Pyogenic granuloma is a misnomer, as in reality it arises in response to various irritating factors such as low-grade local irritation or hormonal factors, traumatic injury as well as presented as inflammatory hyperplasia that is not related to infection. Oral pyogenic granuloma is a lobulated or smooth exophytic lesion with pedunculated or sometimes sessile base, haemorrhagic in tendency. Although excisional surgery is the treatment of choice for it, some other treatment protocols such as laser therapy, sclerotherapy with 3% polidocanol, cryotherapy and steroid therapy have also been proposed. Here, Authors present a case series of gingival as well as extra gingival pyogenic granulomas which were diagnosed and treated by various therapies i.e., surgical excision, Carbon Dioxide (CO2) laser therapy and sclerotherapy. Regression period of lesion with different therapies was evaluated in detail. Maximum patients were female in the age group of 26-50 years in present case series. Almost all cases of pyogenic granuloma had typical clinical characteristic without bony alteration. Amongst all therapies sclerotherapy had the biggest advantage of less regression period for any case of pyogenic granuloma i.e., 7-8 days only.
Introduction
Pyogenic granuloma presented as a non neoplastic, benign, soft tissue lesion that arises in response to various irritating factors such as low-grade local irritation, hormonal factor, traumatic injury and presented as inflammatory hyperplasia that is not related to infection [1]. Irritational factors responsible for pyogenic granuloma includes tooth brush trauma, flecks of calculus or foreign material within the gingival crevice that contributes to exuberant proliferation of connective tissue [2,3]. In oral cavity pyogenic granuloma appears as an exophytic, elevated, smooth, sessile or pedunculated growth usually covered by yellow fibrinous membrane with red erythematous lobulated and warty surface sometimes showing ulcerations. Radiographic findings are usually absent in pyogenic granuloma. Sometimes localised alveolar bone resorption in rare instances of large and long-standing gingival tumours can be seen [2-5].
Excisional biopsy is the recommended treatment of such type of lesion unless it would produce a marked deformity [6]. Along with removal of irritants such as plaque, calculus and foreign materials through scaling and root planning of adjacent teeth, conservative surgical excision or other treatment modalities such as Sclerotherapy, Nd:YAG laser, CO2 laser is recommended for the management of this lesion [7-9]. Here, Authors have presented a case series of gingival as well as extra gingival pyogenic granulomas which were diagnosed and treated by various therapies i.e., surgical excision, CO2 laser therapy and sclerotherapy.
Case Description
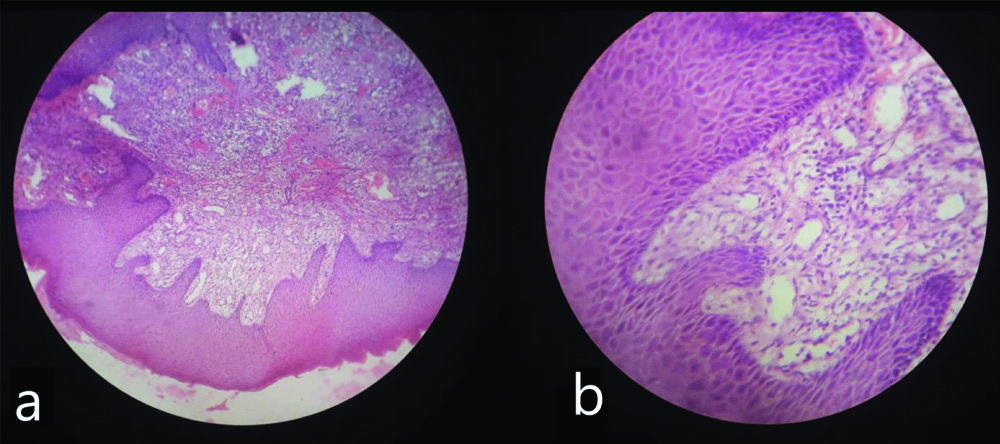
The present case series includes 21 cases of gingival as well as extra gingival pyogenic granulomas histopathologically. Out of 21 cases, 19 cases were of gingival pyogenic granuloma and two cases were of extra gingival pyogenic granuloma. Complete case history and clinical examination was done thoroughly. Various clinical findings such as colour (red/purple), base (sessile/pedunculated), surface (smooth/lobulated), size (few mm to cm) and extension were recorded in detail. Routine haemogram and random blood sugar was done in all patients. Radiographs (IOPA) were done to rule out any bony involvement because of pressure resorption. Under local anaesthesia, incisional biopsies were performed in all cases for histopathologic confirmation [Table/Fig-1a,b]. After histopathological confirmation, patients were selected either for CO2 laser, surgical excision, sclerotherapy using 3% Polidocanol depending upon site, size, bleeding tendency, consistency of the lesion.
