Symptomatic and Incidental Meckel’s Diverticulum in Children: Our Experience and Lesson
Rakesh Kumar1, Vivek Srivastava2, Vaibhav Pandey3
1 Senior Resident, Department of Paediatric Surgery, Institute of Medical Sciences, Banaras Hindu University, Varanasi, Uttar Pradesh, India.
2 Associate Professor, Department of General Surgery, Institute of Medical Sciences, Banaras Hindu University, Varanasi, Uttar Pradesh, India.
3 Associate Professor, Department of Paediatric Surgery, Institute of Medical Sciences, Banaras Hindu University, Varanasi, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vaibhav Pandey, Associate Professor, Department of Paediatric Surgery, Institute of Medical Sciences, Banaras Hindu University, Varanasi-221005, Uttar Pradesh, India.
E-mail: sunny.imsbhu@gmail.com
Introduction
The management of incidentally detected Meckel’s Diverticulum (MD) at laparotomy or laparoscopy has been debatable. In asymptomatic cases, the surgical management is associated with complication of around 1% but the complication rates are variable in other conditions like peritonitis.
Aim
To assess the management and outcome of incidentally diagnosed MD.
Materials and Methods
A retrospective study was conducted from January 2012 to December 2019 using the case records of the patient. The study included all the patients who were diagnosed with cases of MD in the Department. The patients were divided into two groups: Symptomatic Group and Incidental Group. The case records of all the patients were reviewed and data were collected for the demographic details, mode of presentation, the basis of diagnosis, treatment, outcome and follow-up.
Results
Total 132 patients were included in the study, 74 (56.06%) subjects were in symptomatic group and 58 (43.9%) were in incidental group. The mean age of symptomatic patients was 3.1±1.1 years and the incidental group was 6.5±2.4 years. It was significantly less in the symptomatic group (p≤0.001). All the patients in the symptomatic group were managed by laparotomy with diverticulectomy in 8 (10.8%), Wedge resection in 10 (13.5%) cases, segmental bowel resection in 44 (59.4%) and ileostomy in 12 (16.2%) cases. In the incidental group 9 (15.5%) patients underwent laparoscopic diverticulectomy and in rest 49 (66.2%) cases, only the primary procedure was performed. Six (10.3%) patients of incidental group without any intervention presented with complication at follow-up.
Conclusion
The laparoscopic diverticulectomy of MD should be performed in incidentally diagnosed cases of younger age group.
Diverticulectomy, Intestinal obstruction, Laparoscopy
Introduction
Developmental anomalies involving the vitelline ducts are commonly encountered by paediatric surgeons. The Meckel’s Diverticulum (MD) was described by Johann Friedrich Meckel as an outpouching or bulge developed due to incomplete obliteration of the Vetillointestinal Duct (VID) and is the most common congenital anomaly affecting the intestinal tract [1]. MD occurs in 2% of the general population and can occur at any age. Its management, when found incidentally at laparotomy, remains controversial [2]. Studies have reported a higher incidence of postoperative complications following surgical intervention in cases with incidental MD compared to overall rate of late complications if these incidentally diagnosed cases are left in-situ [3]. But other studies have rebutted these findings and have observed contrary results that the surgical excision of incidentally diagnosed MD did not resulted in any escalation of postoperative complications [4,5]. Further, there was high incidence of late complications in the no intervention group. With the advent of paediatric laparoscopy, the incidence of incidentally detected MD may increase because of the obvious reasons [6]. Since 2015, the Author, routinely screened terminal small bowel for the presence of MD while performing laparoscopy for different pathologies like laparoscopic Undescended Testis (UDT), appendicectomy and cholecystectomy. The study was done with an aim to assess the management and outcome of incidentally diagnosed MD. The clinicopathological characteristics of symptomatic and incidental cases were compared with the aim of arising to formulate a protocol regarding the management of incidental cases in the era of paediatric laparoscopy.
