Periradicular Cystic Enucleation and PRF Grafting Following Apicoectomy in Trichotillomania Patient- A Case Report
Vimanyu Kataria1, Surender Sodhi2, Shikha Dogra3, Vignesh Guptha Raju4
1 Senior Lecturer, Department of Oral and Maxillofacial Surgery, Sudha Rustogi College of Dental Sciences and Research, Faridabad, Haryana, India.
2 Principal, Professor and Head, Department of Oral and Maxillofacial Surgery, Dasmesh Institute of Research and Dental Sciences, Faridkot, Punjab, India.
3 Senior Lecturer, Department of Pedodontics and Preventive Dentistry, SGT Dental College and Hospital, Gurgaon, Haryana, India.
4 Reader, Department of Pedodontics and Preventive Dentistry, Karpaga Vinayaga Institute of Dental Sciences, Kanchipuram, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shikha Dogra, Department of Pedodontics and Preventive Dentistry, SGT Dental College and Hospital, Gurgaon-122413, Haryana, India.
E-mail: shikha.dogra87@gmail.com
Diagnosis and treatment planning of untreated traumatised anterior teeth specially in children with psychiatric disorders or special health care needs is a challenge to paediatric dentist, that too in non-pharmacological means is a difficult task. Most of the time when these patients report with such complaint, it is already too late. This could be due to unintentional reasons like lack of parent awareness or patient’s response at the time of insult. All these factors bypass the time of conservative and minimal invasive treatment approaches. Ultimately, delayed treatment of trauma to anterior region exposes pulp and infection progress to periradicular region with cystic changes. Here, in this case report, the non-pharmacological management of periradicular cyst enucleation, followed by apicoectomy and Platelet Rich Fibrin (PRF) grafting was done in a 15-year-old female patient with obsessive compulsive disorder i.e., Trichotillomania (TTM) under local anaesthesia. Symptoms and intraoral swelling was resolved postoperatively in follow-up visits.
Accelerated healing, Obsessive compulsive disorder, Surgical endodontics
Case Report
A 15-year-old female patient and her parents reported to a dental clinic with a chief complaint of pain and swelling in upper left front tooth region of the jaw for past two weeks. Patient gave a history of fall 14 months back while learning to cycle, following which she felt pain in relation to upper left anterior region of the jaw. There was no damage to coronal part of tooth on inspection. No significant family past history was present and patient’s medical history revealed TTM 5 years back. Patient was not under any medication for the same. Past dental history revealed pain in relation to tooth #21 and #22, which got relieved on taking medicines prescribed by dentist. Later patient had an intermittent dull pain in relation to same teeth, but they didn’t seek any intervention. Following this, patient had pain and swelling in left maxillary anterior region, she visited another dentist who started endodontic treatment in left maxillary anterior teeth but referred this patient to paediatric dentist after gathering history of TTM. Patient was able to communicate well and was uncooperative and fearful due to the past dental experience. Extraorally, swelling was not evident with no clinically palpable lymph nodes. She had noticeable hair loss in scalp area with shortened hair (which she used to pull in deep thoughts as reported by the parents, when she was under stress) [Table/Fig-1a,b].
a) A 15-year-old female patient frontal view; b) Profile view showing noticeable hair loss in scalp area with shortened hair.