a) Histopathological features showing hyperplastic surface epithelium with vascular proliferation and mixed inflammatory cells, H&E ×100; b) Histopathological features showing small and large endothelium-lined channels and mixed inflammatory cell infiltrate, H&E ×400.
Out of 21 cases, two cases were treated by CO2 laser, seven cases were treated by surgical excision, and 12 cases including extra gingival pyogenic granuloma (two cases) were treated by sclerotherapy. CO2 laser therapy was done only in small sized lesion with less chances of bleeding as well as easy accessibility. Surgical excision was done only in those cases having, fibrotic consistency without bleeding tendency. Sclerotherapy was done in majority of cases irrespective of site and size of lesion. The naive lesions having soft consistency and chances of more bleeding were treated by this therapy.
a) Preoperative lesion present in mandibular lingual aspect (unusual site) and size of greater than 4 cm (unusual size) treated by surgical excision; and b) Postoperative.
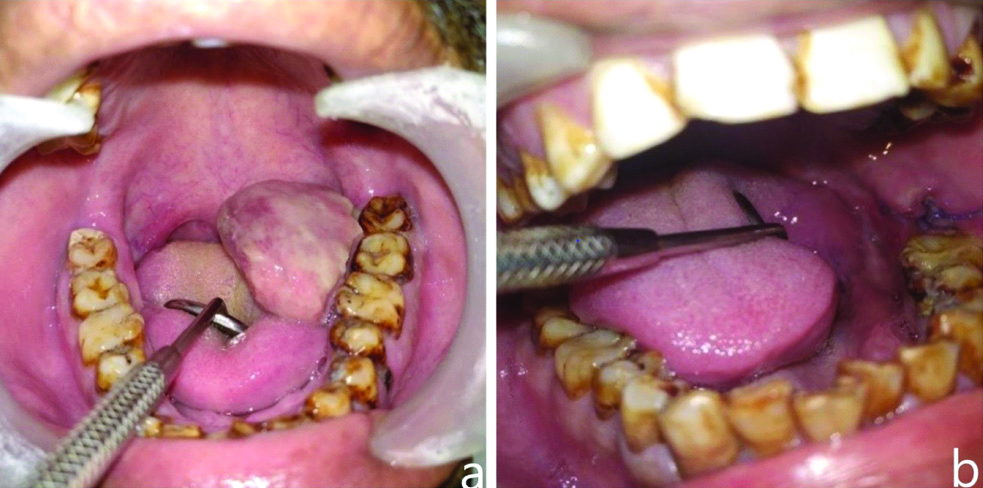
Out of 21 cases seven cases were treated by surgical excision, six cases were located in posterior segment of maxilla and mandible and only one case was in anterior segment. Under aseptic conditions and antibiotic coverage, excision of the lesion was carried out under local anaesthesia of 2% lignocaine hydrochloride with epinephrine (1:100,000) using a scalpel and blade, followed by curettage and thorough scaling of the involved teeth. Sutures (3-BBS) were taken only in lingual pyogenic granuloma due to larger size and more bleeding tendency. All patients were relieved after ensuring complete haemostasis. The patients were advised to use topical antiseptic gel at the site of surgery. Postoperative antibiotics, analgesics, and maintenance of oral hygiene were advised in all cases. First follow-up was done after three days and subsequent weekly follow-up were done. Complete healing was noted in 12-15 days in anterior region and 15-20 days in posterior region.
a) Preoperative lesion in maxillary anterior region treated by CO2 laser; and b) Postoperative.