Materials and Methods
A retrospective study was conducted in the Department of Paediatric Surgery after approval from the Institutional Ethical Committee (No. Dean/2015-16/EC/362). The study was conducted from January 2012 to December 2019 using the case records of the patients. The study included all the children of age less than 12 years who were managed for complications of MD or those in which MD was found incidentally during laparoscopy or laparotomy for some other abdominal condition. The patients were divided into two groups: Symptomatic Group and Incidental Group based on above criteria. The case records of all the patients were reviewed for demographic profile of the children, indication of surgery, surgical procedures performed, postoperative complications and follow-up. The children in which the case records were missing for above details were excluded from the study. In present study, incidentally diagnosed group and asymptomatic group was same.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the Ethical standards of the Institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Statistical Analysis
Statistical analysis was performed using the IBM Statistical Package for the Social Sciences (SPSS) 19.0 Statistics for Windows software (IBM Corp., Armonk, NY). Data were expressed as Mean±SD (Standard Deviation). Data were tested for normality by using Kolmogorov-Smirnov test. Chi-square test was used to test the association between the variables. The p-value <0.05 was considered to be statistically significant.
Results
Total 132 patients were included in the study, out of which 56.06% (74) were symptomatic and 43.9% (58) were asymptomatic. The mean age of symptomatic patients was 3.1±.1.1 years and the asymptomatic group was 6.5±2.4 years. It was significantly less in the symptomatic group (p≤0.001). The gender ratio of the two groups was similar with a slight male preponderance in both the groups [Table/Fig-1].
Comparison of parameters between symptomatic and incidentally diagnosed cases of Meckel’s Diverticulum (MD).
| Parameters | Symptomatic (n=74) | Asymptomatic (Incidentally diagnosed) (n=58) | p-value* |
|---|
| Mean age (Years) | 3.1±1.1 | 6.5±2.4 | <0.001 |
| Gender (M:F) | Male | 44 | 38 | 0.47 |
| Female | 30 | 20 |
| Ratio | 1.4:1 | 1.9:1 |
| Ectopic mucosa | n=35 (47.2%) | n=42 (72.4%) | p-value |
| Present | 12 (34.2%) | 6 (14.2%) | 0.38 |
| Absent | 23 (65.7%) | 36 (85.7%) | |
*Chi-Square test
Histopathological records were available for 35 patients of the symptomatic group and 42 patients of the asymptomatic group. Only ectopic gastric mucosa was found in present study. The incidence of ectopic mucosa was significantly higher in symptomatic group compared to the asymptomatic group [Table/Fig-1].
In 9 (15.5%) of asymptomatic patients (n=58) a diverticulectomy was performed [Table/Fig-2]. All these cases were diagnosed during laparoscopy and were associated with Meckel’s band. None of these patients had any complication in postoperative period. In rest 49 cases, only the primary procedure was performed either by laparoscopy or laparotomy and no intervention was done for MD. Out of 49 asymptomatic patients of MD without intervention for MD, 6 (12.2%) patients presented with complications like haemorrhage or diverticulitis at follow-up. The median duration of this presentation was 3 years (range 2-6 years). On subgroup analysis of the patients with age less than 4 years, size of MD <2 cm and male gender had significantly higher chances of presenting later with complications [Table/Fig-3].
Details of presentation and procedures in the two groups.
| Diagnostic procedure in asymptomatic cases |
|---|
| Acute appendicitis | 13 (22.4%) |
| Undescended testis | 26 (44.8%) |
| Laparoscopic cholecystectomy | 5 (8.6%) |
| Diagnostic laparoscopy | 14 (24.1%) |
| Total | 58 |
| Symptomatic cases presentation |
| Intestinal obstruction | 42 (56.7%) |
| a. Band obstruction | 32 |
| b. Intussusception | 10 |
| Hemorrhage | 24 (32.4%) |
| Pain abdomen/Diverticulitis | 6 (8.1%) |
| Peroforatio of Meckel’s diverticulum | 2 (2.7%) |
| Total | 74 |
| Surgical Procedure |
| Laparoscopic diverticulectomy (Asymptomatic cases) | 9 (10.8%) |
| Wedge resection | 10 (12.0%) |
| Diverticulectomy | 8 (9.6%) |
| Resection and anastomosis | 44 (53.1%) |
| Ileostomy | 12 (14.4%) |
| Total | 83 |
Subgroup analysis of asymptotic group for risk factors of developing complications.
