Shoulder pain is a significant cause of decreased functional activity of an individual. The overall prevalence of shoulder pain is 16-26%, which makes it the third most common cause among musculoskeletal complaints [1]. The shoulder pathologies are diverse with the most common ones being rotator cuff tears, labral injuries, adhesive capsulitis, impingement syndrome and instability. The cause of pain in the shoulder is often difficult to evaluate, and diagnosis is usually ambiguous because physical findings are poorly reproducible. The diagnosis therefore requires multiple imaging modalities to assist in the identification of the underlying pathologic conditions. These imaging modalities include plain radiographs, arthrography, ultrasonography and MRI. The advantages of MRI over the other imaging modalities includes its non invasive nature, provision of superior soft tissue contrast and spatial resolution for assessing tendons and ligaments and therefore, is considered to be an effective tool for evaluation of the shoulder where the common pathology involves the tendons and ligaments. MRI is a time proven sensitive, accurate, cost-effective and a non invasive tool in investigating shoulder pathology [2]. The disadvantages with the MRI include its contraindications in patients with metallic foreign bodies inside the body like certain ferromagnetic orthopaedic implants, cochlear implants, and cardiac pacemakers. The other important disadvantage is for its use in children where sedation becomes necessary and in claustrophobic patients. In addition, the MRI is a comparatively expensive investigation in comparison to other imaging modalities.
Magnetic resonance arthrography, with intra-articular injection of gadolinium as a contrast medium, however has been found to be more accurate than MRI [3-5], alone in the diagnosis of labral pathologic conditions in the shoulder, but, this conflicts with a major advantage of MRI-its non invasive nature [6]. The accuracy of MRI of the shoulder has been found to be both reader and operator-dependent. Also, the effectiveness of MRI for the diagnosis of shoulder disease is dependent on the nature of the pathologic abnormality. There is a conflict regarding the accuracy of MRI in detection of shoulder pathology in literature with certain studies indicating that MRI is very accurate in the identification of rotator cuff tears [6], Bankart’s lesion [7] and osteochondral defects but was not found to be helpful in diagnosing SLAP lesions [8], whereas there are other studies which do not consider MRI as a reliable tool for the definitive diagnosis of shoulder pathology particularly in cases where clinical examination is ambiguous [6,9,10]. In addition to the above, a study conducted by Muthami KM et al., considered a need of investment in the proper training of musculoskeletal radiologists in developing countries [11]. Therapeutic arthroscopy is “the current gold standard” for diagnosing shoulder pathologies. It provides an enhanced 20 power magnification of the shoulder joint [12]. However, arthroscopy is an invasive intervention that requires hospitalisation and anaesthesia, and hence can present with all the potential complications associated with a surgical procedure such as, infection, nerve injuries particularly axillary nerve and musculocutaneous nerve injuries, fluid extravasation, glenohumeral chondrolysis, anaesthesia-related complications, thromboembolic risks and huge financial costs to the patient [13].
The purpose of this study was to correlate the findings of MRI shoulder with the shoulder arthroscopy findings and to determine the sensitivity, specificity, and accuracy of MRI diagnosis of various shoulder pathologic conditions. The effectiveness of shoulder MRI as a preoperative diagnostic tool in the evaluation of the painful shoulder was also evaluated.
Materials and Methods
This cohort study was conducted at a tertiary care Orthopaedics Hospital in Srinagar, Jammu and Kashmir, India, from September 2017 to March 2020 after prior approval by the Institutional Ethical Committee. (GMCE-10445). A total of 42 patients were included in the study. All patients in the age group of 18-80 years that presented to the hospital with chief complaints of chronic shoulder pain for a period of more than six weeks, having symptoms of instability, clinical signs of tear, impingement or functional limitation of the affected shoulder were included in the study. All the patients were thoroughly evaluated clinically before proceeding for MRI and arthroscopy. Exclusion criteria were patients with active infection, rheumatoid arthritis and osteoarthritis.