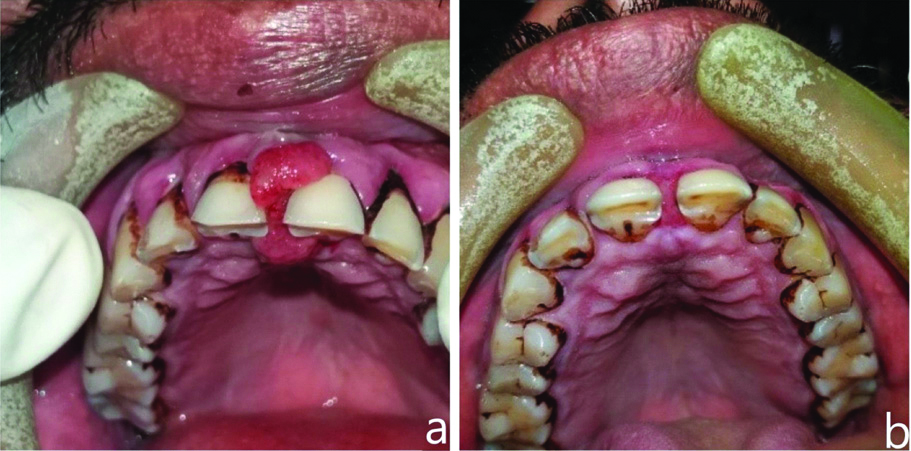
Out of 21 cases CO2 laser therapy was done in two cases of pyogenic granuloma situated at maxillary anterior region having 2 cm size without bleeding tendency. After adequate anaesthesia, the lesion or growth was grasped with Allis tissue holding forceps and raised from its base. The excision procedure was performed from the base of the mass from all the direction in slow and controlled fashion using continuous wave irradiation of wavelength 10600 nm at 10-15W in non contact mode, until removed completely. No suturing was required after laser surgery. All patients were instructed to avoid hard food, smoking/tobacco use. Oral rinse with chlorhexidine mouthwash (0.12%) was prescribed. First follow-up was done after three days and showed complete healing in 10-12 days noted in periodic visits.
a) Preoperative lesion with haemorrhagic tendency situated over maxillary posterior region treated by sclerosing agent Polidocanol 3%; and b) Postoperative picture showing resolution of lesion; c) Preoperative lesion of extra gingival pyogenic granuloma presented on hard palate treated by sclerosing agent-Polidocanol 3%; d) Postoperative image showing resolution of lesion.
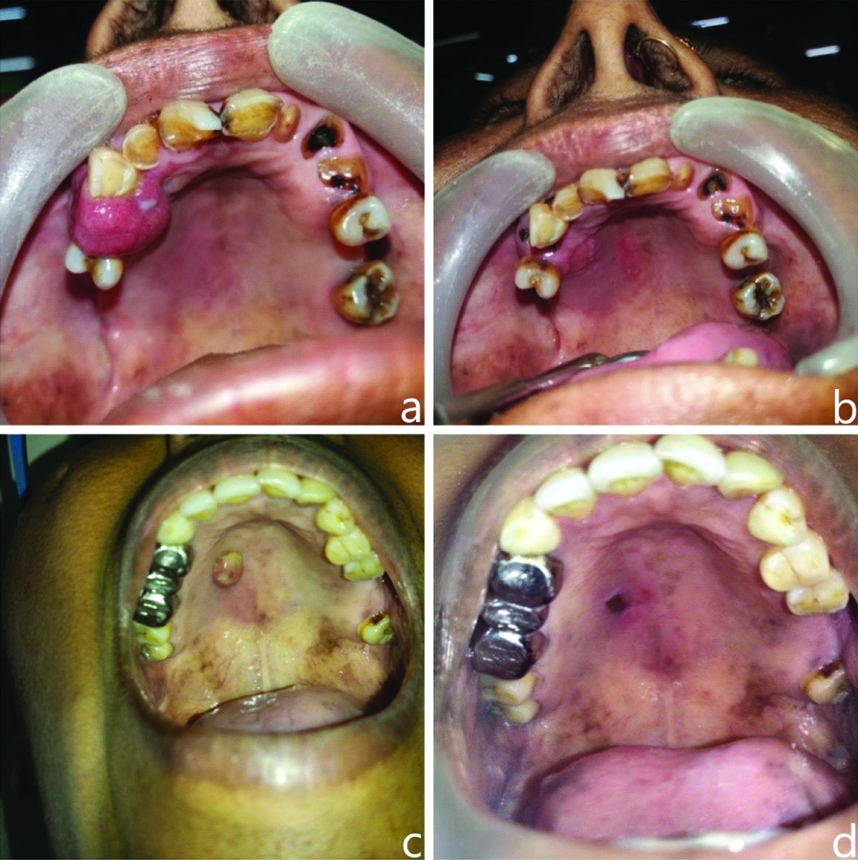
Out of 21 cases, 12 cases including extra gingival pyogenic granuloma were treated by sclerotherapy irrespective of site and size. Out of 12 cases, two cases each on maxillary anterior and posterior, four cases were present over mandibular anterior, two cases were present over mandibular posterior and two cases were present over hard palate of different sizes. All patients were subjected to a patch test to rule out any hypersensitivity reaction to the sclerosing agent. No patient had an allergy to polidocanol. After applying the surface local anaesthesia (Lignocaine Hydrochloride gel 5%) over the lesion, and under aseptic conditions, 0.5-1 mL