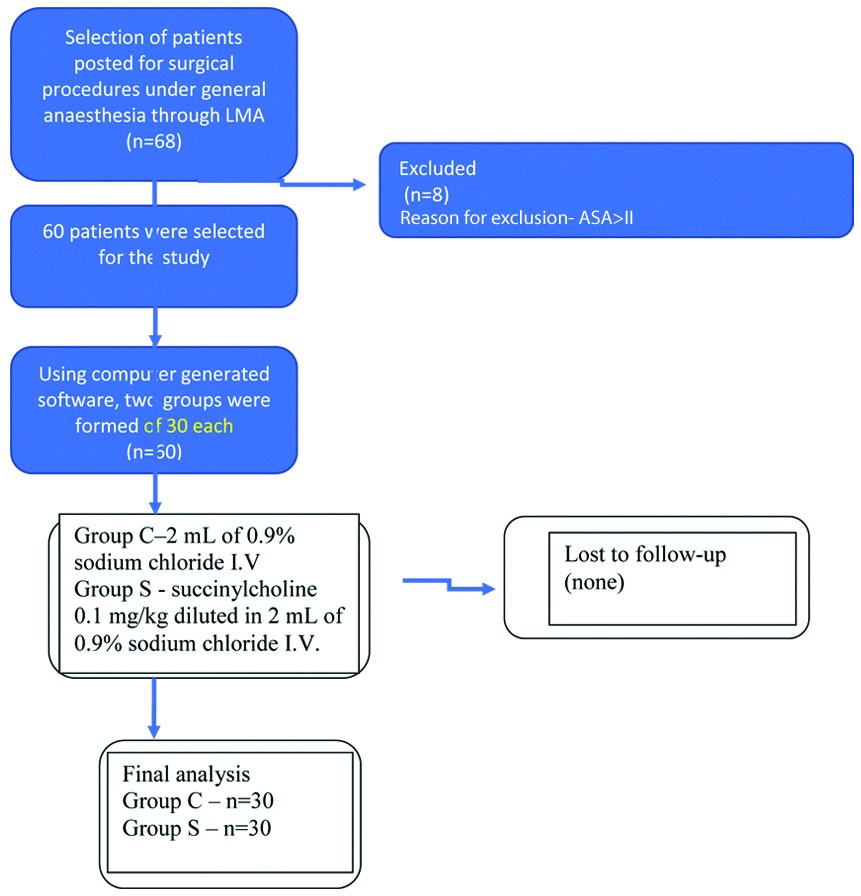
Sixty patients were randomly divided into two equal groups using computer generated software. Control group (Group C) was given 2 mL of 0.9% sodium chloride IV. Study Group (Group S) was given succinylcholine 0.1 mg/kg diluted in 2 ml of 0.9% sodium chloride I.V. Distribution of the patients presented in [Table/Fig-1].
Flowchart of patients enrolled in study.
Patients were preoxygenated for three minutes before induction and then premedication were given with inj. glycopyrrolate 0.004 mg/kg, inj. midazolam 0.01 mg/kg, and inj. fentanyl 1 μg/kg. Induction was done with inj. propofol 2 mg/kg. The effectiveness of drug was confirmed when the patient had lost consciousness, assessed by failure to respond to verbal commands and loss of eyelash reflexes. LMA was inserted 30 seconds later and the insertion conditions were noted.
If any airway reflexes, improper ventilation after insertion of the LMA, or limb and head movement, was seen then second dose of propofol 0.5 mg/kg bolus was given, after which next attempt at insertion was given 30 seconds later. This was done till successful insertion and number of attempts were recorded. On the contrary, ease of insertion was assessed only during the first attempt. Jun JH et al., described ease of insertion as “easy” if the first attempt of insertion was successful, “difficult” when second or third attempt was a success and “failure” when all three attempts fails. [7]. This classification was used in the index study.
A blinded investigator to the patient group collected the following demographic data: age, sex, weight, height. Incidence of cough and gagging, laryngospasm, head and limb movements, number of attempts, use of excess propofol and postoperative myalgia incidence was evaluated.
