Abrikossoff’s Tumour of Oesophagus- An Innocent Bystander or a Silent Killer?
Kuppusamy Senthamizhselvan1, Pazhanivel Mohan2, Bheemanathi Hanuman Srinivas3, Abdoul Hamide4
1 Assistant Professor, Department of Medical Gastroenterology, JIPMER, Puducherry, India.
2 Associate Professor, Department of Medical Gastroenterology, JIPMER, Puducherry, India.
3 Associate Professor, Department of Pathology, JIPMER, Puducherry, India.
4 Professor, Department of Medical Gastroenterology, JIPMER, Puducherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kuppusamy Senthamizhselvan, Department of Medical Gastroenterology, Superspeciality Building, JIPMER, Dhanvantari Nagar, Puducherry, India.
E-mail: senthamizh2909@gmail.com
Oesophageal Granular Cell Tumour (GCT) is a rare tumour arising from schwann cells of the submucosal nerve plexus. They are slow-growing generally, benign though malignant potential has been reported. They are usually found incidentally during endoscopic evaluation of dyspepsia or dysphagia. They rarely produce symptoms on their own unless the size is larger, ulceration occur on their surface or when it compresses the adjacent structure. Though they are submucosal, they are usually diagnosed by standard biopsy techniques or after an endoscopic resection. Oesophageal GCTs without muscularis propria attachment are amenable for Endoscopic Submucosal Dissection (ESD) which is a minimally invasive procedure when compared to surgical resection. They may require follow-up after resection. Here, we report a case of 39-year-old male who presented with epigastric pain, heart burn and underwent endoscopy for the same, which revealed a sub-centimetric yellowish white flat lesion above oesophago-gastric junction. Biopsy was done and histopathology and immuno-histochemistry revealed sheets of tumour cells with clear granular cytoplasm which stained positive for S100 and Calretinin, with a Ki-67 index of 2%, confirming the diagnosis of a benign GCT. Endoscopic Ultrasound (EUS) revealed no local invasion and the patient was advised three months follow-up and annual surveillance endoscopy.
Biopsy, Granular cell tumour, Oesophago-gastric junction, Schwann cells
Case Report
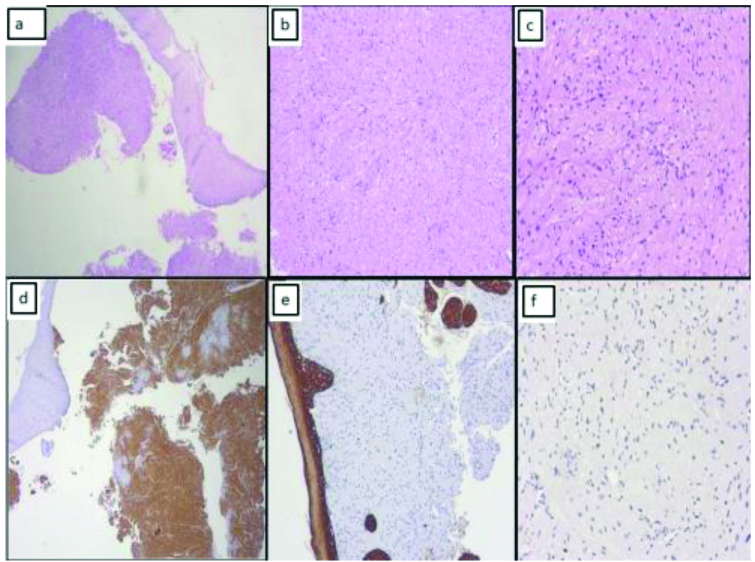
A 39-year-old male presented with epigastric pain and occasional heart burn for the past one year. He did not have any alarming gastrointestinal symptoms like weight loss, vomiting, gastrointestinal bleeding, and difficulty in swallowing. He was diagnosed to have systemic hypertension before three years and was on tablet Amlodipine 5 mg once daily. He used over-the-counter Omeprazole 20 mg capsule twice a day, during his symptom exacerbation in the past one year. He did not consume alcohol or smoke cigarettes. None of his family members had any gastrointestinal problems. On examination he was alert and comfortable. There was no pallor, icterus, and significant lymphadenopathy. His blood pressure was 124/80 mm Hg in sitting position and pulse rate was 84/min. Abdomen was soft and no mass was palpable. Examination of cardiovascular system and respiratory system was normal. Blood investigations showed haemoglobin-12.4 gm/dL, total leukocyte count-10,400 cells/cubic millimetre, platelet-2.9 lacs cells/cubic millimetre, fasting blood glucose-82 mg/dL, blood urea-39 mg/dL, serum creatinine-0.9 mg/dL. Patient was provisionally diagnosed to have persistent dyspepsia with epigastric syndrome and hence, Oesophago-Gastro-Duodenoscopy (EGD) was performed which revealed a yellowish white flat lesion in the distal oesophagus just above the oesophago-gastric junction [Table/Fig-1]. The differential diagnosis for this endoscopic finding was leiomyoma, lipoma and GCT. Biopsies were taken from the lesion using standard biopsy techniques. The mucosa of the stomach and duodenum was normal. Rapid urease test for Helicobacter pylori was negative. EUS revealed a sub-centimetric, hypoechoic submucosal lesion in distal oesophagus. Histopathologic examination showed tumour along with normal squamous epithelium; tumour cells were arranged in sheets and comprised of moderate to abundant amount of granular eosinophilic cytoplasm with central to eccentrically placed bland nuclei [Table/Fig-2a-c]. The pathologist considered GCT, rhabdomyoma, granular cell leiomyoma, hibernoma and xanthoma in differential diagnosis. The immunohistochemistry was positive for S-100 and Calretinin and negative for Pancytokeratin. The Ki-67 index of the tumour was 2% [Table/Fig-2d-f]. Hence, a diagnosis of benign GCT (Abrikossoff’s tumour) was made. In view of smaller size and low Ki-67 index of the tumour, a conservative approach was recommended. He was advised to take Omeprazole 20 mg capsule during epigastric pain and heart burn. The patient was on three months follow-up in outpatient clinic, his symptoms are controlled with Omeprazole and he was scheduled for annual surveillance EGD.