The findings on clinical examination were documented and a provisional diagnosis was made. The differential diagnosis included subacromial impingement syndrome, glenoid labrum abnormalities, partial or complete tears of the rotator cuff, SLAP tears, glenohumeral osteoarthritis, acromioclavicular joint arthritis, biceps tendinitis, synovial chondromatosis, adhesive capsulitis, and glenohumeral instability. These patients had already undergone an exhaustive program of conservative management for a minimum period of six months including the use of Non Steroidal Anti-Inflammatory Drugs (NSAIDs), activity modification, physiotherapy, and intra-articular steroid injections. All patients were subjected to MRI shoulder which was reported by a single radiologist. The details of clinical examination were provided to the radiologist conducting MRI to help with the diagnosis. The findings were documented and the patients were advised arthroscopic exploration and subsequent therapeutic procedure. The patients were subjected to arthroscopy of the shoulder joint after obtaining written consent, required investigations and properly explaining the risks associated with the surgical procedure. Shoulder arthroscopy was done by a single experienced orthopaedic surgeon with standard posterior arthroscopic portals and anterior instrument portals. Arthroscopic exploration of the glenohumeral joint and subacromial space was undertaken in those patients.
Statistical Analysis
Arthroscopy was designated as the standard of reference for the diagnosis of shoulder disease. After the surgical procedure, the arthroscopic findings were documented and correlated with the MRI findings and subsequently the sensitivities, specificities and accuracy of MRI were determined. The data collected was presented in the form of tables and calculated as true positives, true negatives, false positives and false negatives. Further calculations were done for sensitivity, specificity, Positive Predictive Value (PPV) and Negative Predictive Value (NPV). Data was analysed and calculations were done using OpenEpi programs. (https://www.openepi.com/DiagnosticTest/DiagnosticTest.htm).
Results
Demographic data showing the number and percentage of patients affected in various age groups, sex distribution and side distribution and occupational involvement are depicted in [Table/Fig-1]. Majority of patients were rural housewives that were involved in heavy household work and farming. Rotator cuff tear and subacromial bursitis were the most common shoulder pathology [Table/Fig-2]. No differentiation was made whether rotator cuff tear was partial or full thickness and whether it was acute, subacute or chronic tear. At arthroscopic evaluation, there were 26 rotator cuff tears. Among them only 24 tears were correctly identified by MRI. The resulting sensitivity, specificity and accuracy of MRI were 0.92, 0.81 and 0.88, respectively [Table/Fig-3].
Demographic data showing various age groups, side, sex and occupational involvement.
| Variables | Number of patients n (42) | Percentage (%) |
|---|
| Age group (years) |
| 18-40 | 8 | 19.2 |
| 41-60 | 11 | 26.1 |
| 61-80 | 23 | 54.7 |
| Side involved |
| Right | 29 | 69 |
| Left | 13 | 31 |
| Sex |
| Male | 16 | 38.1 |
| Female | 26 | 61.9 |
| Occupation |
| Housewives | 16 | 38.1 |
| Farmer | 9 | 21.4 |
| Labourer | 6 | 14.3 |
| Student | 5 | 11.9 |
| Teacher | 3 | 7.1 |
| Banker | 1 | 2.3 |
| Tailor | 1 | 2.3 |
| Contractor | 1 | 2.3 |
Most common pathologies of the shoulder involved.
| Pathology | MRI (n,%) | Arthroscopy (n,%) |
|---|
| Rotator cuff tear | 27 (64.3) | 26 (61.9) |
| Subacromial bursitis | 22 (52.4) | 26 (61.9) |
| Bankart’s lesion | 10 (23.8) | 9 (21.4) |
| SLAP tear | 4 (9.5) | 7 (16.7) |
| Synovial chondromatosis | 5 (11.9) | 5 (11.9) |
Interpretation of statistical data.