of 3% polidocanol (Asklerol marketed Samarth Life Sciences Pvt., Ltd.,) was slowly injected by insulin syringe in a circumferential manner around the lesion until the solution leaked out from the surface of the lesion. The puncture site was gently compressed for five minutes with gauze. All patients were instructed to avoid hard food, smoking/tobacco use. Oral rinse with chlorhexidine mouthwash (0.12%) was prescribed. Regular follow-ups were done at 24 hours, seven days, and 15 days at weekly intervals up to one month to evaluate the response until the lesions became necrotic and exfoliated. Out of 12, 10 lesions (size up to 2 cm) were regressed with only one injection within 7-8 days. In two cases (size more than 3 cm) second injection was given after seven days and the lesions regressed completely within 15 days.
Irrespective of therapy all the patients were instructed for maintenance of oral hygiene and were evaluated after one, three and six months periodically to know any complications or recurrence.
Discussion
The first case of pyogenic granuloma in English literature is described by Hullihen in 1844 and termed as “botryomycosis hominis” in 1897. The current term of “pyogenic granuloma” or “granuloma pyogenicum.” has been given by Hartzell in 1904, so called as Crocker and Hartzell’s disease [4]. The inflammatory gingival hyperplasia and oral pyogenic granuloma were the most common diagnosis of gingival and alveolar hyperplastic reactive lesions observed in clinicopathological study conducted by Kamal R et al., [10]. Khaitan T et al., (2013) treated four cases of oral pyogenic granuloma by using sclerosing agent. Pyogenic granuloma presented on other dermatological sites treated with sodium tetradecyl sulfate by Moon SE et al., (2005) showed excellent results. Rahman H, (2014) showed complete resolution in a case of pyogenic granuloma of scalp with no recurrence [8,11,12].