| Total patients n=49 | Complication later at follow-up n=6 (%) | No complication groups n=43 (%) | Odds ratio | CI (95%) | p-value* |
|---|
| Age (years) |
| <4 | 4 (66.7) | 10 (23.3) | 6.6 | 1.049-41.51 | 0.027 |
| >4 | 2 (33.3) | 33 (76.7) |
| Gender |
| Male | 5 (83.3) | 14 (32.6) | 10.36 | 1.103-97.25 | 0.016 |
| Female | 1 (16.7) | 29 (67.4) |
| Length of MD (cm) |
| <2 | 2 (33.3) | 34 (79.1) | 7.55 | 1.189-48.03 | 0.017 |
| >2 | 4 (66.7) | 9 (20.9) |
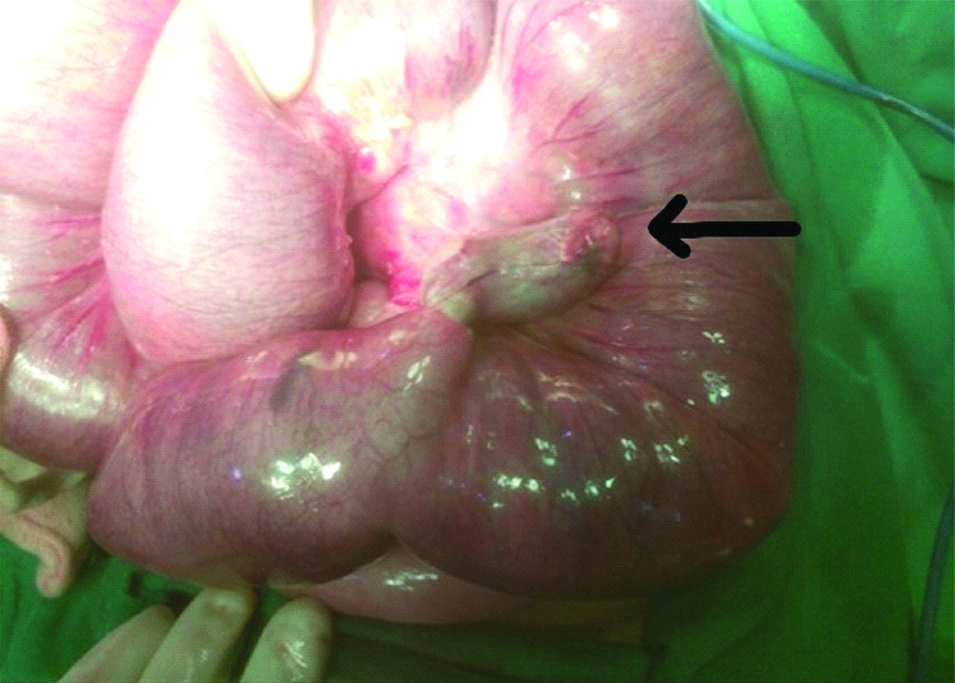
The most common presentation in the symptomatic group (n=74) was acute intestinal obstruction [Table/Fig-4] followed by obstruction, haemorrhage, recurrent pain and perforation peritonitis [Table/Fig-2]. All the patients with symptomatic MD were managed by laparotomy. Diverticulectomy was performed in 8 (10.8%) patients, Wedge resection 10 (13.5%) cases. Resection of the ileal segment with ileo-ileal anastomosis was performed in 44 (59.4%) patients. About 12 (16.2%) patients were managed by a diversion in the form of ileostomy due to underlying gangrene and haemodynamic instability and diverticulectomy. Out of these, 3 (4.05%) patients developed a postoperative anastomotic leak in the resection group and all underwent relaparotomy. An ileostomy was used in two and resection and anastomosis in the other patient. About 16 (21.6%) patients with laparotomy presented with an adhesive obstruction within a median follow-up of 4.5 years (range 2-6 years). Out of this 11 (68.7%) had resection and anastomosis and in 5 (31.2%) cases had segmental resection of MD.
Meckel’s Diverticulum (MD) presenting with band obstruction. Black arrow indicating the MD.
Discussion
The MD is the most common congenital anomaly of the small bowel. Its prevalence varies from 5-25% and the incidence of symptoms in patients with a MD can range from 4-34% [7,8]. The male-female distribution of asymptomatic cases is same but it is around four-time more common in males than females in among the symptomatic cases [9]. In present study, the male cases dominated both in the symptomatic and asymptomatic group. The proportion of symptomatic cases decreases with the highest risk of complication in infants and children. Overall, around 50% of symptomatic cases occur in children in less than 2 years of age [8,10].