| Pathology | TP | FN | TN | FP | Sensitivity | Specificity | PPV | NPV | Accuracy |
|---|
| Rotator cuff tear | 24 | 2 | 13 | 3 | 0.92 | 0.81 | 0.88 | 0.87 | 0.88 |
| Subacromial bursitis | 19 | 7 | 13 | 3 | 0.73 | 0.81 | 0.86 | 0.65 | 0.76 |
| Bankart’s lesion | 8 | 1 | 31 | 2 | 0.88 | 0.94 | 0.8 | 0.96 | 0.92 |
| SLAP tear | 2 | 5 | 33 | 2 | 0.28 | 0.94 | 0.5 | 0.86 | 0.83 |
| Synovial chondromatosis | 4 | 1 | 36 | 1 | 0.8 | 0.97 | 0.8 | 0.97 | 0.95 |
TP: True positives; TN: True negatives; FP: False positives; FN: False negatives; PPV: Positive predictive value; NPV: Negative predictive value; SLAP: Superior labrum anterior posterior
Similarly, 26 cases of subacromial bursitis were identified on arthroscopy of which only 19 cases were correctly reported by MRI. The resulting sensitivity, specificity and accuracy of MRI were 0.73, 0.81 and 0.76, respectively. Therefore, the sensitivity of MRI in diagnosing subacromial effusion or bursitis is significant less than its sensitivity in diagnosing rotator cuff tears. In identifying Bankart’s lesion, MRI identified 8 patients with the lesion among 9 patients that were found to have the lesion on arthroscopy. The resulting sensitivity, specificity and accuracy of MRI were 0.88, 0.94 and 0.92, respectively. However, in case of SLAP tears, only two patients with SLAP tears were correctly identified on MRI among seven patients who were diagnosed with the same on arthroscopy. So the sensitivity of MRI in case of detecting SLAP lesions was only 0.28. Despite the low sensitivity, MRI was highly specific (0.94) and accurate (0.83). The other important pathology was synovial chondromatosis where four patients were accurately identified on MRI among five patients who were diagnosed on arthroscopy. So, overall MRI is highly specific and accurate for all the shoulder pathologies identified above, but the sensitivity is far less when it comes to diagnosing SLAP tears.
Discussion
The aim of this study was to correlate the findings of MRI shoulder with the findings of shoulder arthroscopy and it was found that MRI shoulder is a reliable tool in the diagnosis of shoulder pathologies like subacromial bursitis, rotator cuff tears, bankart’s lesion, synovial chondromatosis whereas its reliability is questionable when it comes to diagnosing SLAP tears.
Rotator Cuff Tear
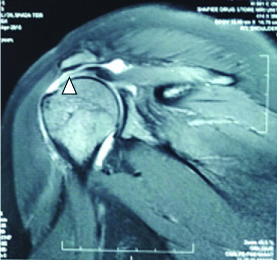
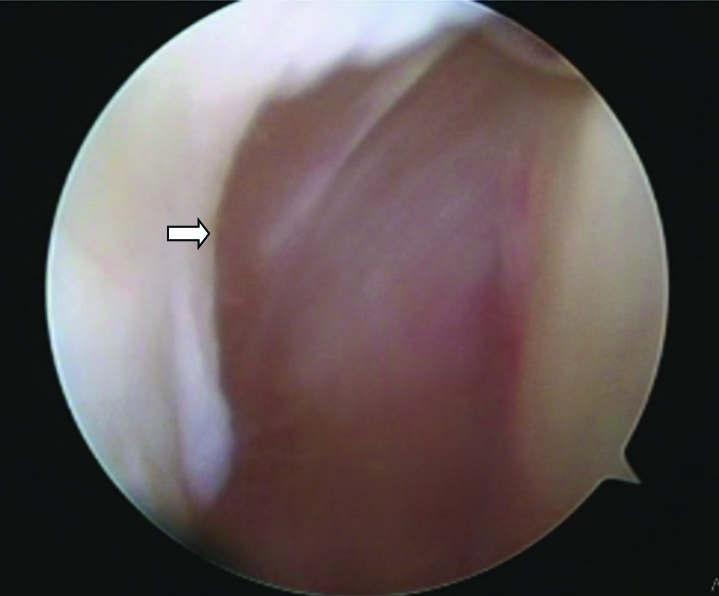
The sensitivity and specificity of MRI shoulder in diagnosing rotator cuff tears in this study [Table/Fig-4,5 and 6] [8,11,14] was comparable to other studies with the exception of Muthami KM et al., that showed a sensitivity of 0.46 [11].