In the current study [Table/Fig-5], approximately 66% of lesions were found in the second, third, and fourth decades of life showing female predominance as reported by other studies [1-7,13-15]. Various local factors such as plaque and calculus accumulation, crowding of teeth in 19 cases (90.47%), four cases of traumatic factors (19.04%) such as tooth brush and toothpick trauma, overhanging restorations, constant irritation from tooth as well as oral adverse habit in four cases (19.04%) such as tobacco or non tobacco related habit and hormonal disturbances in 14 cases (66.66%) were the main aetiological factor as shown in [Table/Fig-6]. Hormonal imbalance has definite role in pyogenic granuloma as all female patients (100%) had history of hormonal alteration that may evoke an exaggerated proliferative response of connective tissue resulting in the angiogenesis and formation of pyogenic granuloma [16,17]. Angiogenesis is involved in the pathogenesis of pyogenic granuloma and may result from the activation of Mitogen-Activated Protein Kinases (MAPK)/ Extracellular signal Regulated Kinase (ERK) signaling pathway [18]. In our study, history of trauma on hard palate was noted in two cases of pyogenic granuloma and hence trauma could be the main aetiological factor even for extra gingival pyogenic granuloma. Preventive measures to maintain oral hygiene are very important to avoid this type of lesions [4,13].
Age and sex wise distribution of the patients.
| Clinical forms of Pyogenic Granuloma cases n=21 |
|---|
| Age in yrs. | Gingival Pyogenic Granuloma (n=19) (90.48%) | Extra Gingival Pyogenic Granuloma (n=2) (9.52%) | Total (n=21) (100%) |
|---|
| Male(n=6) (31.57%) | Female (n=13) (68.42%) | Male(n=1)(50%) | Female (n=1) (50%) |
|---|
| 0-25 | 1 (16.66%) | 1 (7.69%) | 0 | 0 | 2 (14.28%) |
| 26-50 | 4 (66.66%) | 9 (69.23%) | 1 (50%) | 0 | 14 (66.66%) |
| 51-75 | 1 (16.66%) | 3 (23.07%) | 0 | 1 (50%) | 5 (19.047%) |
Distribution of the patients according to aetiological factors.
| Clinical forms of Pyogenic Granuloma cases n= 21 |
|---|
| Aetiological factors | Male7 (28.58%) | Female14 (71.42%) | Total(n=21) (100%) |
|---|
| Local factors | Plaque, calculus, crowding of teeth | 7 (100%) | 12 (85.71%) | 19 (90.47%) |
| Traumatic factors (Tooth brush trauma, toothpick trauma, sharp teeth) | 2 (28.57%) | 2 (14.28%) | 4 (19.04%) |
| Oral adverse habit | 3 (42.85%) | 1 (7.14%) | 4 (19.04%) |
| Hormonal disturbances | 0 | 14 (100%) | 14 (66.66%) |
Pearson Chi-Square Value=29.482, p-value=0.001 Significant
Most studies have shown that the gingiva is the most common location for pyogenic granuloma [1-6,10,15]. Present study found that out of 21 cases, 19 cases, (90.58%) were in gingiva and only two cases (9.52%) were found in extra gingival site that is on hard palate. In our study, almost equal distribution was noted in different segments of maxilla and mandible [Table/Fig-7]. Various studies also showed the same finding [14]. The size varies from a few millimeters to several centimeters. Smaller lesions located in anterior aspect of oral cavity where as bigger size of pyogenic granuloma located in the posterior segment of oral cavity. As in anterior region patient can notice the lesion immediately hence, the smaller size. Bigger size of pyogenic granuloma seen in posterior region as patients will not complain unless the discomfort occurs. Still as such reasons has not been justified about the size of pyogenic granuloma related to site but it can be correlated with the duration of lesion. In present study, out of 21 cases, 12 cases had pedunculated base as they arise from interdental gingiva whereas nine cases had sessile base and arised from broader surface of marginal gingiva. Hence, site from where it originated can be considered as a major factor for sessile and pedunculated base. In present study out of 21 cases, 13 cases had soft consistency and were erythematous in colour and eight cases had smooth surface covered by yellow fibrinous membrane. The naive lesions are highly vascular, often elevated and ulcerated, and bleed easily and it had soft consistency, whereas older lesions tend to be more collagenised and pink in appearance [6,13,14]. The colour varies from reddish to pink depending on the vascularity of the growth. They bleed readily when traumatised representing inflammation. Most of the cases in our study presented with the same features.