Statistical Analysis
The parameters and patient data were recorded and entered in Microsoft Excel sheet. (SPSS Inc. Chicago, IL, USA) version 20.0 software for windows was used for analysis. Incidence of emetic episodes was compared in different study groups and the results was analysed by chi-square test. p<0.05 was considered to be significant.
Results
The two groups were comparable in terms of age and gender as shown in [Table/Fig-2].
| Variables | Group S | Group C | p-value |
|---|
| Age (years) | 28.5±2.12 | 30±7.07 | 0.27 |
| Sex (m/f) | 16/14 | 17/13 | 1 |
| Weight (kg) | 61±1.40 | 60.5±1.6 | 0.2 |
| Height (cm) | 157±15.5 | 152±14.14 | 0.19 |
[Table/Fig-3] showed that in 93.33% of patients LMA was inserted in 1st attempt in group S, whereas 40% of patients in group C required more than one insertion attempt.
Number of attempts for LMA insertion amongst two groups.
| No. of attempts | Group C (Control) | Group S (Succinyl) | p-value |
|---|
| 1 | 18 (60%) | 28 (93.33%) | 0.0025* |
| ≥2 | 12 (40%) | 2 (6.67%) | 0.0025* |
*Statistically significant; Chi square test
[Table/Fig-4] showed incidence of Gagging in two groups and it was statistically significant (p<0.05). [Table/Fig-5] showed that there was no incidence of coughing in group S and the difference was statistically significant (p=0.0026).
| Gagging | Group C | Group S | p-value |
|---|
| Mild | 7 (23.33%) | 1 (3.33%) | 0.023* |
| Moderate | 6 (20%) | 1 (3.33%) | 0.046* |
| Severe | 2 (6.6%) | 0 | 0.475 |
*Statistically significant; Chi square test
Incidence of coughing among two groups.
| Group C | Group S | p-value |
|---|
| Mild | 8 (26.66%) | 0 | 0.0026* |
| Moderate | 0 | 0 | ND |
| Severe | 0 | 0 | ND |
*Statistically significant; Chi square test; ND: Not defined
“Easy” insertion conditions were obtained in 94% of patients in Group S compared to 36% of Group C. (p<0.001).
Head or limb movement occurred in 20 (66.6%) patients of group C, whereas it was not seen in group S (p<0.001)
[Table/Fig-6] showed that 93.3% of patients in group S did not require excess propofol.
Use of excess of propofol in two groups.
| Excess propofol | Group C | Group S | p-value |
|---|
| Yes | 18 (60%) | 2 (6.66%) | <0.0001* |
| No | 12 (40%) | 28 (93.3%) | <0.0001* |
*Statistically significant; Chi square test
[Table/Fig-7] showed that group S had postoperative myalgia in 26.66% cases while it was 13.33% in group C, results being statistically insignificant.
Incidence of postoperative myalgia in two groups.
| Postoperative myalgia | Group C | Group S | p-value |
|---|
| Yes | 4 (13.33%) | 8 (26.66%) | 0.20 |
| No | 26 (86.66%) | 22 (73.33%) | 0.20 |
Chi square test
Laryngospasm occurred in 13 patients of the group C. There were no incidences of laryngospasm in succinylcholine group and the difference was statistically significant (p=0.04).
Discussion
The LMA has been a breakthrough in airway management with its introduction in 1983 [8]. Salem WT obtained that in 75% of patients coughing and gagging was observed when LMA was inserted using only propofol and in only 60% of patients it was successful at the first attempt [9].
Succinylcholine is a depolarising neuromuscular blocker with side effects such as prolonged apnea, anaphylaxia, and myalgia are associated with intubating dose of succinylcholine (1-2 mg/kg). Thus, a low dose of succinylcholine (in this study 0.1 mg/kg) was used for achieving adequate LMA insertion conditions without side effects [6].