MRI showing full thickness tear (white arrowhead) and retraction of supraspinatus tendon insertional foot print with proximal migration of humeral head.

MRI T2 Coronal section showing full thickness tears of supraspinatus tendon (arrowhead) at its insertional foot print.
Arthroscopic image showing large rotator cuff tear (white arrow).
Muthami KM et al., has attributed several reasons to low sensitivity:
Lack of adequate time for proper evaluation of details noted in shoulder MRI.
Use of low Tesla (1.5T) at some centers.
Lack of dedicated musculoskeletal radiologists.
MRI over-diagnosis can be because of the presence of intratendinous tears [6], tendon articular surface tears [11], and supraspinatus tendon being obliquely oriented to the imaging plane [15].
In this study, two rotator cuff tears were missed by MRI whereas three tears were wrongly attributed by MRI and were not found on arthroscopy.
Bhatnagar A et al., and De Mulder K et al., in their studies found that rotator cuff tear was the most common cause of shoulder pain [8,16]. However in this study along with rotator cuff tear, subacromial bursitis was the other most common shoulder pathology.
Subacromial Bursitis
This study was highly sensitive (0.73) and specific (0.81) in diagnosing subacromial bursitis [Table/Fig-7]. It was consistent with other studies [17-19]. However, in one study sensitivity was found to be low (0.50) [17].
MRI T2 sagittal section showing subacromial bursitis (arrowhead).

Reason for low sensitivity is that many asymptomatic shoulders present with fluid in subacromial bursa [20-23].
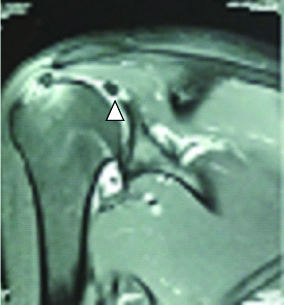
Bankart’s Lesion
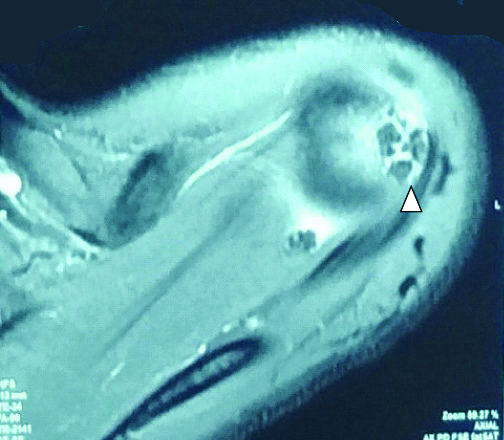
Bankart’s lesion too was diagnosed with high sensitivity (0.88) and specificity (0.94) in the study [Table/Fig-8] which was consistent with the studies conducted by Joshi UP and Puri S and Bhatnagar A et al., however sensitivity was low (0.50) in the study conducted by Momenzadeh OR et al., [7,8,24].
MRI T2 Axial cut showing Bankart’s lesion (arrowhead).
Close proximity of the labrum and capsule with wide variation in type and position of a Bankart’s lesion were the reasons for low sensitivity of MRI in detecting these lesions [25].