Clinical analysis of pyogenic granuloma according to site of involvement.
| Clinical forms of Pyogenic Granuloma cases n=21 |
|---|
| Sites | Maxillary Anterior5 (23.80%) | Maxillary Posterior4 (19.047%) | Mandibular Anterior4 (19.047%) | Mandibular Posterior6 (28.57%) | Hard Palate (Extra Gingival Form)2 (9.53%) | Total (n=21) (100%) |
|---|
| Labial/Buccal | 2 (40%) | 0 | 4 (100%) | 3 (50%) | | 9 (42.8%) |
| Lingual/Palatal | 1 (20%) | 4 (100%) | 0 | 2 (33.3%) | 2 (100%) | 9 (42.8%) |
| Both | 2 (40%) | 0 | 0 | 1 (16.6%) | | 3 (14.2%) |
| Pearson Chi-Square Value=36.067, p-value=0.001 Significant |
| SIZE |
| <2 cm | 4 (80%) | 1 (25%) | 2 (50%) | 2 (33.3%) | 1 (50%) | 10 (47.6%) |
| 2-4 cm | 1 (20%) | 2 (50%) | 2 (50%) | 1 (16.6%) | 1 (50%) | 7 (33.3%) |
| >4 cm | 0 | 1 (25%) | 0 | 3 (50%) | | 4 (38%) |
| Pearson Chi-Square Value=12.213, p-value=0.142 Non significant |
| BASE |
| Pedunculated | 1 (20%) | 3 (75%) | 3 (75%) | 5 (83.3%) | 0 | 12 (57.1%) |
| Sessile | 4 (80%) | 1 (25%) | 1 (25%) | 1 (16.6%) | 2 (100%) | 9 (42.8%) |
| Pearson Chi-Square Value=8.206, p-value=0.084 Non significant |
| SURFACE |
| Smooth | 2 (40%) | 2 (50%) | | 4 (66.6%) | | 8 (38%) |
| Lobulated | 1 (20%) | 2 (50%) | 1 (25%) | | | 4 (38%) |
| Ulcerative | | | 1 (25%) | 2 (33.3%) | | 3 (14.2%) |
| Granular | 2 (40%) | | 2 (50%) | | 2 (100%) | 6 (28.5%) |
| Pearson Chi-Square Value=19.367, p-value=0.080 Non significant |
| COLOUR |
| Erythematous | 3 (60%) | 2 (50%) | 4 (100%) | 2 (33.3%) | 2 (100%) | 13 (61.9%) |
| Pale pink | 2 (40%) | 2 (50%) | | 4 (66.6%) | | 8 (38%) |
| Pearson Chi-Square Value=6.017, p-value=0.198 Non significant |
| CONSISTENCY |
| Firm | 2 (40%) | 2 (50%) | | 4 (66.6%) | | 8 (38%) |
| Soft | 3 (60%) | 2 (50%) | 4 (100%) | 2 (33.3%) | 2 (100%) | 13 (61.9%) |
Pearson Chi-Square Value=6.017, p-value=0.198 Non significant
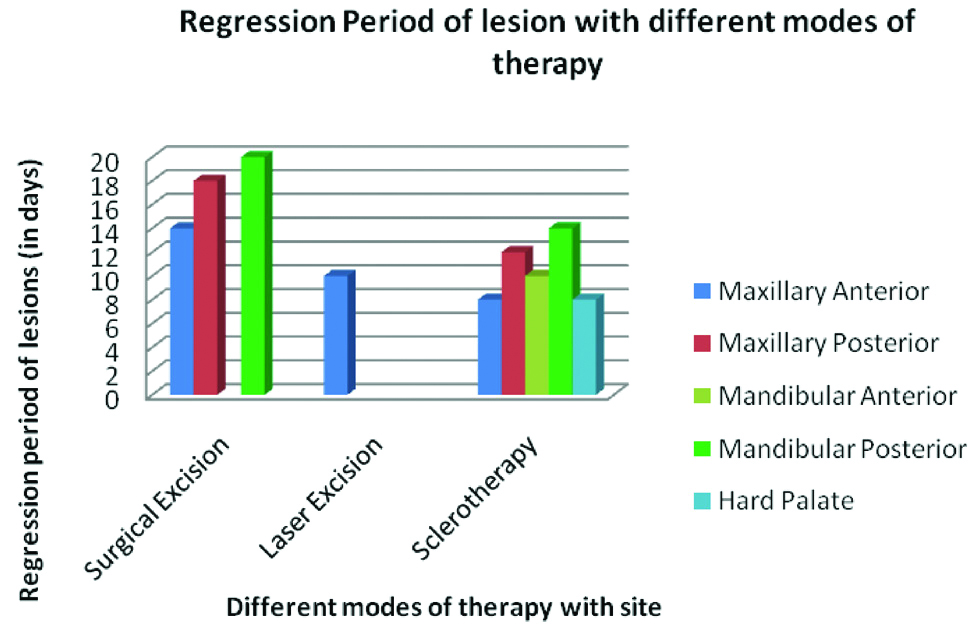
In present study, two cases of pyogenic granuloma of maxillary anterior region were treated by CO2 laser therapy and showed complete healing in 10-12 days as shown in [Table/Fig-8]. Because of easy accessibility in maxillary anterior region CO2 laser therapy is more preferable in small, firm and fibrotic pyogenic granuloma. Surgical excision was performed in seven cases and complete healing was noted in 12-15 days in anterior region and 15-20 days in posterior region. Because of larger size, posteriorly situated pyogenic granuloma took more days for complete healing. Not a single case treated by surgical excision showed any