Oesophago-Gastro-Duodenoscopy (EGD) showing a yellowish white flat lesion in the distal oesophagus.

Photomicrographs of: a) Oesophageal biopsy showing tumour cells (H&E X100); b) Tumour cells arranged in sheets (H&E X200); c) Cells comprised of moderate to abundant amount of granular eosinophilic cytoplasm with central to eccentrically placed bland nuclei (H&E X400); Immunohistochemistry with; d) S-100 and calretinin showed strong positivity in tumour cells; e) Pancytokeratin (H&E X400) showed negative in tumour cells; f) Low Ki-67 index (H&E X400).
Discussion
GCT was first described by Abrikossoff in 1926, since then this rare tumour is also called by his name [1]. GCT can occur virtually in all organs. Gastrointestinal GCTs constitute 6-8%, among them oesophagus is the commonest organ [2]. Oesophageal GCT originates from Schwann cells of the submucosal neural plexus. In two-thirds of the patients, it is located in the distal oesophagus. It constitutes 1% of all the benign tumours of the oesophagus [3]. Among oesophageal GCT, 1-3% has a malignant potential with a 5-year survival rate of less than 35% [4]. Cervical lymph node metastasis has been documented [5]. There are reports of coincidental intramucosal adenocarcinoma of the oesophagus and squamous cell carcinoma of head and neck [6,7]. However, the pseudo-epitheliomatous hyperplasia of the mucosa can give a false picture of squamous cell carcinoma. GCT has a slight male preponderance and mostly diagnosed in the 4th to 6th decade [8]. It can occur as a single lesion or multiple lesions in the oesophagus [9]. They are diagnosed incidentally during endoscopic evaluation for dyspepsia and gastroesophageal reflux disease. The usual symptoms associated are abdominal bloating, loss of appetite and heart burn. However, it can cause dysphagia if the size is more than 1 cm in diameter. Index patient presented with dyspeptic symptoms and GCT was diagnosed incidentally which is the case most often, as reported in a recent case series by Tan HJ et al., [10]. The location at distal oesophagus is consistent with previous reports [11]. During endoscopy, GCTs are sessile, white to yellowish lesions. Larger lesions can undergo ulceration and necrosis. Though they are characteristically submucosal lesions, they can involve mucosa and muscularis propria [12].
EUS can be used to assess local invasion and for fine needle aspiration of the lesion. In EUS, GCTs characteristically are homogenous and hypoechoic and can be mistaken for lipoma or leiomyoma which arise from lamina propria and muscularis propria, respectively. Histopathology shows sheets of polygonal or round cells with abundant granular cytoplasm, which is pathognomonic for GCT. Hence, this tumour is called by this name. The granular appearance is due to accumulation of secondary lysosomes in the cytoplasm. These granules are Periodic Acid Schiff (PAS) positive and diastase-resistant. Immunohistochemistry (IHC) shows positivity for S100, C68, CD57, Calretinin, Nestin and Vimentin [13]. Fanburg-Smith JC et al., proposed that the presence of tumour necrosis, tumour cell spindling, large nucleoli, increased mitotic activity, increased nuclear-cytoplasmic ratio and pleomorphism favours malignancy [14].
Treatment strategies for oesophageal GCT are conservative approach, endoscopic resection, and surgery. Absence of symptoms, small size (<1 cm), absence of invasion in EUS and benign histopathology are indications for conservative approach where patient is advised to undergo annual surveillance endoscopy. Presence of symptoms due to the tumour, size of 1-2 cm and non-attachment to the muscularis propria are indications for endoscopic resection, when there is evidence of tumour invasion or a suspicion of malignancy, surgery is preferable. ESD is a minimally invasive procedure and is recommended as the procedure of choice wherever the facility and expertise are available [15].