In children, the higher rate of morbidity and mortality is reported in symptomatic cases compared to asymptomatic [11,12]. In a systematic review of 244 retrospective studies, Zani A et al., found that the resection of incidentally discovered MD had a significantly higher postoperative complication rate in comparison to those in which it was left in-situ. The present study concluded that incidentally diagnosed cases of MD should be left as this reduces the risk of postoperative complications and does not alters the rate of late complications [3]. But in retrospective review of 76 patients with Zulfikaroglu B et al., found that the resection of incidentally discovered MD was not associated with increased operative morbidity and mortality [4]. Similarly, other studies have highlighted different criteria, that in presence of like male sex, younger than 45 years, diverticula longer than 2 cm and the presence of a fibrous band, should be resected [13].
The most common presentation in present study for symptomatic cases was obstruction compared to bleeding in series from some western countries [9,12]. We hypothesise that acute cases of bleeding may be misdiagnosed in our setup or these children die even before reaching hospital as most of the patients were from poor social background.
All symptomatic complicated MD require surgical resection but the procedure of choice is controversial. The procedure range from simple diverticulectomy in cases with no ectopic mucosa, wedge resection in cases with heterogeneous consistency on palpation to resection and anastomosis [14-16]. In the present study, resection was performed in maximum cases as most of the cases presented with long standing obstruction. The condition of bowel near the diverticula was unhealthy in most of these cases.
The incidence of complication varies with the prevalence of ectopic mucosa in the MD. The gastric mucosa is associated with highest rate of complication. The gastric mucosa may be responsible for ulceration and a higher incidence of bleeding. The incidence of the gastric mucosa is estimated at about 16% in asymptomatic and 50-80% in symptomatic MD [17,18]. In present study also, the ectopic mucosa was higher in symptomatic cases compared to asymptomatic cases.
There has been long standing debate on management of asymptomatic MD. Most studies favour excision of asymptomatic Meckel’s in younger children. With the advent of laparoscopy this indication is expanding. As the most common complication in follow-up in most series is adhesive obstruction and with more and more laparoscopic procedures, this number is decreasing [18,19]. Further, six of the cases in which Meckel’s was left in-situ, presented with complications later. The complications of adhesive obstruction were slightly more in resection group but there was no statistical difference for the excision or wedge resection group. Ileostomy was performed in cases with widespread intra-abdominal infection or marked oedema of the intestinal wall.
Limitation(s)
The retrospective nature of the study was the main limitation.
Conclusion(s)
The rate of late complications in asymptomatic incidentally diagnosed MD was higher in males with age less than four years and diverticulum of size more than 2 cm. Laparoscopic diverticulectomy should be performed in these cases.
*Chi-Square test
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 26, 2020
Manual Googling: Aug 19, 2020
iThenticate Software: Sep 15, 2020 (16%)
[1]. Rattan KN, Singh J, Dalal P, Rattan A, Meckel’s diverticulum in children: Our 12-year experienceAfrican J Paediatr Surg 2016 13(4):170-74.10.4103/0189-6725.19467128051045 [Google Scholar] [CrossRef] [PubMed]
[2]. Alemayehu H, Hall M, Desai AA, St Peter SD, Snyder CL, Demographic disparities of children presenting with symptomatic Meckel’s diverticulum in children’s hospitalsPediatr Surg Int 2014 30(6):649-53.10.1007/s00383-014-3513-y24811048 [Google Scholar] [CrossRef] [PubMed]