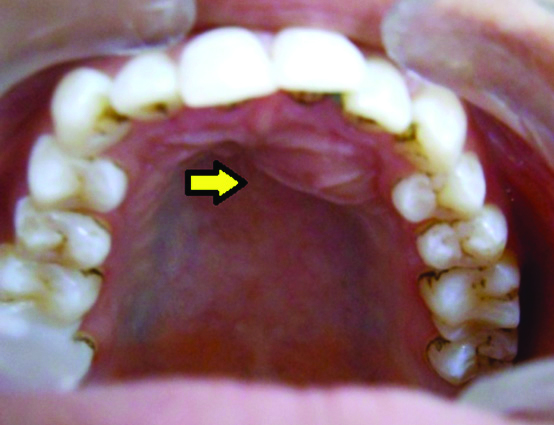
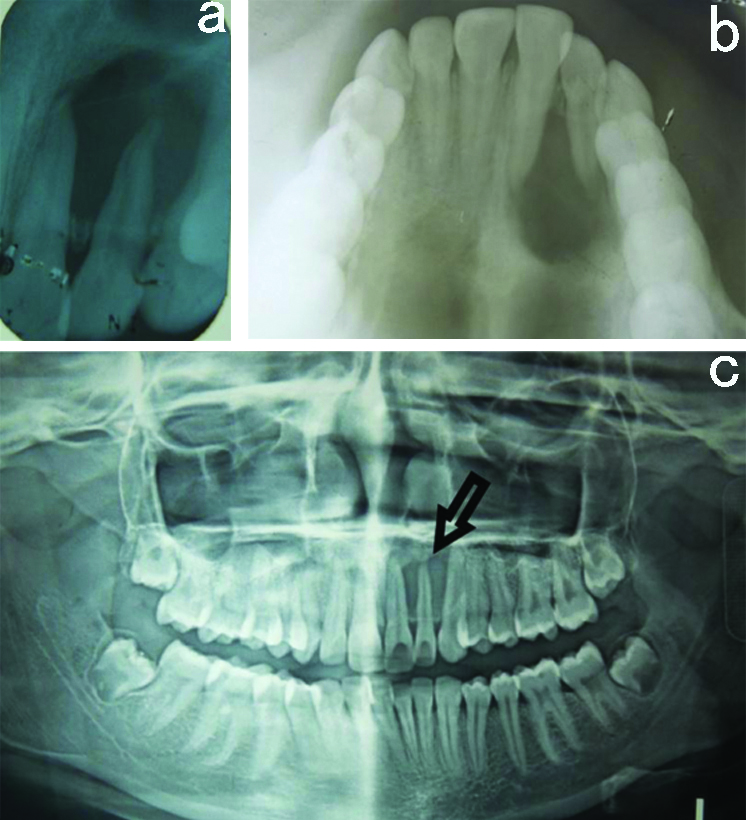
Intraoral examination showed a single localised palatal swelling measuring about 1.0×1.0 cm in relation to tooth #21 and #22, extending from mesial aspect of #21 to distal aspect of #22 which was oval in shape having colour same as that of adjacent mucosa [Table/Fig-2]. No discharge of pus or sinus formation was associated in relation to the same, and swelling was hard and tender on palpation. Thermal pulp testing of the tooth revealed non-vital #21 and #22. No discolouration of the tooth #21 and #22 was observed. An intraoral periapical radiograph, occlusal radiograph and Orthopantomogram (OPG) was advised [Table/Fig-3a-c], which showed well-defined radiolucency in periapical region extending from distal surface of root of #21 to distal surface of root of #22 with apical 0.5-1 mm resorption of apex of #22 and access openings in relation to #21 and #22 done by previous dentist. There was cortical perforation on palatal aspect resulting in swelling. Adjacent teeth showed no root resorption or pathologic migration. Computed Tomography (CT) scan was not done as the patient could not afford it. Cytological findings from aspirated fluid, following Fine Needle Aspiration Cytology (FNAC) showed straw-coloured fluid and presence of chronic inflammatory cells like polymorphs, macrophages and squamous cells. Based on clinical, radiological and FNAC findings, it was diagnosed as Radicular cyst.
Preoperative intraoral photograph showing intraoral swelling in palatal aspect of #21, #22.
a) Preoperative IOPA. b) Occlusal Radiograph. c) Preoperative OPG.