Conclusion(s)
Oesophageal GCT is a rare and generally benign tumour but not without malignant potential. It is diagnosed as a bystander lesion during endoscopic evaluation of dyspepsia or gastroesophageal reflux however, it can have progressive growth, morbidity and even mortality in some patients. It can be diagnosed only if the endoscopist is aware of such a condition and has a high index of suspicion for it. Patient must be well informed about the nature of the disease and they must be involved in the treatment decisions. ESD is relatively safe and effective in most of the cases.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 19, 2020
Manual Googling: Jul 16, 2020
iThenticate Software: Sep 15, 2020 (13%)
[1]. Abrikossoff A, Uber Myome, ausgehend von der quergestreifte willkurlichen MuskulaturVirchows Arch Pathol Anat 1926 260:215-33.10.1007/BF02078314 [Google Scholar] [CrossRef]
[2]. Radaelli F, Minoli G, Granular cell tumours of the gastrointestinal tract: Questions and answersGastroenterol Hepatol 2009 5(11):798-800. [Google Scholar]
[3]. Terada T, Benign tumours of the esophagus: A histopathologic study of 49 cases among 931 consecutive esophageal biopsiesGastroenterology Res 2009 2(2):100-03.10.4021/gr2009.02.1277 [Google Scholar] [CrossRef]
[4]. David O, Jakate S, Multifocal granular cell tumour of theesophagus and proximal stomach with infiltrative pattern: A case report and review of the literatureArch Pathol Lab Med 1999 123(10):967-73.10.5858/1999-123-0967-MGCTOT10506457 [Google Scholar] [CrossRef] [PubMed]
[5]. Chatelain D, Terris B, Molas G, Infiltrating granular cell tumour of the esophagus: A description of two casesAnn Pathol 2000 20(2):158-62. [Google Scholar]
[6]. Alkhoury F, Martin JT, Fiedler P, Esophageal granular cell tumour colliding with intramucosal adenocarcinoma: A case reportCases J 2009 2:809310.4076/1757-1626-2-809319830048 [Google Scholar] [CrossRef] [PubMed]
[7]. Caroppo D, Salerno G, Merolla F, Coexistent squamous cell carcinoma and granular cell tumour of head and neck region: Report of two very rare cases and review of the literatureInt J Surg Pathol 2018 26(1):47-51.10.1177/106689691772451328783989 [Google Scholar] [CrossRef] [PubMed]
[8]. Parfitt JR, McLean CA, Joseph MG, Granular cell tumours of the gastrointestinal tract: Expression of nestin and clinicopathological evaluation of 11 patientsHistopathology 2006 48(4):424-30.10.1111/j.1365-2559.2006.02352.x16487364 [Google Scholar] [CrossRef] [PubMed]
[9]. Lowe DL, Chaudhary AJ, Lee JR, Four cases of patients with gastrointestinal granular cell tumoursSouth Med J 2007 100(3):298-300.10.1097/SMJ.0b013e318030eeff17396735 [Google Scholar] [CrossRef] [PubMed]
[10]. Tan JH, Chong CXZ, Lim KH, Ong HS, Granular cell tumor of esophagus: A rare disease of the esophagusAnnals of Case Reports and Images 2018 1(1):310.24983/scitemed.acri.2018.00076 [Google Scholar] [CrossRef]
[11]. Thumallapally N, Ibrahim U, Kesavan M, Esophageal granular cell tumour: A case report and review of literatureCureus 2016 8(9):e78210.7759/cureus.78227752408 [Google Scholar] [CrossRef] [PubMed]
[12]. Lu W, Xu MD, Zhou PH, Zhang YQ, Chen WF, Zhong YS, Endoscopic submucosal dissection of esophageal granular cell tumourWorld J Surg Oncol 2014 12:22110.1186/1477-7819-12-22125030028 [Google Scholar] [CrossRef] [PubMed]
[13]. Nie L, Xu G, Wu H, Huang Q, Sun Q, Fan X, Granular cell tumour of the esophagus: A clinicopathological study of 31 casesInt J Clin Exp Pathol 2014 7(7):4000-07. [Google Scholar]
[14]. Fanburg-Smith JC, Meis-Kindblom JM, Fante R, Malignant granular cell tumour of soft tissue: Diagnostic criteria and clinicopathologic correlationAm J Surg Pathol 1998 22(7):779-94.10.1097/00000478-199807000-000019669341 [Google Scholar] [CrossRef] [PubMed]
[15]. Knoop RF, Schmidt A, Kayser G, Thimme R, Fischer A, Endoscopic submucosal dissection of an esophageal granular cell tumourVideo GIE 2019 4(2):58-61.10.1016/j.vgie.2018.10.01530766943 [Google Scholar] [CrossRef] [PubMed]