SLAP Tear
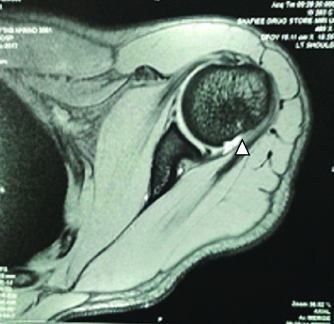
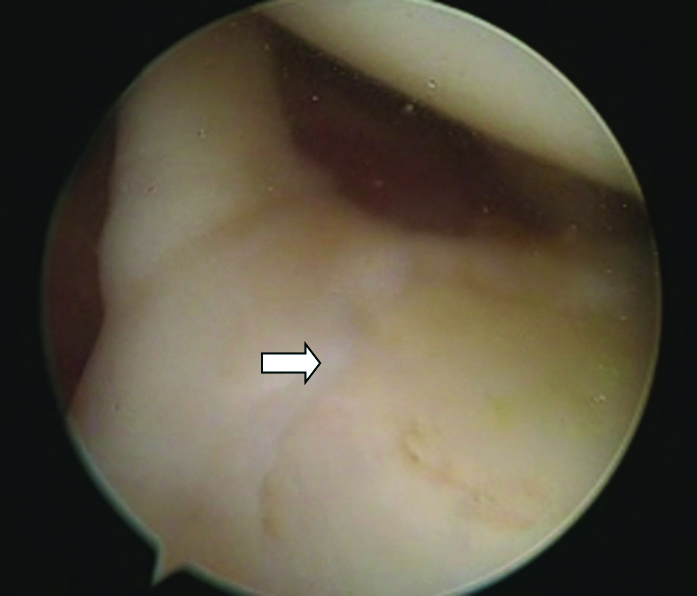
The sensitivity for diagnosing SLAP tear [Table/Fig-9,10] was low (0.28) which was consistent with the study conducted by Bhatnagar A et al., however in the studies conducted by Momenzadeh OR et al., and Iqbal HJ et al., sensitivity was 0.95 and 0.74, respectively [8,24,26]. Overall, the specificity (0.94) was high which was consistent with the other studies [8,24,26].
MRI T2 Coronal section showing suspected SLAP tear (arrowhead).
Arthroscopic image showing SLAP tear (type 1) (white arrow).
The probable reasons that the SLAP tears were missed on MRI may be because these lesions are very small, therefore inadequate spatial resolution may cause them to go undetected [27], and the course of glenoid labrum is curved along the glenoid surface, and coronal oblique images are typically not oriented along the long axis of the glenoid, which can lead to partial volume averaging with adjacent fluid and tissues, limiting accuracy [15,28,29].
Synovial Chondromatosis
In this study, MRI was found to be a highly sensitive (0.80) and specific (0.97) investigation in diagnosing this condition. This was consistent with the work of Momenzadeh OR et al., [30] who found comparable results [Table/Fig-11].
MRI T2 Axial section showing synovial chondromatosis (arrowhead) of shoulder joint.
The sensitivity of MRI in detecting shoulder pathologies varied from poor (0.28) for SLAP lesion to very good (0.88) for Bankart’s tear and (0.80) for synovial chondromatosis to excellent for rotator cuff tears (0.92). Although sensitivity of MRI was variable for different shoulder pathologies, specificity was comparatively high in detecting all of the above shoulder pathologies. [Table/Fig-12] shows the comparison of statistical results of present study with other studies [7,8,11,14,17-19,24,26,30].
Comparison of statistical results of present study with literature [7,8,11,14,17-19,24,26,30].