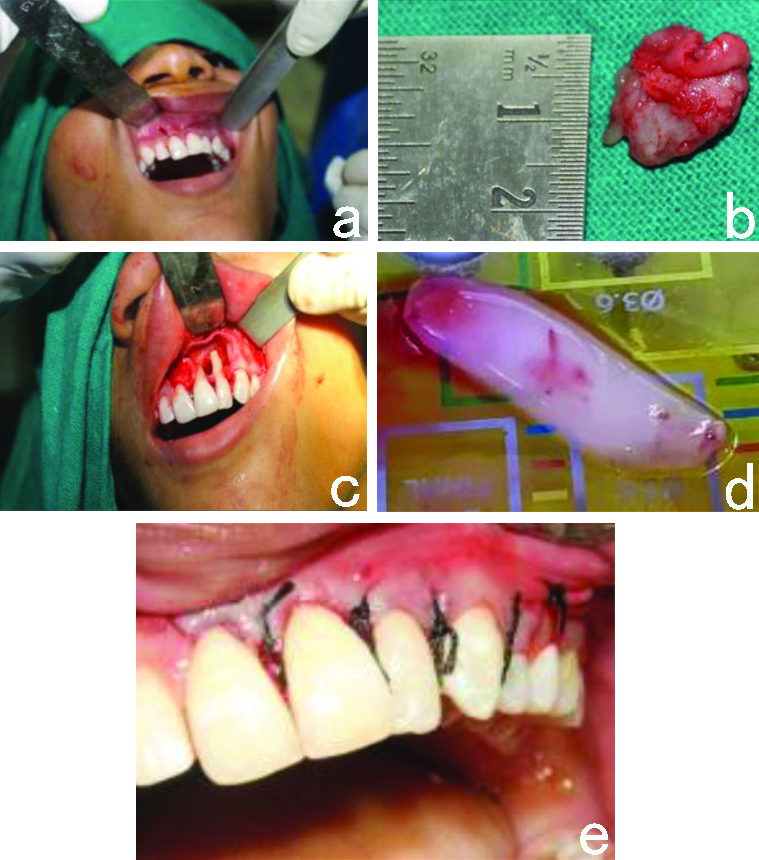
At the first visit, behaviour management and demonstration of brushing technique was taught to the patient. Antibiotics and analgesics were also prescribed. On the basis of diagnosis, further treatment plan was explained to the parents and written consent was obtained to carry out the procedure. Endodontic treatment was performed in tooth number #21 and #22, as access opening was done by the referring dentist, a day prior to reporting, working length was determined (tooth #21-22 mm; #22-20.5 mm). Chemomechanical preparation was performed and calcium hydroxide RC CAL- PRIME denatal products pvt., ltd., was used as intracanal medicament for a week. In subsequent visit, obturation was done using lateral condensation technique with gutta percha. Under Local Anaesthesia (Lignocaine 2%), a full thickness flap was raised through buccal approach followed by cystic enucleation and Apicoectomy in relation to #21 and #22. This was followed by preparation and grafting with PRF from patient’s own blood sample. About 10 ml of blood was drawn in Red Vacutainer Biopro (without any anticoagulant), placed in centrifuge with counter tube containing water, and run at 3000 rpm for 10 minutes. The middle fraction containing the fibrin clot was then collected 2 mm below lower dividing line, to obtain the PRF which was separated and packed into the defect. Six interrupted sutures (3-0 Black Braided Silk) were placed [Table/Fig-4a-e]. Postoperative instructions like care of surgical site, diet, advices on suture removal as well as review visit were given to the patient and medications were prescribed (Antibiotics and Analgesics). The histopathology report revealed cystic cavity lined by non-keratinised stratified squamous epithelium with mixed inflammatory infiltration confirming the provisional diagnosis of an infected radicular cyst. Sutures were removed after one week and postoperative OPG was taken [Table/Fig-5]. During six months follow-up, patient was asymptomatic with complete healing of the lesion [Table/Fig-6].
a) Intraoperative photograph. b) Cyst enucleated during operation. c) Intraoperative photograph showing full thickness flap raised using buccal approach for apicocectomy. d) Intraoperative photograph showing grafting with Platelet Rich Fibrin (PRF). e) Postoperative photograph showing six inturupted sutures.
Postoperative OPG one week after treatment.
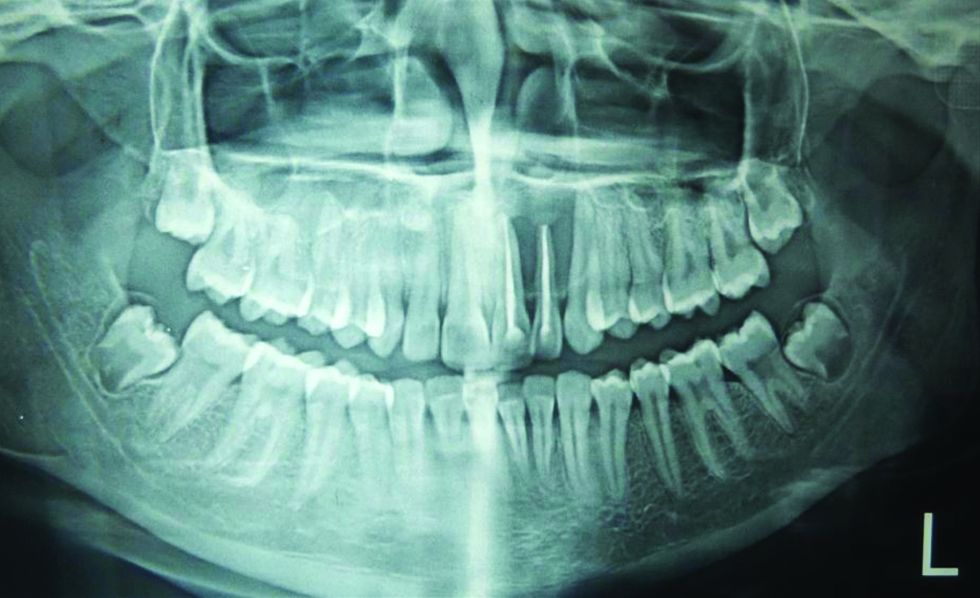
Six months follow-up Photograph showing resolved lesion.