[3]. Zani A, Eaton S, Rees CM, Pierro A, Incidentally detected Meckel diverticulum: To resect or not to resect?Ann Surg 2008 247:276-81.10.1097/SLA.0b013e31815aaaf818216533 [Google Scholar] [CrossRef] [PubMed]
[4]. Zulfikaroglu B, Ozalp N, Zulfikaroglu E, Ozmen MM, Tez M, Koc M, Is incidental Meckel’s diverticulum resected safely?N Z Med J 2008 121:39-44. [Google Scholar]
[5]. Duan X, Ye G, Bian H, Yang J, Zheng K, Liang C, Laparoscopic vs. Laparoscopically assisted management of Meckel’s diverticulum in childrenInt J Clin Exp Med 2015 8(1):94-100. [Google Scholar]
[6]. Chen Q, Gao Z, Zhang L, Zhang Y, Pan T, Cai D, Multifaceted behavior of Meckel’s diverticulum in childrenJ Pediatr Surg 2018 53(4):676-81.10.1016/j.jpedsurg.2017.11.05929331260 [Google Scholar] [CrossRef] [PubMed]
[7]. Hansen CC, Søreide K, Systematic review of epidemiology, presentation, and management of Meckel’s diverticulum in the 21st centuryMedicine (Baltimore) 2018 97(35):e1215410.1097/MD.000000000001215430170459 [Google Scholar] [CrossRef] [PubMed]
[8]. Al Janabi M, Samuel M, Kahlenberg A, Kumar S, Al-Janabi M, Symptomatic paediatric Meckel’s diverticulum: Stratified diagnostic indicators and accuracy of Meckel’s scanNucl Med Commun 2014 35(11):1162-66.10.1097/MNM.000000000000019325162963 [Google Scholar] [CrossRef] [PubMed]
[9]. Menezes M, Tareen F, Saeed A, Khan N, Puri P, Symptomatic Meckel’s diverticulum in children: A 16-year reviewPediatr Surg Int 2008 24(5):575-77.10.1007/s00383-007-2094-418322689 [Google Scholar] [CrossRef] [PubMed]
[10]. Anand P, Singh S, Sarin N, Intussusception caused by heterotopic gastric mucosa in small intestine: A case reportJ Med Case Rep 2017 11(1):25810.1186/s13256-017-1425-x28893301 [Google Scholar] [CrossRef] [PubMed]
[11]. Akçakaya A, Alimoglu O, Ozkan OV, Sahin M, Complicated Meckel’s diverticulumUlus Travma Acil Cerrahi Derg 2003 9(4):246-49. [Google Scholar]
[12]. Charki MT, Oukhouya MA, Benmassaoud Z, Mahmoudi A, Khattala K, Bouabdallah Y, Complications of Meckel’s diverticulum in children: About 18 casesPan Afr Med J 2019 33:11310.11604/pamj.2019.33.304.1896631692745 [Google Scholar] [CrossRef] [PubMed]
[13]. Robijn J, Sebrechts E, Miserez M, Management of incidentally found Meckel’s diverticulum a new approach: Resection based on a Risk ScoreActa Chir Belg 2006 106:467-70.10.1080/00015458.2006.1167993317017710 [Google Scholar] [CrossRef] [PubMed]
[14]. Varcoe RL, Wong SW, Taylor CF, Newstead GL, Diverticulectomy is inadequate treatment for short Meckel’s diverticulum with heterotopic mucosaANZ J Surg 2004 74(10):869-72.10.1111/j.1445-1433.2004.03191.x15456435 [Google Scholar] [CrossRef] [PubMed]
[15]. Robinson JR, Correa H, Brinkman AS, Lovvorn HN, Optimizing surgical resection of the bleeding Meckel diverticulum in childrenJ Pediatr Surg 2017 52:1610-15.10.1016/j.jpedsurg.2017.03.04728359587 [Google Scholar] [CrossRef] [PubMed]
[16]. Blouhos K, Boulas KA, Tsalis K, Barettas N, Paraskeva A, Kariotis I, Meckel’s Diverticulum in adults: Surgical concernsFront Surg 2018 5:5510.3389/fsurg.2018.0005530234126 [Google Scholar] [CrossRef] [PubMed]
[17]. Sinopidis X, Fouzas S, Kambouri K, Panagidis A, Alexopoulos V, Karatza A, Predictive model of heterotopy in Meckel’s diverticulum in childrenANZ J Surg 2019 89(6):E241-45.10.1111/ans.1522631067605 [Google Scholar] [CrossRef] [PubMed]
[18]. Chan KW, Lee KH, Mou JW, Cheung ST, Tam YH, Laparoscopic management of complicated Meckel’s diverticulum in children: A 10-year reviewSurg Endosc 2008 22(6):1509-12.10.1007/s00464-008-9832-018322735 [Google Scholar] [CrossRef] [PubMed]
[19]. Cobellis G, Cruccetti A, Mastroianni L, Amici G, Martino A, One-trocar transumbilical laparoscopic-assisted management of Meckel’s diverticulum in childrenJ Laparoendosc Adv Surg Tech 2007 17(2):238-34.10.1089/lap.2006.003617484657 [Google Scholar] [CrossRef] [PubMed]