| Rotator cuff tears | SS | SP | PPV | NPV | ACC |
|---|
| Bhatnagar A et al., [8] | 0.91 | 1.0 | 1.0 | 0.63 | 0.9 |
| Muthami KM et al., [11] | 0.46 | 0.88 | 0.71 | 0.72 | - |
| Naqvi GA et al., [14] | 0.91 | 0.84 | 0.92 | 0.84 | 0.89 |
| Present study | 0.92 | 0.81 | 0.88 | 0.87 | 0.88 |
| Subacromial bursitis | SS | SP | PPV | NPV | ACC |
| Monu JU [17] | 0.5 | 1.0 | 1.0 | 0.81 | 0.84 |
| Malhi AM and Khan R [18] | 0.84 | 0.76 | 0.83 | 0.78 | - |
| Sabharwal T et al., [19] | 1.0 | 0.98 | 0.75 | 1.0 | 0.98 |
| Present study | 0.73 | 0.81 | 0.86 | 0.65 | 0.76 |
| Bankart’s lesion | SS | SP | PPV | NPV | ACC |
| Joshi UP and Puri S [7] | 0.91 | 0.86 | 0.95 | 0.75 | 0.9 |
| Bhatnagar A et al., [8] | 0.8 | 1.0 | 1.0 | 0.89 | 0.9 |
| Momenzadeh OR et al., [24] | 0.5 | 0.84 | 0.77 | 0.6 | - |
| Present study | 0.88 | 0.94 | 0.8 | 0.96 | 0.92 |
| SLAP tear | SS | SP | PPV | NPV | ACC |
| Bhatnagar A et al., [8] | 0.15 | 0.96 | 0.67 | 0.69 | 0.7 |
| Momenzadeh OR et al., [24] | 0.74 | 0.8 | 0.78 | 0.76 | - |
| Iqbal HJ et al., [26] | 0.95 | 0.85 | 0.84 | 0.96 | - |
| Present study | 0.28 | 0.94 | 0.5 | 0.86 | 0.83 |
| Synovial chondromatosis | SS | SP | PPV | NPV | ACC |
| Momenzadeh OR et al., [30] | 0.91 | 0.91 | 0.66 | 0.98 | - |
| Present study | 0.8 | 0.97 | 0.8 | 0.97 | 0.95 |
SS: Sensitivity; SP: Specificity; PPV: Positive predictive value; NPV: Negative predictive value; ACC: Accuracy; SLAP: Superior labrum anterior posterior
The PPV of MRI in present study was 0.88 (88%), 0.86 (86%), 0.8 (80%) in detecting rotator cuff tears, subacromial bursitis, Bankart’s lesion and synovial chondromatosis respectively. Hence MRI was found to be useful in confirming clinical diagnosis of these pathologies. The PPV for SLAP tear was 0.50 (50%), which shows that MRI isn’t as reliable to confirm clinical diagnosis of SLAP tear as it is for diagnosing the other above pathologies.
The NPV of MRI in this study was 0.65 (65%) for subacromial bursitis which was slightly low and implies that MRI should not be routinely used to rule out this shoulder pathology. Whereas, NPV of MRI was 0.97 (97%), 0.96 (96%), 0.87 (87%), 0.86 (86%) for synovial chondromatosis, Bankart’s tear, rotator cuff tear, and SLAP tear, respectively, that shows that MRI could be helpful to rule out the above shoulder pathologies.
The accuracy of MRI was highest (0.95) in diagnosing synovial chondromatosis, followed by bankart’s lesion (0.92), and rotator cuff tear (0.88). Accuracy of MRI was on the lower side when diagnosing SLAP tears (0.83) and subacromial bursitis (0.76).
The clinical findings and provisional diagnosis were provided to the radiologist in each case, which probably was one of the reasons for high accuracy of MRI. Therefore, clinical evaluation and provision of those clinical findings to the radiologist could improve the accuracy of MRI in the diagnosis of shoulder pathology.
Limitation(s)
This study was limited by the facts that MRI shoulder is an expensive investigation which cannot be afforded by some patients and it is difficult to persuade some patients to undergo an invasive procedure like shoulder arthroscopy.
Conclusion(s)
As far as the results are concerned, MRI is a very useful and effective tool in diagnosing various shoulder pathologies with exception of SLAP tears where its sensitivity diminishes significantly. But the drawbacks with MRI included a good proportion of false negative and false positive cases which diminish its overall accuracy. The proportion of false negative results was 16.6% and 11.9% in cases with subacromial effusion and SLAP tears, respectively. Therefore, there is a need of more investment in the training of musculoskeletal radiologists and procurement of higher magnetic field MRI’s to improve the diagnostic accuracy of MRI shoulder.
Since arthroscopy remains the gold standard for diagnosing soft tissue shoulder pathologies with very high accuracy, it is important that one should proceed to arthroscopy after taking an MRI which gives us a better idea of concerned pathology and the need for operative intervention. This is particularly important in set ups where there are large waiting lists for elective surgeries.
TP: True positives; TN: True negatives; FP: False positives; FN: False negatives; PPV: Positive predictive value; NPV: Negative predictive value; SLAP: Superior labrum anterior posterior