Discussion
Trichotillomania is an obsessive-compulsive disorder characterised by pulling out one’s own hair, resulting in noticeable hair loss from scalp area which may further be infected at the site of torn hair leading to medical complications such as skin irritations or infections. In some severe cases these patients may ingest the hair after pulling and are posed to gastrointestinal complications like hairballs [1]. Method by which individual pulls the hair varies, most commonly, hands, particularly the thumb and forefinger, are used to remove the hair, sometimes tweezers and other cosmetic devices are also used [2]. Prevalence of TTM patients is low, in medical epidemiological surveys it has been as reported to range of 0.6% to 3.6% among adults [3], whereas this increases to 11.03% in young adults in college as reported in literature [4]. In India, the prevalence was reported to be 1.23% [5].
No definite etiology has been confirmed till date for TTM. Some research has drawn conclusion towards stress as main cause for the development of TTM. Appearance of bald spots further exaggerate anxiety and depression state in these patients, and their attempts towards hair pulling increases the chances of becoming a habitual means of coping with stress, further enhancing intra and interpersonal distress. Some authors are inclined towards genetic predisposition of aetiology due to mutation in SLITRK1 gene [6], which plays role in cortex development and neuronal growth. Ultimately, abnormal functioning of the basal ganglia, and frontal lobe dysfunction may result in the habit formation, and habit inhibition, respectively [7]. In such psychological disorders, falls are very common leading to trauma of maxillofacial region.
Treating children with psychiatric disorders is a real challenge to paediatric dentist by applying non-pharmacological and pharmacological behaviour management techniques. Always a positive attitude of dentist with love, and care may alter uncooperative behaviour of these children as they are more affectionate towards empathy and child friendly environment. Also, most of the parents and efficient paediatric dentists prefer non-pharmacological behaviour management techniques under local anaesthesia while treating these patients in minimum invasive manner. The present case was managed successfully by endodontic therapy with thorough debridement and disinfection of the root canal system followed by surgery at chairside, which was carried out under local anaesthesia [8].
Radicular cyst is an inflammatory cystic lesion which develops in the apical tissues as a consequence of an infected and necrotic pulp. Mostly, they are asymptomatic and noticed when teeth with non-vital pulp are subjected to periapical radiographs [9]. Management of large cystic lesion is a subject of debate [10], treatment for large periapical lesions varies from conventional root canal therapy with long-term calcium hydroxide as intracanal medicament to various surgical interventions, whereas endodontists maintain that true cysts can be successfully treated only by surgical means [11,12]. When the size and extent of the lesion is large, to achieve satisfactory healing and good prognosis, surgical management is the treatment of option. Differential diagnosis of Radicular Cyst includes Dentigerous Cysts, Pindborg Tumour, Periapical Cementoma, Traumatic Bone Cyst, Ameloblastoma, Odontogenic Keratocyst and Odontogenic Fibroma [13].
Vidhale G et al., used PRF along with bone graft in his case and showed regenerative potential along with good functional recovery [14]. Autologous PRF is considered as a healing biomaterial. PRF is not only economical but also does not require any biochemical handling of blood [9,14]. Further, its preparation is simple, easy, less time consuming and cost effective. As a by-product of patient’s own blood, the chances of infectious diseases transmission is rare. It promotes more efficient cell migration and proliferation. It also helps in haemostasis [9].
Pedodontist should have thorough knowledge about materials and various treatment options involved in management of patient with TTM. In the present case, after the completion of treatment, patient was given oral hygiene instructions and adviced for routine revisits to dentist for proper maintenance of the oral cavity as a whole.
Conclusion(s)
From this case presentation, authors suggest that PRF is effective clinically and radiographically in the treatment of intrabony defect and more clinical research with long-term follow-up are needed. Also, proper behavior management plays vital role in treating a patient with TTM.