Therefore, objective of this study was to assess the effectiveness of low dose of Succinylcholine in facilitation of LMA insertion, but with minimal or rather no side effects related to succinylcholine. Various studies have been conducted comparing different low doses of succinylcholine to have adequate LMA insertion conditions with minimal side effects, as larger doses that resulted in significant postoperative myalgia. Yoshino A et al., compared 0.25 with 0.5 mg/kg of succinylcholine and found that 0.5 mg/kg of succinylcholine had better diminution of airway reflexes facilitating LMA insertion. They used thiopentone as an inducing agent without an opioid. But, this dose resulted in more postoperative myalgia [8]. George LR et al., compared two different doses of succinylcholine 0.1 mg/kg and 0.25 mg/kg for LMA insertion and observed that overall insertion conditions were better in 0.25 mg/kg group than 0.1 mg/kg group [10].
Aghamohammadi D et al., found that use of low dose of succinylcholine with supplementation of propofol had better LMA insertion conditions and use of excess propofol and number of attempts reduced significantly [11]. In this study, ease of insertion of LMA and the excellent insertion conditions were obtained in 94% of patients in Group S compared to 36% of group C (p<0.001). There was no incidence of head and limbs movement, coughing or laryngospasm in Group S. Gagging was significantly less observed in the Group S compared to the Group C.
Coughing, head and limbs movement occurred less frequently in the Group S compared to the Group C. These findings were consistent with Aghamohammadi D et al., where ease of insertion with 0.1 mg/kg succinylcholine was 93.33% and in normal saline group it was 36.66% (p<0.001) [11]. Korula S et al., did a comparative study for LMA insertion using succinyl choline 0.35 mg/kg and 0.08 mg/kg of atracurium and concluded that succinylcholine had better insertion conditions with minimal incidence of coughing, gagging and limb movements [12].
Similarly, Moneni A also did a comparative study for LMA insertion using succinylcholine 0.35 mg/kg and 0.06 mg/kg of atracurium and concluded that in succinylcholine group 83% patient had excellent insertion conditions, whereas it was only 46% with atracurium [13].
In the present study, for any airway reflexes, head or limb movement during LMA insertion, excess dose of propofol was given, following which another attempt at insertion was taken 30 seconds later. The amount of excess propofol used in the control group, was higher than succinylcholine group. In 60% patients of Group C excess dose of propofol was needed against 6.66% of Group S. The difference was statistically significant. (p<0.001). These findings were consistent with those of Jamil SN et al., [14].
In this study, LMA insertion in first attempt was found to be 93.33% in succinylcholine group whereas it was 60% in the control group. The difference was statistically significant. (p=0.0025). It is similar to Aghamohammadi D et al., where successful LMA insertion in first attempt in 90% patients in succinylcholine group was found and it was 46.6% patients in control group [11]. Ho KM and Chui PT also found that LMA insertion in first attempt was higher in the succinylcholine group [15].
Postoperative sore throat and myalgia was seen with a lesser incidence in control group (13.33%) than succinylcholine group (26.66%) and the difference was not statistically significant (p=0.2). It was similar to findings of Gunaseelan S and Prabhu RK, who also concluded the incidence of postoperative myalgia as statistically not significant [16]. Ho KM and Chui PT reported a higher incidence of myalgia in control group than in succinylcholine group which was statistically significant [15]. Also, Waters DJ and Mapleson WW gave a hypothesis that postsuccinylcholine myalgia is due to the shearing of soft tissues by the asynchronous muscle contractions. Thus, lesser dose of the drug will cause less myalgia [17].
Limitation(s)
The type of LMA used was not defined, so insertion conditions with different generation LMAs are not comparable. Also, patients with pseudocholinesterase enzyme deficiency were the limitation of the study.
Conclusion(s)
The use of low dose succinylcholine, reduced upper airway reflexes, also lead to ease of insertion of LMA and reduction in number of attempts. Reduced number of attempts hereby lead to less upper airway manipulation resulting in a lower incidence of myalgia and sore throat. Thus, low-dose succinylcholine (0.1 mg/kg) when compared to standard dose of propofol facilitated LMA insertion. The supplemental doses of propofol were also significantly reduced.
*Statistically significant; Chi square test
*Statistically significant; Chi square test
*Statistically significant; Chi square test; ND: Not defined
*Statistically significant; Chi square test
Chi square test