complication. Twelve cases including extra gingival pyogenic granuloma (two cases) were treated by sclerotherapy. Complete healing occurred within 7-8 days that is a shorter period as compared to surgical excision and laser surgery. Sclerotherapy uses the injection of a sclerosant (tissue irritants) which causes vascular thrombosis and endothelial damage leading to endofibrosis and vascular obliteration when injected into or adjacent to blood vessels [13,14]. Sclerotherapy has been reported to have the advantages of minimal scarring, little recurrence, and few complications in the treatment of pyogenic granuloma compared with other procedures [8-10].
Graph shows regression period of lesion with different modes of therapy.
Conclusion(s)
Pyogenic granuloma is a simple, benign reactive lesion of gingiva occurring at various sites in oral cavity. Successful result in treating pyogenic granuloma is obtained by considering various factors such as site, size and consistency of the lesion. Hence, selection of treatment modalities is very important for better prognosis. Sclerotherapy has more advantage as it is simple, minimally invasive, economical, and less time required for the lesion to heal completely.
Pearson Chi-Square Value=29.482, p-value=0.001 Significant
Pearson Chi-Square Value=6.017, p-value=0.198 Non significant
[1]. Mighell AJ, Robinson PA, Hume WJ, Immunolocalisation of tenascin-C in focal reactive overgrowths of oral mucosaJ Oral Pathol Med 1996 25:163-69.10.1111/j.1600-0714.1996.tb00214.x8809684 [Google Scholar] [CrossRef] [PubMed]
[2]. Neville BW, Damm DD, Allen CM, Bouquot JE, Oral and Maxillofacial Surgery 2002 2nd edPhiladelphiaSaunders:447-49. [Google Scholar]
[3]. Regezi JA, Sciubba JJ, Jordan RC, Oral Pathology: Clinical Pathological Considerations 2003 4th edPhiladelphiaWB Saunders:115-16. [Google Scholar]
[4]. Gomes SR, Shakir QJ, Thaker PV, Tavadia JK, Pyogenic granuloma of the gingiva: A misnomer? A case report and review of literatureJ Indian Soc Periodontol 2013 17(4):51410.4103/0972-124X.11832724174735 [Google Scholar] [CrossRef] [PubMed]
[5]. Jafarzadeh H, Sanatkhani M, Mohtasham N, Oral pyogenic granuloma: A reviewJ Oral Sci 2006 48(4):167-75.10.2334/josnusd.48.16717220613 [Google Scholar] [CrossRef] [PubMed]
[6]. Newadkar UR, Khairnar S, Dodamani A, Pyogenic granuloma: A clinicopathological analysis of fifty casesJ Oral Res Rev 2018 10:07-10.10.4103/jorr.jorr_21_17 [Google Scholar] [CrossRef]