Contribution by the authors: Diagnosis, Treatment Planning and Case designing: SS, VK; Treating Surgeons: VK, SD; Manuscript, Preparation and Editing: VGR, SD.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Dec 21, 2019
Manual Googling: Jul 06, 2020
iThenticate Software: Sep 15, 2020 (13%)
[1]. Franklin ME, Zagrabbe K, Benavides KL, Trichotillomania and its treatment: A review and recommendationsExpert Rev Neurother 2011 11(8):1165-74.10.1586/ern.11.9321797657 [Google Scholar] [CrossRef] [PubMed]
[2]. Woods DW, Wetterneck CT, Flessner CA, A controlled evaluation of acceptance and commitment therapy plus habit reversal for trichotillomaniaBehaviour research and therapy 2006 44(5):639-56.10.1016/j.brat.2005.05.00616039603 [Google Scholar] [CrossRef] [PubMed]
[3]. Christenson GA, Pyle RL, Mitchell JE, Estimated lifetime prevalence of trichotillomania in college studentsJ Clin Psychiatry 1991 52(10):415-17. [Google Scholar]
[4]. Hajcak G, Franklin ME, Simons RF, Keuthen NJ, Hairpulling and skin picking in relation to affective distress and obsessive-compulsive symptomsJ Psychopathol Behav Assess 2006 28(3):177-85.10.1007/s10862-005-9001-x [Google Scholar] [CrossRef]
[5]. Malhotra S, Grover S, Baweja R, Bhateja G, Trichotillomania in childrenIndian paediatrics 2008 45(5):403 [Google Scholar]
[6]. Ozomaro U, Cai G, Kajiwara Y, Yoon S, Makarov V, Delorme R, Characterisation of SLITRK1 variation in obsessive-compulsive disorderPloS one 2013 8(8):e7037610.1371/journal.pone.007037623990902 [Google Scholar] [CrossRef] [PubMed]
[7]. Schreiber LR, Odlaug BL, Grant JE, Diagnosis and treatment of trichotillomaniaNeuropsychiatry 2011 1(2):123-32.10.2217/npy.11.8 [Google Scholar] [CrossRef]
[8]. Appukuttan DP, Strategies to manage patients with dental anxiety and dental phobia: Literature reviewClin Cosmet Investig Dent 2016 8:35-50.10.2147/CCIDE.S6362627022303 [Google Scholar] [CrossRef] [PubMed]
[9]. Pradeep K, Kudva A, Narayanamoorthy V, Cariappa KM, Saraswathi MV, Platelet-rich fibrin combined with synthetic nanocrystalline hydroxy apatite granules in the management of radicular cystNiger J Clin Pract 2016 19(5):688-91.10.4103/1119-3077.18871127538563 [Google Scholar] [CrossRef] [PubMed]
[10]. Gallego DR, Torres DL, GarcIa MC, Romero MR, Infante PC, Gutiérrez JP, Differential diagnosis and therapeutic approach to periapical cysts in daily dental practiceMedicina oral: Organo oficial de la Sociedad Espanola de Medicina Oral y de la Academia Iberoamericana de Patologia y Medicina Bucal 2002 7(1):54-58. [Google Scholar]
[11]. Nair PN, Sjögren U, Schumacher E, Sundqvist G, Radicular cyst affecting a root-filled human tooth: A long-term post-treatment follow-upInt Endod J 1993 26(4):225-33.10.1111/j.1365-2591.1993.tb00563.x8225641 [Google Scholar] [CrossRef] [PubMed]
[12]. Lin LM, Ricucci D, Lin J, Rosenberg PA, Nonsurgical root canal therapy of large cyst-like inflammatory periapical lesions and inflammatory apical cystsJ Endod 2009 35(5):607-15.10.1016/j.joen.2009.02.01219410070 [Google Scholar] [CrossRef] [PubMed]
[13]. Deshmukh J, Shrivastava R, Bharath KP, Mallikarjuna R, Giant radicular cyst of the maxillaCase Reports 2014 2014:bcr201420367810.1136/bcr-2014-20367824792022 [Google Scholar] [CrossRef] [PubMed]
[14]. Vidhale G, Jain D, Jain S, Godhane AV, Pawar GR, Management of radicular cyst using platelet-rich fibrin & iliac bone graft-A case reportJ Clin Diagn Res 2015 9(6):34-36.10.7860/JCDR/2015/13368.613626266233 [Google Scholar] [CrossRef] [PubMed]