[7]. Erbasar GN, Senguven B, Gultekin SE, Cetiner S, Management of a recurrent pyogenic granuloma of the hard palate with diode laser: A case reportJ Lasers Med Sci 2016 7(1):5610.15171/jlms.2016.1227330700 [Google Scholar] [CrossRef] [PubMed]
[8]. Khaitan T, Sinha R, Sarkar S, Kabiraj A, Ramani D, Sharma M, Conservative approach in the management of oral pyogenic granuloma by sclerotherapyJ Indian Acad Oral Med Radiol 2018 30:46-51.10.4103/jiaomr.jiaomr_15_18 [Google Scholar] [CrossRef]
[9]. Gilmore A, Kelsberg G, Safranek S, What’s the best treatment for pyogenic granuloma?J Fam Pract 2010 59(1) [Google Scholar]
[10]. Kamal R, Dahiya P, Puri A, Oral pyogenic granuloma: Various concepts of etiopathogenesisJournal of Oral and Maxillofacial Pathology 2012 16(1):7910.4103/0973-029X.9297822434943 [Google Scholar] [CrossRef] [PubMed]
[11]. Moon SE, Hwang EJ, Cho KH, Treatment of pyogenic granuloma by sodium tetradecyl sulfate sclerotherapyArch Dermatol 2005 141:644-46.10.1001/archderm.141.5.64415897398 [Google Scholar] [CrossRef] [PubMed]
[12]. Rahman H, Pyogenic granuloma successfully cured by sclerotherapy: A case reportJ Pak Assoc Dermatol 2014 24(4):361-64. [Google Scholar]
[13]. Patil SR, Maheshwari S, Khandelwal S, Wadhawan R, Somashekar SB, Deoghare A, Prevalence of reactive hyperplastic lesions of the gingiva in the Western Indian populationJ Orofac Sci 2014 6:41-45.10.4103/0975-8844.132585 [Google Scholar] [CrossRef]
[14]. Shadi S, Mahmoodabadi RZ, Danesh-Sani SA, Parviz M, Maryam E, Oral pyogenic granuloma: A retrospective analysis of 151 cases in an Iranian populationInt J Oral Maxillofac Pathol 2011 2(3):03-06. [Google Scholar]
[15]. Krishnapillai R, Punnoose K, Punnya V, Koneru A, Oral pyogenic granuloma-A review of 215 cases in a South Indian Teaching Hospital, Karnataka, over a period of 20 yearsOral Maxillofac Surg 2012 16:305-09.10.1007/s10006-012-0315-z22274762 [Google Scholar] [CrossRef] [PubMed]
[16]. Angelopoulos AP, Pyogenic granuloma of the oral cavity: Statistical analysis of its clinical featuresJ Oral Surg 1971 29:840-47. [Google Scholar]
[17]. Lawoyin JO, Arotiba JT, Dosumu OO, Oral pyogenic granuloma: A review of 38 cases from NigeriaBr J Oral Maxillofac Surg 1997 35:185-89.10.1016/S0266-4356(97)90561-1 [Google Scholar] [CrossRef]
[18]. Pereira TDSF, de Amorim LSD, Pereira NB, Vitório JG, Duarte-Andrade FF, Guimaräes LM, Oral pyogenic granulomas show MAPK/ERK signaling pathway activation, which occurs independently of BRAF, KRAS, HRAS, NRAS, GNA11, and GNA14 mutationsJ Oral Pathol Med 2019 00:01-05. [Google Scholar]